Abstract
Aim:
To investigate the effect of evodiamine (a quinolone alkaloid from the fruit of Evodia rutaecarpa) on the progression of Alzheimer's disease in SAMP8 and APPswe/PS1ΔE9 transgenic mouse models.
Methods:
The mice at age of 5 months were randomized into the model group, two evodiamine (50 mg·kg−1·d−1 and 100 mg·kg−1·d−1) groups and an Aricept (2 mg·kg−1·d−1) group. The littermates of no-transgenic mice and senescence accelerated mouse/resistance 1 mice (SAMR1) were used as controls. After 4 weeks of treatment, learning abilities and memory were assessed using Morris water-maze test, and glucose uptake by the brain was detected using positron emission tomography/computed tomography (PET/CT). Expression levels of IL-1β, IL-6, and TNF-α in brain tissues were detected using ELISA. Expression of COX-2 protein was determined using Western blot.
Results:
In Morris water-maze test, evodiamine (100 mg·kg−1·d−1) significantly alleviated the impairments of learning ability and memory. Evodiamine (100 mg·kg−1·d−1) also reversed the inhibition of glucose uptake due to development of Alzheimer's disease traits in mice. Furthermore, the dose of evodiamine significantly decreased the expression of IL-1β, IL-6, TNF-α, and COX-2 that were involved in the inflammation due to Alzheimer's disease.
Conclusion:
The results indicate that evodiamine (100 mg·kg−1·d−1) improves cognitive abilities in the transgenic models of Alzheimer's disease.
Similar content being viewed by others
Introduction
Alzheimer's disease (AD) is a progressive and irreversible neuro-degenerative disorder that leads to cognitive, memory and behavioral impairments. Brain regions involved in learning and memory processes, including the temporal and frontal lobes, are reduced in size in AD patients as the result of degeneration of synapses and death of neurons. The pathogenesis of AD is complex, and involves many molecular, cellular and physiological pathologies1. The 'amyloid cascade hypothesis' emphasizes a central role for amyloid beta-peptide (Aβ) in the pathogenesis of AD, and suggests that formation and aggregation of Aβ represent key features and possibly involve a triggering mechanism of AD. Based on the amyloid cascade hypothesis, Aβ has become a major therapeutic target2. However, amyloid plaques also accumulate during aging, and the stage of AD does not always correlate with the level of neuritic plaques3. Recently, it was reported that immunisation with Aβ42 resulted in clearance of amyloid plaques in AD patients, but this clearance did not prevent progressive neurodegeneration4. Accumulating evidence increasingly indicates that the inflammatory process is encountered in the pathology of AD. Examination of postmortem brains of AD patients has revealed an abundant presence of inflammatory mediators, such as pro-inflammatory cytokines and chemokines5, 6, 7. Epidemiological studies indicate that anti-inflammatory drug consumption can significantly reduce the risk of AD8.
Transgenic mice produced by crossing animals expressing mutant amyloid precursor protein and presenilin 1 (APPswe/PS1ΔE9) and senescence-accelerated mouse/prone 8 (SAMP8) transgenic mice mimic the AD phenotype via different mechanisms. The APPswe transgene encodes a mouse–human hybrid with the mouse sequence in the extracellular and intracellular regions and a human sequence within the Aβ domain with Swedish mutations K594N/M595L. The PS1ΔE9 transgene encodes the exon 9-deleted human presenilin-1. The APPswe/PS1ΔE9 double transgenic mice develop behavioral phenotypic and pathological features which make them useful as an AD model9. The senescence-accelerated mouse (SAM) is an accelerated aging model that was established through phenotypic selection from a common genetic pool of the AKR/J strain of mice. The SAMP8 mice show significant impairments in a variety of learning tasks, when compared with senescence accelerated mouse/resistance 1 (SAMR1) mice. Moreover, the abnormal APP and Aβ metabolism in the SAMP8 mice brain suggests that SAMP8 is not only a good model for studying age-related learning and memory deficits, but may also prove to be a useful model for studying Aβ-mediated effects in cognitive decline10, 11, 12.
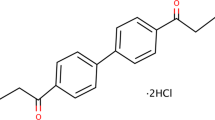
Chinese herbs have been and still are widely used as important remedies in Oriental medicine. Over recent years, a variety of biologically active constituents have been isolated from these sources. It is reported that tea polyphenol can reverse scopolamine- or D-galactose-induced deficits in cognitive abilities13, 14. Resveratrol acts to reduce pathological plaques in mice15, 16 and has anti-oxidant activity in vitro and in vivo16, 17. Evodiamine, a quinolone alkaloid, is a component isolated from the fruit of Evodia rutaecarpa, a traditional Chinese herb that has been used for treatment of headaches, abdominal pain, postpartum hemorrhage, dysentery and amenorrhea18, 19. However, the treatment of AD with evodiamine has not been reported. In the present study, we investigated the effect and the possible mechanisms of action of evodiamine in mouse models of AD.
Materials and methods
Animal models
The APPswe/PS1ΔE9 double-transgenic mouse in a C57BL/6J genetic background was bred in our laboratory. This mouse shows spatial memory deficits at 3 months of age and senile plaques in brain tissue at 4.5 months of age9. SAMP8 and SAMR1 mouse were obtained from the Department of Laboratory Animal Science, Peking University Health Science Center (Beijing, China). SAMR1 is one species of SAM, which shows normal aging characteristics. SAMP8 is a model of age-related dementia of the Alzheimer type and shows significant impairment in a variety of learning tasks10, 11, 12. All mice were maintained in an AAALAC-accredited facility and the use of animals was approved by the Animal Care and Use Committee of the Institute of Laboratory Animal Science of Peking Union Medical College (SCXK-2005-0013).
Groups and treatment
For screening of 12 herbal monomers, 5 month old transgenic mice were randomly divided into 13 groups (n=16 to 20 per group). One group was used as a vehicle control group and the remaining 12 groups were used for treatment with herbal monomers. The herbal monomers were purchased from Qingdao University Natural Product Institute (Qingdao, China). The littermates of non-transgenic mice were used as wild type (WT) controls. The WT and vehicle groups received a standard diet and the treated groups received a standard diet plus the respective monomers at the doses described in Table 1. The doses of 12 individual herbal monomers were selected based on human-equivalent dosages and data in previous reports13, 14, 16, 20. Morris water-maze tests were performed after 4 weeks of treatment, since this time period was believed sufficient for APPswe/PS1ΔE9 transgenic mice to show significant impairments in function when compared with WT mice.
For evodiamine analysis, APPswe/PS1ΔE9 and SAMP8 transgenic mice at 5 months of age were randomized into vehicle, evodiamine-Evo 50 (50 mg·kg−1·d−1), evodiamine-Evo 100 (100 mg·kg−1·d−1) and Aricept (2 mg·kg−1·d−1) groups. Aricept is an inhibitor of acetyl-cholinesterase and is presently used in long-term symptomatic treatments for patients with AD, since it enhances CNS levels of synaptic acetyl-choline. The administered does of Aricept was the human-equivalent dosage, calculated according to the weights of the mice. The littermates of no-negative mice and SAMR1 mice were used as WT controls. The mice were treated with standard diet or standard diet plus monomer for 4 weeks and their capacities for learning and memory were assessed by the Morris water-maze test.
Morris water-maze test
The protocol of the Morris water-maze test was modified from the reported methods21, 22, 23. Briefly, the apparatus included a pool with a diameter of 100 cm, filled with opaque water at 22–24 °C. An escape platform (15 cm in diameter) was placed 0.5 cm below the water surface. Two tests, constituting two blocks of trials, 60 s each, were performed daily for 5 consecutive days. The platform location and the animal starting point were held constant within each pair of daily tests, but they were changed from day to day. The mice were allowed to stay on the platform for 15 s before and after each trial. The time taken for an animal to reach the platform (latency period) was recorded. On the fifth day, a probe test was performed after the second daily trial; briefly, the platform was removed from the maze, and the number of crossings by the mice when the area from which the platform had been removed was recorded (for a maximal period of 60 s). Monitoring was performed with a video tracking system (Noldus Ltd, Ethovision XT, Holland). Results are represented as mean±SEM.
Histochemical analysis
The brain tissues from 6 month old animals were fixed in neutral buffered formalin. The tissues were dehydrated in an alcohol gradient then embedded in paraffin and sliced at 4 μm thickness. Thioflavin-S staining was performed on these slices24. After de-paraffinization and hydration, sections were washed in PBS and incubated in 2% potassium metabisulfite and 1% oxalic acid until they appeared white. The sections were then washed in water and stained for 10 min with a solution of 0.015% Thioflavin-S in 50% ethanol. Finally, the sections were washed in 50% ethanol and in water, then dried, and dipped in Histo-Clear before being cover-slipped with Permount. All chemicals were obtained from Sigma.
PET/CT images analysis
The PET/CT scan was modified from the reported method25. Briefly, mice from treated and positive and negative control groups were randomly chosen. They were anesthetized using 1.5% isoflurane, along with 31% O2 inhalation (flow rate: 2.5 L/min) through a nose cone prior to injection of the tracer. During operation, the body temperature of each mouse was maintained by a thermostat-controlled thermal heater; the mouse was imaged on a small-animal scanner (microPET/CT, Inveon, Siemens). Prior to the dynamic small-animal procedure, 18F-FDG tracer (FDG) (at ∼14.8–18.5 MBq) was injected as a bolus (∼200 μL) through a tail vein catheter and the animal was kept at room temperature for 45 min. FDG is a glucose analog that is actively transported into cells. Then the mouse was exposed to a 10-min PET scan, and a 10-min CT scan was obtained for attenuation correction of small-animal PET images. Images were reconstructed using the filtered back-projection algorithm with CT-based photon-attenuation correction26. The voxel size was 0.2×0.2×0.8 mm3. The field of view was 11.28×12.66 cm2.
ELISA
Mouse brain tissue was sampled and 100 mg of tissue per animal was homogenized in 1.0 mL of 0.9% NaCl solution containing 0.1% PMSF (Sigma, MO, USA). After centrifugation at 14 000 rpm for 15 min at 4 °C, the resulting supernatants were sampled in triplicate to detect the levels of IL-1β, IL-6, and TNF-α by an ELISA kit (R&D Systems and Invitrogen) according to the provided instructions.
Western blot
Mouse brain tissue was sampled and 100 mg of tissue per animal was homogenized in 1.0 mL of RIPA buffer containing 0.1% PMSF and 0.1% protease inhibitor cocktail (Sigma, MO, USA). After centrifugation at 14 000 round per minute for 15 min at 4 °C, the protein concentration in the resulting supernatants was detected by the BCA method. Aliquots of 60 μg per sample were subjected to 10% SDS-PAGE, followed by transfer onto a nitrocellulose membrane (Immobilon NC; Millipore, Molsheim, France). Immunoblotting was then carried out with antibodies specific for COX-2 at 1:100 dilution (Cayman Chemical, USA). Primary antibodies were visualized with anti-rabbit HRP-conjugated secondary antibodies (Santa Cruz) using a chemiluminescence detection system (Western Blotting Luminal Reagent, Santa Cruz). Sample loading was normalized with GAPDH. Bands were quantified by the densitometry function of the Quantity One software.
Statistical analyses
Statistical analyses were performed by one-way ANOVA followed by Tukey's Honestly Significantly Different (HSD) test. Data with a P<0.05 were deemed statistically significant. Results are expressed as mean±SEM.
Results
Comparative analysis of the effects of 12 different herbal monomers in APPswe/PS1ΔE9 transgenic mice
Twelve herbal monomers, that have varied effects on the CNS, microcirculation, anti-oxidative or anti-inflammatory responses, were selected to analyze their respective effects on cognitive abilities of APPswe/PS1ΔE9 transgenic mice. These herbal monomers and their usages are illustrated by Table 1, which shows their individual effects as evaluated by the Morris water-maze test. Only evodiamine showed the capacity to significantly improve cognitive abilities of APPswe/PS1ΔE9 transgenic mice, specifically referring to their spatial memory deficits at 3 months of age and the AD phenotype which progressively develops as the animals age.
Evodiamine treatment increased spatial learning and memory in SAMP8 and APPswe/PS1ΔE9 transgenic mice
To investigate the effect of evodiamine on AD models, it was used to treat both APPswe/PS1ΔE9 and SAMP8 transgenic mice at age of 5 months. In consideration of the welfare of the animals, administration of evodiamine was effected through oral administration via their diet. After 4 weeks of treatment, learning capacity and memory were assessed by the Morris water-maze test (Figure 1A–1D). During training d 1 the latency period in each group was approximately 40 s, and no significant differences were observed among the groups, over the five days of testing, during which performance of all five groups improved significantly in diminishing latency. On the third day of evodiamine treatment there was improvement in the behavior of the APPswe/PS1ΔE9 transgenic mice, evinced by decrease of latency by 35% (P<0.05, n=13) in the Evo 50 group and by 41% (P<0.05, n=17) in the Evo 100 group comparing the data with those of the vehicle group (Figure 1A). The probe trial in the Morris water-maze test on the day after the 5-day training showed that the number of crossings of the area from which the platform had been removed increased by 33% (P<0.05, n=17) in the Evo 100 group compared with the vehicle group (Figure 1B), and no significant differences were observed between Evo 50 group and vehicle groups. Evodiamine treatment also resulted in improvement in the behavior of the SAMP8 mice, evinced by a decrease in the latency period of 43% (P<0.05, n=12) (Figure 1C) and by a significantly increased number of crossings of the original platform area equivalent to 42% (P<0.05, n=12) in the Evo 100 group (Figure 1D), compared with observations for the vehicle group. Treatment with evodiamine at a dose of 50 mg·kg−1·d−1 showed no improvement in the behavior of the SAMP8 mice. Thus, the administration of the dose of 100 mg·kg−1·d−1 was significantly effective in improvement of behavior in both the SAMP8 and APPswe/PS1ΔE9 transgenic mouse models, which develop AD characteristics via different pathological mechanism9, 12.
Determination of the effect of evodiamine on mouse models of AD by the Morris water-maze test. The non-transgenic littermates (WT) and SAMR1 mice (R1) were given a standard diet and used as normal controls for APPswe/PS1ΔE9 and for SAMP8 mice, respectively. The APPswe/PS1ΔE9 and SAMP8 groups were given standard diet and used as normal vehicle controls (Vehicle). The APPswe/PS1ΔE9 and SAMP8 transgenic mice were treated with evodiamine at a dose of 50 mg·kg−1·d−1(Evo 50) or 100 mg·kg−1·d−1 (Evo 100) for 4 weeks. APPswe/PS1ΔE9 and SAMP8 transgenic mice were treated with Aricept at a dose of 2 mg·kg−1·d−1 in the same manner as for treatment with evodiamine and used as positive controls (Aricept). Latency during 5 d of the Morris water-maze tests and platform crossings on the day after the 5-d training period were tabulated for APPswe/PS1ΔE9 (A and B) and SAMP8 (C and D) transgenic mice. (bP<0.05, cP<0.01 vs vehicle group).
Evodiamine had no effect on Aβ deposition in the APPswe/PS1ΔE9 transgenic mouse
Since the dose of 100 mg·kg−1·d−1 was effective in both SAMP8 mice and APPswe/PS1ΔE9 mice, we used this dose to investigate whether evodiamine treatment would inhibit Aβ deposition in the APPswe/PS1ΔE9 transgenic mouse, which forms senile plaque in brain tissue after 6 months of age9. After 4 weeks of administration, hippocampus tissues were sampled from the WT, vehicle, Evo 100, and Aricept groups. Paraffin sections were prepared and stained with thioflavin-S medium. Observation using the fluorescence microscope showed that Aβ deposition clearly occurred in the APPswe/PS1ΔE9 transgenic mice compared with those in the WT control group. Neither evodiamine nor Aricept treatment showed observable inhibition of Aβ deposition in APPswe/PS1ΔE9 transgenic mice (Figure 2), suggesting that the effect of evodiamine on improvement of behavior in AD mouse models involves other mechanisms.
Evodiamine treatment has no effect on Aβ deposition in the brain of the APPswe/PS1ΔE9 transgenic mouse. After 4 weeks of administration, brain tissues from WT and vehicle mice, and mice treated with evodiamine at a dose of 100 mg·kg−1·d−1 (Evo 100) or with Aricept at a dose of 2 mg·kg−1·d−1 (Aricept) were utilized in standard pathological procedures and sections were stained with Thioflavin-S to visualize the deposition of Aβ. (Magnification×100).
Evodiamine treatment increased glucose uptake in brain tissue in the APPswe/PS1ΔE9 transgenic mouse
The AD patient exhibits large decreases in glucose uptake and energy metabolism in the frontal cortex and temporal lobes1. Brain glucose uptake was detected by PET scan in living mice of the WT, vehicle, Evo 100, and Aricept groups after 4 weeks of treatment (Figure 3A, 3B). The results showed that glucose uptake by APPswe/PS1ΔE9 transgenic mice was significantly decreased by 16% (P<0.05, n=3), compared with that of WT controls. Treatment with evodiamine ameliorated the glucose uptake decrease caused by APPswe/PS1ΔE9 expression by 16% (P<0.05, n=4). Aricept administration also improved glucose uptake in APPswe/PS1ΔE9 transgenic mice by 23% (P<0.05, n=3).
Evodiamine treatment increases glucose uptake in the brain of the APPswe/PS1ΔE9 transgenic mouse. After 4 weeks administration, the WT and Vehicle mice, and those treated with evodiamine at a dose of 100 mg·kg−1·d−1 (Evo 100) or Aricept at a dose of 2 mg·kg−1·d−1 (Aricept) were subjected to the PET/CT scan to obtain typical images as shown in panel A. Glucose (as FDG) uptake per gram of brain tissue is depicted in panel B (n=3–4). (bP<0.05 vs vehicle group).
Evodiamine treatment inhibited the expression of inflammatory cytokines in the APPswe/PS1ΔE9 transgenic mouse
Inflammatory factors IL-1β, IL-6, and TNF-α were detected with the ELISA in lysates of brain tissues from WT, vehicle, Evo 100 and Aricept groups after 4 weeks of treatment (Figure 4). The results indicated that evodiamine decreased the levels of IL-1β by 23% (P<0.05), IL-6 by 27% (P<0.05), and TNF-α by 26% (P<0.05), compared with their levels in the vehicle group. Aricept administration also significantly decreased the levels of IL-1β and IL-6, but not that of TNF-α.
Evodiamine treatment inhibits the expression of inflammatory cytokines in the APPswe/PS1ΔE9 transgenic mouse. After 4 weeks of administration, brain tissue from WT and Vehicle mice and those treated with evodiamine at a dose of 100 mg·kg−1·d−1 (Evo 100) or Aricept at a dose of 2 mg·kg−1·d−1 (Aricept) were sampled and total lysates were isolated. The levels of IL-1β (A, n=6), IL-6 (B, n=6), and TNF-α (C, n=6) were detected by ELISA kits. (bP<0.05 vs vehicle group).
Evodiamine treatment decreased the expression of COX-2 in the APPswe/PS1ΔE9 transgenic mouse
COX-2 is one of the important determinants in inflammatory response-mediated cytotoxicity. Accumulation of COX-2 protein was observed in the vehicle group, compared with WT mice, and the accumulation of COX-2 protein caused by expression of APPswe/PS1ΔE9 transgenic genes was significantly reduced by evodiamine, by up to 73% (P<0.01, n=4) and reduced by Aricept by up to 67% (P<0.01, n=4) after 4 weeks of treatment (Figure 5A, 5B).
Western blot analysis for COX-2 protein. Brain tissues from WT and Vehicle mice and those treated with evodiamine at a dose of 100 mg·kg−1·d−1 (Evo 100) or Aricept at a dose of 2 mg·kg−1·d−1 (Aricept) were sampled and total lysates were isolated. COX-2 levels were detected by Western blot, using GAPDH for normalization (A). The density of bands (B, n=4) was quantified by densitometry using the Bio-Rad Quantity One software. (cP<0.01 vs vehicle group). ND: not detected.
Discussion
In the present study we evaluated 12 herbal monomers in APPswe/PS1ΔE9 transgenic mice by the Morris water-maze test (Table 1). Evodiamine alone, from among the 12 herbal monomers, showed some effect on reversal of the AD phenotype through capacity to improve the cognitive abilities of the APPswe/PS1ΔE9 transgenic mice.
We first showed that 4 weeks of administration of evodiamine to the APPswe/PS1ΔE9 and SAMP8 transgenic mice improved spatial learning and memory of mice with symptoms of AD at 5 months of age (Figure 1). Our results indicate that evodiamine can improve spatial learning and memory in APPswe/PS1ΔE9 and SAMP8 transgenic mice, but that the improvement is not due to reduction in the pathological development of senile plaque in brain tissues (Figure 2). The perturbations in energy metabolism in the AD patient evinced by large decreases in glucose uptake and energy metabolism in the frontal cortex and temporal lobes27 are also present in the transgenic mouse model of AD (Figure 3). Evodiamine also significantly ameliorates the decrease in glucose uptake caused by APPswe/PS1ΔE9 expression (Figure 3), suggesting on this basis that treatment with evodiamine could contribute to improvement of brain function in the AD model.
Evodiamine has been shown to have various effects on biological processes, such as testosterone28 and catecholamine secretion29, as well as vasodilative30, anti-nociceptive31, obesity20, and thermoregulatory and uterotonic effects32. Evodiamine has anti-tumor potential through its ability to inhibit proliferation, induce apoptosis and reduce invasion and metastasis of a wide variety of tumor cells, including breast cancer, prostate cancer, leukemic T-lymphocyte, melanoma, cervical cancer, colon cancer and lung cancer cells33. Previous studies indicated that evodiamine represses COX-2 and inducible nitric oxide synthase (iNOS) expression and PGE2 release in RAW264.7 cells34 and inhibits LPS-induced NO production and iNOS up-regulation in microglial cells35, suggesting that evodiamine has anti-inflammatory activity. Our results demonstrated that evodiamine decreased the levels of IL-1β, IL-6, TNF-α and COX-2 protein, compared with levels in the vehicle group (Figures 4 and 5).
Examination of postmortem brains of AD patients reveals the abundant presence of inflammatory mediators, such as pro-inflammatory cytokines and chemokines, eg, IL-1, IL-6, TNF-α, MIP-1b, complement activation products, and oxygen radicals5, 6, 7. Inflammatory processes are present also in transgenic AD mouse models5, 6, 7. Our results indicated that evodiamine decreased the levels of IL-1β (Figure 4). IL-1 is reported to induce expression of AChE protein and mRNA and to increase AChE enzyme activity, and that such an effect exacebates cholinergic decline and dysfunction in AD36. Our results also indicated that evodiamine decreased the levels of IL-6 (Figure 4). IL-6 occurs normally at barely detectable levels in the adult CNS, and is strongly induced under pathological conditions37, 38. We found that evodiamine decreased the levels of TNF-α (Figure 4). TNF-α is a proinflammatory cytokine, the biological effects of which include stimulation of the acute-phase response, and cytotoxicity; furthermore, TNF-α stimulates IL-1 and IL-6 production, expression of adhesion molecules, and procoagulant activity39. In our studies evodiamine was shown to decrease the levels of COX-2 protein (Figure 5). COX-2 is an enzyme that plays a pivotal role in the arachidonate cascade leading to prostaglandin synthesis. Because the latter is so deeply intertwined with other inflammatory mechanisms, the inhibition of COX-2, with the attendant inhibition of prostaglandins, is a central target for anti-inflammatory therapy40. COX-2 mRNA and protein are considerably up-regulated in affected areas of the brain in AD. COX-2 helps mediate production of prostaglandins and other inflammatory factors, and it is itself up-regulated by pro-inflammatory mediators. For example, IL-1 and TNF-α are known to regulate COX-2 expression. Thus, this enzyme occupies a pivotal amplifying position for inflammatory reactions41, 42. Since evodiamine inhibits the expression of IL-1β, IL-6, TNF-α, and COX-2 protein, it may effect attenuation of CNS dysfunction in AD. However, the role of inflammation in the pathogenic process is still a matter of debate. One proposal is that the deposition of fibrillated Aβs in the human cortex could induce a local inflammatory reaction. Thus, neuro-inflammation is still considered to be a downstream consequence in the amyloid hypothesis, and inflammation has been considered as a secondary bystander response to neuronal degeneration and death3. Salminen et al43 indicate that increased production of amyloid-β oligomers can activate the innate immunity system via pattern-recognition receptors and evoke the pathology of AD. In addition, the pathology of AD seems be the outcome of the activation of innate immunologic defenses in the brain. Therefore, inflammation is not merely a bystander in neuro-degeneration but a powerful pathogenic force in the disease process.
The preponderance of our present findings suggests that evodiamine could alleviate impairment of learning abilities and memory and significantly improve the glucose uptake in the APPswe/PS1ΔE9 transgenic mice, and that the therapeutic effect of evodiamine was likely mediated through the inhibition of the inflammatory process, but not of senile plaque reduction. Our results suggest that evodiamine could have potential usage in treatment of AD.
Author contribution
Lian-feng ZHANG designed research; Shu-min YUAN perfermed research; Kai GAO contributed PET/CT images analysis; Xiong-zhi QUAN helped with Western blot analysis; Jiang-ning LIU helped with modifying figures; Chuan QIN, Dong-mei WANG, Chun-mei MA contributed pathological analysis; and Lian-feng ZHANG and Shu-min YUAN wrote the paper.
References
Mattson MP . Pathways towards and away from Alzheimer's disease. Nature 2004; 430: 631–9.
Hardy J, Selkoe DJ . The amyloid hypothesis of Alzheimer's disease: progress and problems on the road to therapeutics. Science 2002; 297: 353–6.
Eikelenboom P, Veerhuis R, Scheper W, Rozemuller AJ, van Gool WA, Hoozemans JJ . The significance of neuroinflammation in understanding Alzheimer's disease. J Neural Transm 2006; 113: 1685–95.
Holmes C, Boche D, Wilkinson D, Yadegarfar G, Hopkins V, Bayer A, et al. Long-term effects of Abeta42 immunisation in Alzheimer's disease: follow-up of a randomised, placebo-controlled phase I trial. Lancet 2008; 372: 216–23.
McGeer EG, McGeer PL . Inflammatory processes in Alzheimer's disease. Prog Neuropsychopharmacol Biol Psychiatry 2003; 27: 741–9.
Heneka MT, O'Banion MK . Inflammatory processes in Alzheimer's disease. J Neuroimmunol 2007; 184: 69–91.
Rojo LE, Fernandez JA, Maccioni AA, Jimenez JM, Maccioni RB . Neuroinflammation: implications for the pathogenesis and molecular diagnosis of Alzheimer's disease. Arch Med Res 2008; 39: 1–16.
Hayden KM, Zandi PP, Khachaturian AS, Szekely CA, Fotuhi M, Norton MC, et al. Does NSAID use modify cognitive trajectories in the elderly? The Cache County study. Neurology 2007; 69: 275–82.
Wang X, Liu P, Zhu H, Xu Y, Ma C, Dai X, et al. miR-34a, a microRNA up-regulated in a double transgenic mouse model of Alzheimer's disease, inhibits bcl2 translation. Brain Res Bull 2009; 80: 268–73.
Butterfield DA, Poon HF . The senescence-accelerated prone mouse (SAMP8): a model of age-related cognitive decline with relevance to alterations of the gene expression and protein abnormalities in Alzheimer's disease. Exp Gerontol 2005; 40: 774–83.
Miyamoto M . Characteristics of age-related behavioral changes in senescence-accelerated mouse SAMP8 and SAMP10. Exp Gerontol 1997; 32: 139–48.
Flood JF, Morley JE . Learning and memory in the SAMP8 mouse. Neurosci Biobehav Rev 1998; 22: 1–20.
Kim HK, Kim M, Kim S, Kim M, Chung JH . Effects of green tea polyphenol on cognitive and acetylcholinesterase activities. Biosci Biotechnol Biochem 2004; 68: 1977–9.
Lu JH, Guo J, Yang WH . Effects of green tea polyphenol on the behaviour of Alzheimer' s disease like mice induced by D-galactose and Abeta25-35 . Zhong Yao Cai 2006; 29: 352–4.
Marambaud P, Zhao H, Davies P . Resveratrol promotes clearance of Alzheimer's disease amyloid-beta peptides. J Biol Chem 2005; 280: 37377–82.
Karuppagounder SS, Pinto JT, Xu H, Chen HL, Beal MF, Gibson GE . Dietary supplementation with resveratrol reduces plaque pathology in a transgenic model of Alzheimer's disease. Neurochem Int 2009; 54: 111–8.
Sehirli O, Tozan A, Omurtag GZ, Cetinel S, Contuk G, Gedik N, et al. Protective effect of resveratrol against naphthalene-induced oxidative stress in mice. Ecotoxicol Environ Saf 2008; 71: 301–8.
Lee SH, Son JK, Jeong BS, Jeong TC, Chang HW, Lee ES, et al. Progress in the studies on rutaecarpine. Molecules 2008; 13: 272–300.
Wang L, Hu CP, Deng PY, Shen SS, Zhu HQ, Ding JS, et al. The protective effects of rutaecarpine on gastric mucosa injury in rats. Planta Med 2005; 71: 416–9.
Kobayashi Y, Nakano Y, Kizaki M, Hoshikuma K, Yokoo Y, Kamiya T . Capsaicin-like anti-obese activities of evodiamine from fruits of Evodia rutaecarpa, a vanilloid receptor agonist. Planta Med 2001; 67: 628–33.
Cox MM, Tucker AM, Tang J, Talbot K, Richer DC, Yeh L, et al. Neurobehavioral abnormalities in the dysbindin-1 mutant, sandy, on a C57BL/6J genetic background. Genes Brain Behav 2009; 8: 390–7.
Imbimbo BP, Hutter-Paier B, Villetti G, Facchinetti F, Cenacchi V, Volta R, et al. CHF5074, a novel gamma-secretase modulator, attenuates brain beta-amyloid pathology and learning deficit in a mouse model of Alzheimer's disease. Br J Pharmacol 2009; 156: 982–93.
Shiryaev N, Jouroukhin Y, Giladi E, Polyzoidou E, Grigoriadis NC, Rosenmann H, et al. NAP protects memory, increases soluble tau and reduces tau hyperphosphorylation in a tauopathy model. Neurobiol Dis 2009; 34: 381–8.
Bussiere T, Bard F, Barbour R, Grajeda H, Guido T, Khan K, et al. Morphological characterization of thioflavin-S-positive amyloid plaques in transgenic Alzheimer mice and effect of passive Abeta immunotherapy on their clearance. Am J Pathol 2004; 165: 987–95.
Yu AS, Lin HD, Huang SC, Phelps ME, Wu HM . Quantification of cerebral glucose metabolic rate in mice using 18F-FDG and small-animal PET. J Nucl Med 2009; 50: 966–73.
Chow PL, Rannou FR, Chatziioannou AF . Attenuation correction for small animal PET tomographs. Phys Med Biol 2005; 50: 1837–50.
Blass JP . Brain metabolism and brain disease: is metabolic deficiency the proximate cause of Alzheimer dementia? J Neurosci Res 2001; 66: 851–6.
Lin H, Tsai SC, Chen JJ, Chiao YC, Wang SW, Wang GJ, et al. Effects of evodiamine on the secretion of testosterone in rat testicular interstitial cells. Metabolism 1999; 48: 1532–5.
Yoshizumi M, Houchi H, Ishimura Y, Hirose M, Kitagawa T, Tsuchiya K, et al. Effect of evodiamine on catecholamine secretion from bovine adrenal medulla. J Med Invest 1997; 44: 79–82.
Chiou WF, Chou CJ, Shum AY, Chen CF . The vasorelaxant effect of evodiamine in rat isolated mesenteric arteries: mode of action. Eur J Pharmacol 1992; 215: 277–83.
Kobayashi Y . The nociceptive and anti-nociceptive effects of evodiamine from fruits of Evodia rutaecarpa in mice. Planta Med 2003; 69: 425–8.
King CL, Kong YC, Wong NS, Yeung HW, Fong HH, Sankawa U . Uterotonic effect of Evodia rutaecarpa alkaloids. J Nat Prod 1980; 43: 577–82.
Jiang J, Hu C . Evodiamine: a novel anti-cancer alkaloid from Evodia rutaecarpa. Molecules 2009; 14: 1852–9.
Liu YN, Pan SL, Liao CH, Huang DY, Guh JH, Peng CY, et al. Evodiamine represses hypoxia-induced inflammatory proteins expression and hypoxia-inducible factor 1alpha accumulation in RAW264.7. Shock 2009; 32: 263–9.
Ko HC, Wang YH, Liou KT, Chen CM, Chen CH, Wang WY, et al. Anti-inflammatory effects and mechanisms of the ethanol extract of Evodia rutaecarpa and its bioactive components on neutrophils and microglial cells. Eur J Pharmacol 2007; 555: 211–7.
Li Y, Liu L, Kang J, Sheng JG, Barger SW, Mrak RE, et al. Neuronal-glial interactions mediated by interleukin-1 enhance neuronal acetylcholinesterase activity and mRNA expression. J Neurosci 2000; 20: 149–55.
Vallieres L, Rivest S . Regulation of the genes encoding interleukin-6, its receptor, and gp130 in the rat brain in response to the immune activator lipopolysaccharide and the proinflammatory cytokine interleukin-1beta. J Neurochem 1997; 69: 1668–83.
Gruol DL, Nelson TE . Physiological and pathological roles of interleukin-6 in the central nervous system. Mol Neurobiol 1997; 15: 307–39.
Baert FJ, D'Haens GR, Peeters M, Hiele MI, Schaible TF, Shealy D, et al. Tumor necrosis factor alpha antibody (infliximab) therapy profoundly down-regulates the inflammation in Crohn's ileocolitis. Gastroenterology 1999; 116: 22–8.
Akiyama H, Barger S, Barnum S, Bradt B, Bauer J, Cole GM, et al. Inflammation and Alzheimer's disease. Neurobiol Aging 2000; 21: 383–421.
O'Banion MK, Miller JC, Chang JW, Kaplan MD, Coleman PD . Interleukin-1 beta induces prostaglandin G/H synthase-2 (cyclooxygenase-2) in primary murine astrocyte cultures. J Neurochem 1996; 66: 2532–40.
Yamamoto K, Arakawa T, Ueda N, Yamamoto S . Transcriptional roles of nuclear factor kappa B and nuclear factor-interleukin-6 in the tumor necrosis factor alpha-dependent induction of cyclooxygenase-2 in MC3T3-E1 cells. J Biol Chem 1995; 270: 31315–20.
Salminen A, Ojala J, Kauppinen A, Kaarniranta K, Suuronen T . Inflammation in Alzheimer's disease: amyloid-beta oligomers trigger innate immunity defence via pattern recognition receptors. Prog Neurobiol 2009; 87: 181–94.
Acknowledgements
The present work was supported in part by the Ministry of Health Foundation (No 200802036) and the National Science and Technology Major Projects (No 2009ZX09501-026).
The authors appreciate that Dr JAMES improved the expression of English and the figures.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Yuan, Sm., Gao, K., Wang, Dm. et al. Evodiamine improves congnitive abilities in SAMP8 and APPswe/PS1ΔE9 transgenic mouse models of Alzheimer's disease. Acta Pharmacol Sin 32, 295–302 (2011). https://doi.org/10.1038/aps.2010.230
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2010.230
Keywords
This article is cited by
-
Evodiamine Relieve LPS-Induced Mastitis by Inhibiting AKT/NF-κB p65 and MAPK Signaling Pathways
Inflammation (2022)
-
Low-dose pioglitazone can ameliorate learning and memory impairment in a mouse model of dementia by increasing LRP1 expression in the hippocampus
Scientific Reports (2019)
-
Protective effects of evodiamine in experimental paradigm of Alzheimer’s disease
Cognitive Neurodynamics (2018)
-
Development and Validation of a Rapid and Specific UHPLC–MS/MS Method for Simultaneous Determination of 21 Bioactive Components in Tiantai No. 1 Pill and Rat Plasma
Chromatographia (2018)
-
A promising antitumor activity of evodiamine incorporated in hydroxypropyl-β-cyclodextrin: pro-apoptotic activity in human hepatoma HepG2 cells
Chemistry Central Journal (2016)