Abstract
Aim:
To investigate the effect of N-benzyl-5-phenyl-1H-pyrazole-3-carboxamide (BPC) on angiogenesis in human umbilical vein endothelial cells (HUVECs).
Methods:
Capillary-like tube formation on matrigel and cell migration analyses were performed in the absence of serum and fibroblast growth factor (FGF-2). Reactive oxygen species (ROS) were measured using a fluorescent probe, 2′, 7′- dichlorodihydrofluorescein (DCHF). The nitric oxide (NO) production of HUVECs was examined using a NO detection kit. Morphological observation under a phase contrast microscope, a viability assay using 3-[4, 5-dimethylthiazol-2-yl]-2, 5-diphenyl-tetrazolium (MTT) and a lactate dehydrogenase (LDH) activity analysis by a detection kit were performed to evaluate the toxicity of BPC on HUVECs in the presence of serum and FGF-2. The level of hypoxia-inducible factor 1α (HIF-1α) and the release of vascular endothelial growth factor (VEGF) were measured by Western blot and ELISA, respectively.
Results:
In the absence of serum and FGF-2, cells treated with BPC (5-20 μmol/L) rapidly aligned with one another and formed tube-like structures within 12 h. In the presence of serum and FGF-2, cells treated with BPC for 24, 48 and 72 h had no changes in morphology, viability or LDH release compared with the control group. Cell migration in the BPC-treated group was significantly increased compared with the control group. During this process, NO production and ROS level were elevated dramatically, and the levels of HIF-1α and VEGF were increased dependent on the generation of ROS.
Conclusion:
BPC most effectively promoted angiogenesis and migration in HUVECs in the absence of FGF-2 and serum.
Similar content being viewed by others
Introduction
More and more people are suffering from chronic ischemic diseases. Ischemia, defined as the insufficiency or even loss of blood flow to an organ, occurs as a result of various pathologies associated with vascular obstruction or disruption. These can include myocardial infarction, stroke and pulmonary embolism1. Newly formed blood vessels provide a route for supplying metabolic requirements such as nutrients, growth factors and oxygen to the site of hypoxic or ischemic tissues and organs affected by defective blood circulation and functionally improve ischemia-associated tissue damage and injury2.
The pyrazole unit is a core structure in a number of natural products. Pyrazole derivatives are known to exhibit a wide range of biological properties. It has been widely reported that pyrazole derivatives could inhibit cell proliferation and promote cell apoptosis. In our laboratory, several pyrazole derivatives have been synthesized. We found that 1-arylmethyl-3-aryl-1H-pyrazole-5-carbohydrazide hydrazone derivatives could suppress A549 lung cancer cell growth3, 1-(2′-hydroxy-3′-aroxypropyl)-3-aryl-1H-pyrazole-5-carbohydrazide derivatives induced A549 cell autophagy4 and ethyl 3-(o-chlorophenyl)-5-methyl-1-phenyl-1H-pyrazole-4-carboxylate inhibited human umbilical vein endothelial cell (HUVEC) apoptosis5. Nevertheless, no reports about the effects of multi-substituted pyrazole derivatives on the angiogenesis of vascular endothelial cells have yet been documented.
In our previous papers, we synthesized a series of pyrazole derivatives and obtained their crystal structures6, 7, 8, 9. After screening, we identified N-benzyl-5-phenyl-1H-pyrazole-3-carboxamide (BPC) as a proangiogenic agent (Figure 1). Reactive oxygen species (ROS) and nitric oxide (NO) played important roles in angiogenesis. It was reported that ROS regulated angiogenesis and tumor growth through hypoxia-inducible factor 1α (HIF-1α) and vascular endothelial growth factor (VEGF)10. However, little is known about the ROS-HIF-1α-VEGF pathway in angiogenesis under ischemic conditions. Our current results show that BPC could effectively induce angiogenesis by increasing ROS and NO when deprived of FGF-2 and serum and that ROS regulates angiogenesis through HIF-1α and VEGF. The data reveal that BPC (5 μmol/L) exhibits protective proangiogenic properties. This suggests that BPC may represent a promising strategy for treating ischemic diseases.
Materials and methods
Materials
HUVECs were obtained in our laboratory using the method of Jaffe et al11. Fetal bovine serum (FBS) was purchased from Hyclone Lab (USA). M199 medium was purchased from Gibco (USA). Matrigel was purchased from BD Biosciences (USA). The NO detection kit and LDH kit were purchased from Nanjing Jiancheng Bioengineering Institute (China). A fluorescent probe, 2′,7′-dichlorodihydrofluorescein (DCHF) was obtained from Sigma-Aldridch (USA). Chemicals including dimethyl sulfoxide (DMSO), 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl-tetrazolium (MTT), N-acetyl-L-cysteine (antioxidant and free radical scavenger, NAC) and protease inhibitor cocktail were obtained from Sigma-Aldrich (St Louis, MO). All other chemicals were purchased from original sources and were of superior grade and purity.
Cell culture
HUVECs were cultured in M199 medium supplemented with 20% fetal bovine serum and FGF-2 (70 ng/mL) in a humidified incubator at 37 °C with 5% CO2. The medium was refreshed on every second day. The experiments were performed on cells with a population doubling level (PDL) of 5–10.
Exposure of HUVECs to BPC
When the cultures of HUVECs reached sub-confluency, the medium was replaced with basal M199 medium (without serum and FGF-2) after one wash with the same medium. The cells were then treated in two ways: (a) cells deprived of serum and FGF-2 were cultured in basal M199 medium with DMSO [<0.1% (v/v)] (control group) and (b) cells cultured in basal M199 medium (without serum and FGF-2) were treated with 5, 10, 20, or 40 μmol/L BPC (test group). BPC was dissolved in DMSO and applied to cells such that the final concentration of DMSO in the culture medium was below 0.1% (v/v). DMSO at a concentration of 0.1% (v/v) does not affect cell viability. The morphological changes of cells were observed under a phase contrast microscope (Nikon, Japan) at 24, 48, and 72 h. To further investigate the roles of ROS in this process, we treated the cells with NAC (10 mmol/L) to depress the levels of ROS12.
Cell viability assay
HUVECs were plated in 96-well cell culture plates. When the cultured cells became sub-confluent, they were washed once with basal M199 medium. Then the cells were treated with 5, 10, or 20 μmol/L of BPC in the presence of serum and FGF-2. At 24, 48, and 72 h, cell viability was determined by MTT assay, as described previously13. The viability was calculated as: percent=(OD of treated group/OD of control group)×100.
Lactate dehydrogenase (LDH) assay
An LDH assay was performed on the cells treated with BPC for 48 h using an LDH kit according to the manufacturer's protocol. LDH catalyzes the reduction of pyruvate to L-lactate with a concomitant oxidation of NADH2 to NAD. Because the oxidation of NADH2 is directly proportional to the reduction of pyruvate in equimolar amounts, LDH activity can be calculated from the rate of decrease in absorbance at 440 nm14. Light absorption was measured with a Cintra 5 UV-vis spectrometer (GBC, Australia), and LDH activity was calculated as follows:
LDH (U/L)=(ΔAsample/min–ΔAblank/min )×F
F=1000×Vtotal/(Vsample×extinction coefficient); where ΔA= change in absorbance, min=minute, V=volume in mL and extinction coefficient=mmol absorptivity of NADH at 440 nm (which was 6.3).
Capillary-like tube formation assay
The formation of vascular-like structures in HUVECs was assessed by growth-factor-reduced Matrigel as previously described15. HUVECs were seeded on 24-well plates coated with Matrigel at 4×104−5×104 cells/well in basal M199 medium and incubated at 37 °C for 1 h. Cells were treated with or without 5, 10, or 20 μmol/L BPC in the absence of FGF-2 and serum, then incubated at 37 °C for 12 h. Tube formation was observed with an inverted-phase contrast microscope (Nikon, Tokyo, Japan) at 2, 4, and 8 h. The degree of tube formation was quantified by measuring the length of tubes in random fields from each well using the National Institutes of Health (NIH) Image Program.
Cell migration assay
The cell migration assay was performed as described previously16, 17. Cells were seeded on 24-well plates. When cells reached a post-confluent state, wounds of a 1 mm width were created by scraping the cell monolayer with a sterile pipette tip. Cells were treated with 5, 10, or 20 μmol/L BPC in the absence of FGF-2 and serum, then incubated at 37 °C for 24 h. Migration was documented by photos taken immediately after scraping. Cell migration was quantified by measuring the distance between the wound edges at 0, 12, and 24 h using the NIH Image Program.
NO production assay
HUVECs were treated as described above for 3, 6, and 12 h. Then 100 μL of culture solution was used for the NO assay. NO production was detected with a NO detection kit following the manufacturer's protocol. The optical density was measured at a wavelength of 550 nm. NO production was expressed as μmol/L.
Intracellular ROS assay
HUVECs were treated as described above for 3, 6, and 12 h. Intracellular ROS levels were measured using a fluorescent probe, 2′,7′-dichlorodihydrofluorescein (DCHF) (Sigma), which could be rapidly oxidized into the highly fluorescent 2′,7′-dichlorofluorescein (DCF) in the presence of intracellular ROS18. Fluorescence was monitored with a laser scanning confocal microscope (Leica, Germany) using an excitation wavelength of 488 nm. The amount of ROS was quantified as the relative fluorescence intensity of DCF per cell in the scan area.
VEGF release assay
HUVECs were treated as described above for 3, 6, and 12 h. The culture supernatants were collected and the level of VEGF in the culture media was quantified using a commercially available ELISA kit (R&D, USA) according to the manufacturer's instructions. The optical density was measured at a wavelength of 450 nm.
Western blot analysis
Cells with various treatments were lysed in lysis buffer containing 25 mmol/L Tris-HCl (pH 6.8), 2% SDS, 6% glycerol, 1% 2-mercaptoethanol, 2 mmol/L PMSF, 0.2% bromophenol blue and a protease inhibitor cocktail for 10 min at room temperature and boiled for another 10 min. Protein concentration was determined by Coomassie brilliant blue protein assay. Equal amounts of total protein (40 mg) were separated with 15% SDS-PAGE and were electroblotted onto polyvinylidene difluoride membranes. The membrane was blocked with 5% (w/v) nonfat dry milk in PBS–Tween 20 (0.05% PBST) for 1 h and incubated with anti-HIF-1α and anti-GAPDH antibodies (1/1000) at 4–8 °C overnight. After washing in TBST and TBS, the membrane was incubated with appropriate horseradish peroxidase-conjugated secondary antibodies (1/5000) for 1 h at room temperature. The immunoreactive bands were chromogenously developed with 3,30-diaminobenzidine. GAPDH was used as a loading control. The relative quantity of proteins was analyzed by use of Quantity One software (Bio-Rad, Hercules, CA). HIF-1α levels were measured relative to the loading control (GAPDH). The densitometric analysis of HIF-1α levels, from experiments performed at least in triplicate, was shown relative to GAPDH levels.
Statistical analyses
Data were expressed as the means±SEM. (n>3) and analyzed by t-test. Differences at P<0.05 and P<0.01 were considered statistically significant and dramatically significant, respectively.
Results
Effects of BPC on endothelial cell morphology in the absence and presence of serum and FGF-2
When deprived of serum and FGF-2, HUVECs gradually detach from the dish and undergo apoptosis. This is an in vitro model commonly used to mimic the in vivo ischemic condition19. In this study, we screened proangiogenic agents using this model of the ischemic condition. When deprived of serum and FGF-2 for 48 h, cells treated with BPC were elongated and formed capillary-like structures in morphology compared with control cells (Figure 2A).
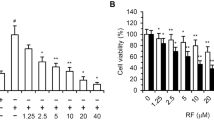
Effects of BPC on endothelial cells in the absence and presence of serum and FGF-2. (A) Cell morphological micrographs were obtained under a phase contrast microscope at 24, 48 and 72 h (×200). In the control group (Ctrl), cells were cultured in basal M199 medium (without serum and FGF-2) with DMSO [<0.1% (v/v)]. In the experimental groups, cells were treated with 5 (d-f), 10 (g-i), 20 (j-l), or 40 (m-o) μmol/L BPC. (B) Cell morphological micrographs obtained under a phase contrast microscope at 24, 48 and 72 h (×200). In the control group (Ctrl), cells were cultured in M199 medium with DMSO [<0.1% (v/v)]. In the experimental groups, cells were treated with 5 (d-f), 10 (g-i), or 20 (j-l) μmol/L BPC. (C) Cell viability was determined using MTT assay at 24, 48 and 72 h in the presence of serum and FGF-2 (n=3). (D) LDH assay was performed on cells treated as described in the text for 48 h in the presence of serum and FGF-2 (n=3).
To investigate the toxicity of BPC on HUVECs under normal conditions, we examined the morphology, viability and LDH activity of HUVECs treated with BPC in the presence of serum and FGF-2. The results showed no morphological changes among these groups at each time point (Figure 2B). In addition the MTT assay showed that under normal conditions, cell viability was not affected (Figure 2C). As shown in Figure 2D, the release of LDH from HUVECs was not increased by BPC. The data showed that BPC was not toxic to cells under normal conditions.
BPC induces endothelial cell differentiation into capillary-like tube structures in vitro
To demonstrate the proangiogenic function of BPC on HUVECs, we performed a capillary-like tube formation assay on Matrigel. Capillary-like tubes developed in HUVECs treated with BPC (5, 10, or 20 μmol/L) on Matrigel-coated 24-well plates with basal M199 medium at 2, 4, and 8 h. At the early stage, HUVECs could not differentiate towards capillary-like tube structures without BPC. In the presence of BPC, the cells rapidly aligned with one another and formed tube-like structures within 12 h (Figure 3). BPC (5 μmol/L) significantly promoted the capillary-like tube formation compared with control at 8 h (P<0.01) (Figure 3B).
BPC induced endothelial cell differentiation into capillary-like structures in vitro. (A) BPC promoted vascular structure formation in an in vitro Matrigel assay without FGF-2 and serum (×200). HUVECs were seeded without BPC (a-c) and with BPC (d-l) for 2, 4, and 8 h. (B) Quantitative assessment of the extent of tube formation (bP<0.05, cP<0.01 vs Ctrl, n=5).
BPC promotes migration of endothelial cells in vitro
Migration of endothelial cells plays an importnat role in angiogenesis20. To examine the effect of BPC on cell migration, we performed the cell monolayer wound healing assay. As shown in Figure 4, cells without BPC treatment showed little migratory capacity at the 12 and 24 h time points. Cell migration in the BPC treated group was significantly increased compared with control (P<0.05, P<0.01). BPC at 5 μmol/L promoted cell migration most effectively (Figure 4B).
BPC promotes migration of endothelial cells in vitro. BPC induced HUVEC migration in the absence of FGF-2 and serum (200×). (A) Representative photomicrographs of migration. Cells migrated in FGF-2 and serum-free medium at 0, 12, and 24 h in the absence (a-c) and presence of BPC (d-l). (B) Quantitative assessment of migration distance (bP<0.05, cP<0.01 vs Ctrl, n=4).
BPC enhances ROS levels and intracellular NO generation
ROS plays an important role in modulating angiogenesis. We detected the levels of intracellular ROS in the cells treated as described above at 3, 6, and 12 h. As shown in Figure 5A, the level of ROS in cells treated with BPC increased in a dose-dependent manner at 6 and 12 h (P<0.05, P<0.01). After incubation with NAC, the cells did not differentiate towards a capillary-like tube structure compared with those not treated with NAC 10 mmol/L (Figure 5C), but ROS levels were effectively depressed (data not shown).
BPC induces angiogenesis through increase in ROS and NO. (A) An intracellular ROS assay was performed on the cells treated with BPC 5–20 μmol/L for 3, 6, and 12 h (×200). Relative DCF fluorescence reflected the intensity of ROS in Ctrl and BPC groups. (B) Quantitative assessment of ROS levels using relative fluorescence intensity of DCF per cell in the scan. bP<0.05, cP<0.01 vs Ctrl. (C) NAC inhibited angiogenesis induced by BPC (×200). (D)The change of NO production in cells treated with BPC 5–20 μmol/L for 3, 6, and 12 h. bP<0.05, cP<0.01 vs Ctrl, n = 3. (E) NO increase was not affected by NAC 10 mmol/L. Ctrl cells were cultured in M199 medium with DMSO. BPC cells were treated with 10 μmol/L BPC (cP<0.01 vs ctrl, n=3).
It is well known that NO participates in multiple events in HUVECs, including differentiation and migration. NO production was examined after treatment with BPC for 3, 6, and 12 h. The results showed that NO production of HUVECs treated with BPC was altered significantly at 3 and 6 h (P<0.05, P<0.01) (Figure 5D). To further analyze the relationship between ROS and NO, we examined NO production after incubation with NAC 10 mmol/L. The results showed that NO generation was not affected (Figure 5E).
BPC enhanced the HIF-1α level and VEGF release depending on the generation of ROS
VEGF plays a major role in the induction of angiogenesis and is transcriptionally regulated by HIF-1 in response to hypoxia21. In previous studies, endogenous ROS levels could regulate HIF-1α expression22. In this study, HIF-1α was increased after BPC treatment. However, HIF-1α expression was inhibited when NAC was used to eliminate ROS (Figure 6A, 6B). The results indicate that HIF-1α expression depends on the generation of cellular ROS.
BPC enhanced HIF-1α levels and VEGF release dependent on the generation of ROS. (A) BPC-enhanced HIF-1α expression was inhibited by NAC 10 mmol/L at 6 h. (B) Bar graph plots of relative HIF-1α levels (bP<0.05, cP<0.01 vs Ctrl. fP<0.01 vs 10 μmol/L BPC; n=3). (C) BPC enhanced VEGF release. In the control group (Ctrl), cells were cultured in M199 medium with DMSO [<0.1% (v/v)]. In the experimental groups, cells were treated with BPC at 5, 10, or 20 μmol/L. (bP<0.05, cP<0.01 vs Ctrl. n=3). (D) BPC-enhanced VEGF release was inhibited by NAC 10 mmol/L. Ctrl cells were cultured in M199 medium with DMSO [<0.1% (v/v)]. BPC cells were treated with 10 μmol/L BPC (bP<0.05 vs Ctrl. eP<0.05 vs 10 μmol/L BPC; n=3).
After treatment with BPC, we examined VEGF levels using ELISA. As shown in Figure 6C, the release of VEGF was enhanced by BPC. To test whether ROS affected VEGF release, we used NAC to eliminate ROS. The results show that the release of VEGF was inhibited when ROS levels were depressed (Figure 6D).
Discussion
Angiogenesis generally refers to the growth of microvessels that sprouts the size of capillary blood vessels23. It plays a critical role in both physiological processes, such as wound healing, embryological development and the menstrual cycle, and the pathogenesis of various diseases, such as cancer, diabetic retinopathy and rheumatoid arthritis24, 25. In the last century, emerging evidence suggested that angiogenesis may be an ideal strategy to treat ischemic diseases. The promotion of angiogenesis facilitates various physiological processes and the treatment of diseases including inflammatory diseases, cardiac ischemia, peripheral vascular diseases and myocardial infarction. In our study, pyrazole derivatives were synthesized and screened. We identified BPC as a proangiogenic agent in the absence of serum and FGF-2. Our data showed that BPC at 5 μmol/L could effectively induce endothelial cell angiogenesis in the absence of FGF-2 and serum. The identification of BPC may contribute to further work in the development of a potential drug for treating ischemic diseases.
ROS generated by endothelial cells include superoxide and hydroxyl, nitric oxide (NO) and non-radical species such as hydrogen peroxide (H2O2)24. Accumulating evidence suggests that high levels of ROS could act as signaling molecules to mediate various growth-related responses, including angiogenesis. It has been reported that VEGF (vascular endothelial growth factor) and angiopoietin-1 (Ang1), two angiogenic growth factors, induce EC migration through an increase in ROS13, 26. Recently, Zhao et al reported that ROS promote the formation of new vessels in the infracted heart and contribute to cardiac repair25. In our study, BPC promoted HUVEC angiogenesis, while ROS were significantly increased. VEGF is considered to be the most important growth factor involved in angiogenesis, which is mainly regulated by HIF-1 in response to hypoxia. HIF-1 is a heterodimeric basic helix-loop-helix transcription factor composed of HIF-1α and HIF-1β subunits22. It has been reported that endogenous ROS levels could regulate HIF-1α and VEGF expression to induce angiogenesis in ovarian cancer cells10. However, the role of the ROS-HIF-1α-VEGF pathway in angiogenesis under ischemic conditions remains to be defined. Our results showed that the levels of HIF-1α and VEGF were modulated by ROS during this process. It suggests that BPC promotes angiogenesis through the ROS-HIF-1α-VEGF pathway.
Nitric oxide (NO) is a short-lived free radical that acts as a small biological molecule and exists extensively in the body. NO, a highly diffusible intercellular signaling molecule with a wide range of biological effects, is generated by nitric oxide synthase (NOS), which catalyzes the conversion of L-arginine to L-citrulline27. Since it was discovered 20 years ago, NO has been found to play an important role in angiogenesis and in the nervous and immune systems. The release of NO is of great importance for regulating endothelial cell function during vasodilatation, vascular remodeling and angiogenesis28. It has been reported that NO is required in VEGF-induced angiogenesis in HUVECs29. Our results showed that BPC increased the release of NO in this process. NO may act as an important modulator in BPC-induced angiogenesis.
Pyrazole compounds can act as inhibitors and cytotoxic agents. It has been reported that 4′-(6,7-disubstituted-2,4-dihydro-indeno [1,2-c]pyrazol-3-yl)-biphenyl-4-ol can act as a potent Chk1 inhibitor and that the pyrazole-based compound could inhibit the activity of heat shock protein 9030, 31. In our present study, we found that BPC was not toxic to endothelial cells under normal conditions. Furthermore, BPC could effectively induce endothelial cell angiogenesis in the absence of serum and FGF-2. These data reveal that BPC, with its remarkable biological properties and no toxic properties, exhibits exceptional characteristics among the multitudinous pyrazole compounds. This suggests that BPC could be practically used in clinical trials.
In summary, the results of this study showed that BPC could induce HUVEC angiogenesis and promote migration in the absence of FGF-2 and serum in vitro. The results also revealed that 5 μmol/L BPC significantly promoted angiogenesis and migration. Angiogenesis induced by BPC was mediated by the ROS-HIF-1α-VEGF and NO signal pathways. Moreover, in the presence of FGF-2 and serum, BPC did not affect cell morphology and viability and did not increase LDH activity. The data indicated that BPC at 5 μmol/L exhibited significant proangiogenic properties and that it might represent a potential agent for the development of therapeutic drugs to treat ischemic diseases.
Author contribution
Jun-ying MIAO and Bao-xiang ZHAO designed the research; Hai-yan ZHANG, Le SU, Bin HUANG, Jing ZHAO, and Shang-li ZHANG performed the research; Shang-li ZHANG analyzed the data; Hai-yan ZHANG wrote the paper.
References
Chatterjee S, Chapman KE, Fisher AB . Lung ischemia: a model for endothelial mechanotransduction. Cell Biochem Biophys 2008; 52: 125–38.
Chunga BH, Leec JJ, Kimb JD, Jeoungd D, Leed H, Choe J, et al. Angiogenic activity of sesamin through the activation of multiple signal pathways. Biochem Biophys Res Commun 2009; 391: 254–60.
Xia Y, Fan CD, Zhao BX, Zhao J, Shin DS, Miao JY . Synthesis and structure-activity relationships of novel 1-arylmethyl-3-aryl-1H-pyrazole-5-carbohydrazide hydrazone derivatives as potential agents against A549 lung cancer cells. Eur J Med Chem 2008; 43: 2347–53.
Fan CD, Zhao BX, Wei F, Zhang GH, Dong WL, Miao JY . Synthesis and discovery of autophagy inducers for A549 and H460 lung cancer cells, novel 1-(2′-hydroxy-3′-aroxypropyl)-3-aryl-1H-pyrazole-5-carbohydrazide derivatives. Bioorg Med Chem Lett 2008; 18: 3860–4.
Zhao BX, Zhang L, Zhu XS, Wan MS, Zhao J, Zhang Y, et al. Synthesis and discovery of a novel pyrazole derivative as an inhibitor of apoptosis through modulating integrin beta4, ROS, and p53 levels in vascular endothelial cells. Bioorg Med Chem 2008; 16: 5171–80.
Ge YQ, Xia Y, Wei F, Dong WL, Zhao BX . N-Benzyl-5-phenyl-1H-pyrazole-3-carboxamide. Acta Cryst 2007; E63; o1186–o1187.
Ge YQ, Dong WL, Xia Y, Wei F, Zhao BX . Ethyl 3-(2-hydroxy-5-methylphenyl)-1H-pyrazole-5-carboxylate. Acta Cryst 2007; E63: o1313–o1314.
Dong WL, Ge YQ, Xia Y, Zhao BX . Ethyl 5-(ethoxycarbonyl)-3-phenyl-1H-pyrazole-1-acetate. Acta Cryst 2007; E63: o4701.
Dong WL, Ge YQ, Zhao BX . Ethyl 5-(ethoxycarbonyl)-3-(4-methoxyphenyl)-1H-pyrazole-1-acetate. Acta Cryst 2008; E64: o64.
Xia C, Meng Q, Liu LZ, Rojanasakul Y, Wang XR, Jiang BH . Reactive oxygen species regulate angiogenesis and tumor growth through vascular endothelial growth factor. Cancer Res 2007; 67: 10823–30.
Jaffe EA, Nachman RL, Becker CG, Minick CR . Culture of human endothelial cells derived from umbilical veins. Identification by morphologic and immunologic criteria. J Clin Invest 1973; 52: 2745–56.
Chen YH, Xu X, Sheng MJ, Zhang XY, Gu Q, Zheng Z . PRMT-1 and DDAHs-induced ADMA upregulation is involved in ROS- and RAS-mediated diabetic retinopathy. Exp Eye Res 2009; 89: 1028–34.
Price P, McMillan TJ . Use of the tetrazolium assay in measuring the response of human tumor cells to ionizing radiation. Cancer Res 1990; 50: 1392–6.
Meng N, Wu L, Gao J, Zhao J, Su L, Su H, et al. Lipopolysaccharide induces autophagy through BIRC2 in human umbilical vein endothelial cells. J Cell Physiol 2010; 225, 174–9.
Kureishi Y, Luo Z, Shiojima I, Bialik A, Fulton D, Lefer DJ, et al. The HMG-CoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals. Nat Med 2000; 6: 1004–10.
Burk RR . A factor from a transformed cell line that affects cell migration. Proc Natl Acad Sci USA 1973; 70: 369–72.
Vasvari GP, Dyckhoff G, Kashfi F, Lemke B, Lohr J, Helmke BM, et al. Combination of thalidomide and cisplatin in an head and neck squamous cell carcinomas model results in an enhanced antiangio-genic activity in vitro and in vivo. Int J Cancer 2007; 121: 1697–704.
Su L, Zhao B, Lv X, Wang N, Zhao J, Zhang S, et al. Safrole oxide induces neuronal apoptosis through inhibition of integrin beta4/SOD activity and elevation of ROS/NADPH oxidase activity. Life Sci 2007; 80: 999–1006.
Araki S, Shimada Y, Kaji K, Hayashi H . Apoptosis of vascular endothelial cells by fibroblast growth factor deprivation. Biochem Biophys Res Commun 1990; 168: 1194–200.
Matsunaga N, Shimazawa M, Otsubo K, Hara H . Phosphatidylinositol inhibits vascular endothelial growth factor-A-induced migration of human umbilical vein endothelial cells. J Pharmacol Sci 2008; 106: 128–35.
Gao N, Ding M, Zheng JZ, Zhang Z, Leonard SS, Liu KJ, et al. Vanadate-induced expression of hypoxia-inducible factor 1α and vascular endothelial growth factor through phosphatidylinositol 3-kinase/Akt pathway and reactive oxygen species. J Biol Chem 2002; 277: 31963–71.
Liu LZ, Hu XW, Xia C, He J, Zhou Q, Shi X, et al. Reactive oxygen species regulate epidermal growth factor-induced vascular endothelial growth factor and hypoxia-inducible factor-1α expression through activation of AKT and P70S6K1 in human ovarian cancer cells. Free Radic Biol Med 2006; 41: 1521–33.
Folkman J . Angiogenesis: an organizing principle for drug discovery? Nat Rev Drug Discov 2007; 6: 273–86.
Ushio-Fukai M, Alexander RW . Reactive oxygen species as mediators of angiogenesis signaling: role of NAD(P)H oxidase. Mol Cell Biochem 2004; 264, 85–97.
Zhao W, Zhao T, Chen Y, Ahokas RA, Sun Y . Reactive oxygen species promote angiogenesis in the infarcted rat heart. Int J Exp Pathol 2009; 90: 621–9.
Harfouche R, Malak NA, Brandes RP, Karsan A, Irani K, Hussain SN . Roles of reactive oxygen species in angiopoietin-1/tie-2 receptor signaling. FASEB J 2005; 19: 1728–30.
Kung HN, Chien CL, Chau GY, Don MJ, Lu KS, Chau YP . Involvement of NO/cGMP signaling in the apoptotic and anti-angiogenic effects of beta-lapachone on endothelial cells in vitro. J. Cell Physiol 2007; 2: 522–32.
Borgmann S, Radtke I, Erichsen T, Blochl A, Heumann R, Schuhmann W . Electrochemical high-content screening of nitric oxide release from endothelial cells. Chembiochem 2006; 4: 662–8.
Cudmore M, Ahmad S, Al-Ani B, Hewett P, Ahmed S, Ahmed A . VEGF-E activates endothelial nitric oxide synthase to induce angiogenesis via cGMP and PKG-independent pathways. Biochem Biophys Res Commun 2006; 345: 1275–82.
Sharp SY, Boxall K, Rowlands M, Prodromou C, Roe SM, Maloney A, et al. In vitro biological characterization of a novel, synthetic diaryl pyrazole resorcinol class of heat shock protein 90 inhibitors. Cancer Res 2007; 67: 2206–16.
Tao ZF, Li G, Tong Y, Chen Z, Merta P, Kovar P, et al. Synthesis and biological evaluation of 4′-(6,7-disubstituted-2,4-dihydro-indeno [1,2-c]pyrazol-3-yl)-biphenyl-4-ol as potent Chk1 inhibitors. Bioorg Med Chem Lett 2007; 17: 4308–15.
Acknowledgements
This work was financially supported by the National 973 Research Project (No 2011CB503906), the National Natural Science Foundation of China (No 90813022 and 20972088) and the Science and Technology Developmental Project of Shandong Province (No 2008GG10002034 and Z2008D04).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zhang, Hy., Su, L., Huang, B. et al. N-benzyl-5-phenyl-1H-pyrazole-3-carboxamide promotes vascular endothelial cell angiogenesis and migration in the absence of serum and FGF-2. Acta Pharmacol Sin 32, 209–216 (2011). https://doi.org/10.1038/aps.2010.201
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2010.201
Keywords
This article is cited by
-
Pseudolaric acid B-driven phosphorylation of c-Jun impairs its role in stabilizing HIF-1alpha: a novel function-converter model
Journal of Molecular Medicine (2012)