Abstract
Aim:
To evaluate the clinical impact of reduced heparin responsiveness (HRreduced) on the incidence of myocardial infarction (MI) following off-pump coronary artery bypass graft surgery (OPCAB), and to identify the predictors of HRreduced.
Methods:
A total of 199 patients scheduled for elective OPCAB were prospectively enrolled. During anastomosis, 150 U/kg of heparin was injected to achieve an activated clotting time (ACT) of ≥300 s, and the heparin sensitivity index (HSI) was calculated. HSIs below 1.0 were considered reduced (HRreduced). The relationships between the HSI and postoperative MI, cardiac enzyme levels and preoperative risk factors of HRreduced were investigated.
Results:
There was no significant relationship between the HSI and cardiac enzyme levels after OPCAB. The incidence of MI after OPCAB was not higher in HRreduced patients. HRreduced occurred more frequently in patients with low plasma albumin concentrations and high platelet counts.
Conclusion:
HRreduced was not associated with adverse ischemic outcomes during the perioperative period in OPCAB patients, which seemed to be attributable to a tight prospective protocol for obtaining a target ACT regardless of the presence of HRreduced.
Similar content being viewed by others
Introduction
Heparin inhibits thrombin generation by binding to antithrombin III (AT-III), and heparin is widely used as an anticoagulant during percutaneous coronary interventions (PCI) and coronary artery bypass graft surgery (CABG) to prevent thromboembolic complications1, 2, 3. However, large variability exits in individual heparin responsiveness4, 5, and despite the theoretical possibility of increased periprocedural ischemic events associated with reduced heparin responsiveness (HRreduced), clinical evidence is either contradictory or limited.
In patients undergoing PCIs, conflicting results exist with regard to the association between HRreduced and ischemic complications such as abrupt vessel closure during and after angioplasty6, 7, 8, 9, 10. In the surgical setting, only a single retrospective study has been performed to evaluate the relationship between ischemic complications in patients undergoing on-pump CABG, which found a close correlation between HRreduced and fatal myocardial infarction (MI)11.
Surgical revascularization is also widely performed by off-pump coronary artery bypass graft surgery (OPCAB) during which a similar degree of anticoagulation, as used during PCIs, is sufficient. Unlike with PCIs, however, all patients presenting for OPCAB have previous exposure to heparin during coronary angiography, which is one of the well-established risk factors of HRreduced4, 5, 12. Moreover, OPCAB still confers significant inflammatory responses and is associated with a postoperative procoagulant state relative to on-pump CABG13, 14. Concerning the possible relationship between HRreduced and an increased risk of ischemic events, there is still no clear recognition of patients with HRreduced or the clinical significance of HRreduced in patients undergoing OPCAB at present.
The aim of this study was to prospectively identify predictors of HRreduced and its clinical impact with regard to the incidences of MI and other major morbidity endpoints in the immediate postoperative period in patients undergoing OPCAB.
Materials and methods
Patients
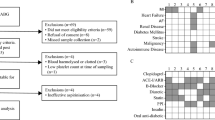
This was a prospective study enrolling all consecutive patients scheduled for elective isolated multivessel OPCAB between April 2007 and March 2008 at a single university hospital. The approval of the institutional review board and patients consent were obtained. Exclusion criteria were the presence of known preoperative coagulopathy, emergency surgery or preoperative use of an intra-aortic balloon pump.
Patients demographics; preoperative medications, including anticoagulant therapy; and preoperative hematological and biochemical laboratory results, including hematocrit, total white cell count, percentage of neutrophils, platelet count, plasma protein and albumin concentrations, C-reactive protein (CRP), fibrinogen concentration, activated partial thromboplastin time, and prothrombin time, as well as levels of myocardial enzymes including creatinine kinase-MB (CK-MB) and troponin (Tn) T, were assessed. Additionally, the preoperative AT-III concentration and activated clotting time (ACT) were assessed.
All patients received standard anesthetic and surgical care according to institutional guidelines by physicians blinded to this study.
Measurement for ACT
ACT was monitored with the Hemochron® Response Whole Blood Coagulation System (International Technidyne Corp (ITC), Edison, NJ, USA) using Hemochron HRFTCA510 celite ACT tubes.
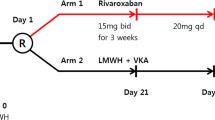
Heparin sensitivity index
Baseline ACT was determined by blood sampling immediately after the insertion of the arterial line. An initial dose of 150 U/kg of porcine heparin was injected into a central venous line just prior to Y-graft formation; the target ACT value was 300 s15. Ten minutes after the loading dose, the ACT was measured. An ACT of 300 s or greater was considered adequate. Then, a follow up ACT measurement was taken 30 min after the first ACT measurement. If the ACT fell below the target value of 300 s, an additional dose of heparin was administered. If the ACT was between 250 and 299 s, an additional 2000 U of heparin was administered, and if the ACT was between 200 and 249 s, then an additional 3000 U of heparin was injected. Ten minutes after the injection of additional heparin, the ACT was remeasured. Upon completion of anastomoses, the ACT was measured again, and the heparin activity was neutralized with protamine sulfate. If the ACT was greater than 300 s, 50 mg of protamine sulfate was administered. If the ACT was between 251 and 299 s or between 200 and 250 s, 30 mg or 20 mg protamine sulfate was administered, respectively. Patients were considered to have HRreduced if the heparin sensitivity index [HSI, HSI=(post-heparin ACT – baseline ACT)/heparin loading dose (U/kg)] was below 1.0 after the initial dose of 150 U/kg of heparin16. Patients with HSI≥1 were considered to have normal heparin responsiveness (HRnormal).
Variables assessed
Intraoperative variables such as the total amount of heparin and protamine administered, the number and nature of grafts, the amount of blood loss and the amount transfused were recorded. The amount of blood loss and blood transfused during postoperative period, the coagulation profiles and myocardial enzyme levels were recorded.
All of the patients were transferred to the intensive care unit (ICU) after surgery and treated with fentanyl-based intravenous patient-controlled analgesia for 2–3 d for pain control, and anti-platelet therapy was started within 24 h unless contraindicated.
In the immediate postoperative period, the following variables were assessed. The highest postoperative CK-MB and Tn-T levels were recorded during first seven postoperative days. Clinical diagnostic criteria for MI were defined as the occurrence of an increase in cardiac enzyme levels five times above the upper normal limit; new Q waves of greater than 0.04 mm or a reduction in R waves greater than 25% in at least 2 leads, or both; new ST elevation in at least 2 contiguous leads measuring more than 0.2 mV in leads V1–V3 or more than 0.1 mV in all other leads; or a new left bundle branch block17. Postoperative major morbidity endpoints were defined as permanent stroke, renal dysfunction, hemostatic re-exploration, deep sternal wound infection, and prolonged ventilation (>48 h)18. For clarification, renal dysfunction was defined as an acute postoperative renal insufficiency resulting in 1 or more of the following: (1) an increase in the serum creatinine level (Cr) to >2.0 mg/dL, (2) a ≥50% increase in Cr over the preoperative baseline value, or (3) a new requirement for dialysis. The development of de novo atrial fibrillation was also assessed. Patients were followed up for 6 months postoperatively for cardiac morbidities/mortality and restenosis, which was defined as stenosis with a cross-sectional diameter >50% at the site of bypass graft as assessed by computed tomography (CT) angiography. Cardiac morbidities included Q-wave and non-Q-wave MI and the need for repeat revascularization19.
Statistical analysis
Statistical analyses were performed with SPSS 12.0 software (SPSS, Inc, Chicago, IL, USA). Data were expressed as the mean±SD or as the number of patients (percentage). Data were tested using the Pearson χ2 test, Mann-Whitney U-test or Student's t test, as appropriate, to compare patients with HRreduced to patients with HRnormal. Factors associated with HRreduced with a P value <0.05 in the univariate analysis were entered into a multivariate logistic regression analysis following a stepwise, forward model. To evaluate the relationship between the HSI and changes in cardiac enzyme levels (highest postoperative cardiac enzyme level – preoperative cardiac enzyme level), linear regression analysis was performed. We determined that at least 148 patients would be required to detect a two-fold increase in the incidence of postoperative MI in patients with HRreduced7 at an alpha level of 0.05 with 80% power, considering the 20% incidence of HRreduced16, 20 in cardiac surgical patients and the 8% incidence of postoperative MI following OPCAB in our institute21.
Results
A total of 199 patients were enrolled during this study period. Thirty-one (15.5%) of these 199 patients met the criteria for HRreduced (HSI range, 0.51 to 0.99). In the HRnormal group, the HSI range was 1.00 to 4.04. The patient characteristics were not different between the two groups. Preoperative medications and the number of patients requiring continuous heparin use preoperatively were also similar between the groups (Table 1).
The preoperative laboratory results indicated that patients with HRreduced were more likely to have significantly lower Hct, plasma total protein and plasma albumin concentrations; significantly higher neutrophil percentages, platelet counts, CRP and fibrinogen concentrations; and significantly shortened partial thromboplastin times compared to patients with HRnormal (Table 2). In multivariate analysis, low plasma albumin concentrations (P=0.001, odds ratio 0.191, 95% confidence interval 0.073–0.498) and high platelet counts (P=0.033, odds ratio 1.006, 95% confidence interval 1.000–1.011) remained independent risk factors of HRreduced.
During surgery, patients with HRreduced received significantly larger amounts of heparin and transfused red blood cells (Table 3).
There was no significant relationship between the HSI and changes in the CK-MB and Tn-T levels (P=0.804 and 0.904, respectively). The HSI was also similar between the patients with and without postoperative myocardial infarction (1.5±0.5 vs 1.5±0.4, P=0.939). The incidence of perioperative MI within 7 d and the incidence of other postoperative complications were not significantly different between the two groups (Table 4). During the 6 month follow up period, none of the patients developed symptoms of ischemia except 1 patient in the HRnormal group who developed a symptomatic arrhythmia caused by restenosis of the venous graft to the right coronary artery and underwent PCI with a stent procedure. CT angiography was performed in 105 patients and 16 patients of the HRnormal and HRreduced groups, respectively. Sixteen patients in the HRnormal group met the predefined criteria of restenosis, in contrast to none of the patients in the HRreduced group (Table 4).
Discussion
In this prospective study evaluating the risk factors for HRreduced and its association with MI and morbidity endpoints following OPCAB, low albumin concentrations and high platelet counts were identified as independent predictors of HRreduced. However, the incidences of postoperative MI and morbidity endpoints including cardiac morbidities were not increased in patients with HRreduced.
The use of heparin during procedures involving coronary arteries requires particular attention to decrease perioperative thrombogenesis without increasing the risk of bleeding. During cardiopulmonary bypass (CPB), ACTs of less than 300 s caused coagulation in bypass circuits, and ACTs are recommended to be longer than 400–480 s1, 22. Accordingly, a single retrospective review evaluating the impact of heparin responsiveness on ischemic complications within the first postoperative 48 h revealed that HRreduced was an important risk factor for fatal MI after on-pump CABG11. Additionally, in patients undergoing coronary balloon angioplasty, there was an inverse relationship between heparin responsiveness and the incidence of abrupt vessel collapse during and after angioplasty7, 8, 23. On the contrary, other studies involving patients undergoing stent insertion reported no correlation between heparin responsiveness and ischemic complications9, 10, although there was a case of stent thrombosis associated with HRreduced6.
OPCAB constitutes an important axis as a surgical revascularization technique of diseased coronary arteries, and by avoiding CPB, a reduced amount of heparin is required during surgery. Based on previous studies, ACTs between 250 and 300 s during OPCAB seem to be acceptable in many institutions22, 24, and the majority of hospitals administered 150 U/kg heparin at the beginning of graft anastomosis for a target ACT value of approximately 300 s15, which is similar to that for PCI. In view of the inflammation and coagulation statuses, OPCAB stands in a unique position because it is still associated with significant inflammatory responses and the activation of the coagulation and fibrinolytic systems following mid-sternotomy and cardiac manipulation, which are more pronounced in OPCAB patients than in patients undergoing PCI2, 25. Moreover, it has been demonstrated that OPCAB is associated with a postoperative procoagulant state related to increases in prothrombin factor and von Willebrand factor and to transient platelet dysfunction compared to on-pump CABG13, 14. In addition, unlike for PCI, all patients presenting for OPCAB have previous exposure to heparin during coronary angiography, which is a well-known risk factor for HRreduced4, 5, 12, and yet, evidence is lacking with regard to heparin responsiveness and its clinical impact on OPCAB patients. Thus, we aimed to evaluate factors affecting HRreduced and the relationship between heparin responsiveness and postoperative MI and morbidity endpoints.
As our results indicate, patients with HSIs<1.0 composed 16% of the study population, and low albumin concentrations and high platelet counts were identified as independent predictors of HRreduced. However, we did not observe any relationship between the HSI and changes in myocardial enzyme levels, and the HSI was also similar between patients with and without postoperative MI. Plausible causes for these results are as follows. Although previous studies found adverse ischemic outcomes in patients with HRreduced, these studies were either retrospective or did not prospectively manage the target ACT as in this study. In the current trial, the ACT was closely monitored and maintained at >300 s prospectively by administering additive heparin if necessary during grafting. The ACT measured after the last heparin dose and before coronary anastomosis was above 300 s in all patients; this may be why HRreduced did not demonstrate any clinical relevance with respect to myocardial enzyme levels and MI during the perioperative period. This is in accordance with the results of previous studies in the PCI setting in which ACT was prospectively managed to be at least 225 s regardless of the presence of HRreduced9, 10. Considering that patients with HRreduced seemed to be in a preoperatively hypercoagulable state and that the minimum ACT during surgery was significantly lower in patients with HRreduced (297±44 s vs 253±23 s, P<0.001), it still might be important to acknowledge the risk in these patients and to perform additional and frequent ACT measurements to maintain an adequate ACT level and to titrate the heparin dosage during surgery. Inflammatory markers such as CRP and the neutrophil percentages were not independent risk factors for HRreduced. Perhaps the utilization of more distinct inflammatory markers such as interleukins could have resulted in a different outcome. Unlike previous studies of cardiac surgery, in our study, the AT-III levels were not lower in patients with HRreduced, and only a few patients exhibited AT-III levels below 60% (4 in the HRnormal and 1 in the HRreduced group). Low AT-III activity has been reported to contribute to HRreduced and hypercoagulability26, 27 and could result in major thrombotic complications after PCI and on-pump CABG28, 29. Considering the significant decrease in AT-III activity during on-pump CABG30, the different results compared to the previous study may also be partly attributable to the variable AT-III activity. Although, the HRreduced group received a significantly larger amount of heparin and transfused red blood cells during surgery, it is difficult to establish a direct relationship between them because the HRreduced group initially had a lower hematocrit level.
Heparin responsiveness potentially may influence not only the periprocedural morbidity but also the long term patency of grafted vessels. Heparin inhibits the activation of the mitogen-activated protein kinase in vascular smooth muscle cells, and thus, the relative resistance to the antiproliferative action of heparin could be associated with long term graft patency31. In an in vitro study, heparin resistance in cultured vascular smooth muscle cells was a highly significant predictor of subsequent vein graft stenosis32. Although there have been few studies evaluating whether a population clinically characterized by HRreduced during vascular procedures has concurrent hyperstenotic characteristics with an increased risk of graft stenosis, more careful follow-up is required in these patients. In this study, HRreduced was not associated with cardiac morbidities or restenosis of graft vessels during a six month follow-up period after OPCAB.
The limitations of this study are as follows. The anti-platelet therapy consisting of aspirin and clopidogrel was started empirically 24 h after surgery as appropriate, and the inter-individual variability of clopidogrel responsiveness was not assessed, which might have affected the ischemic outcomes of the patients regardless of the HSI33.
In conclusion, low plasma albumin concentrations and high platelet counts were identified as independent predictors of HRreduced. Despite a strong theoretical possibility and a close relationship between HRreduced and postoperative MI in on-pump CABG patients, HRreduced was not associated with adverse ischemic outcomes during the postoperative period after OPCAB. A tight prospective protocol for obtaining a target ACT regardless of the presence of HRreduced seems to be of the highest importance while performing surgical revascularization.
Author contribution
Duk-hee CHUN, Seong-wan BAIK, and Young Lan KWAK designed the study; Duk-hee CHUN, So Yeon KIM, Jae Kwang SHIM, and Jong Chan KIM performed the research; Duk-hee CHUN, Seong-wan BAIK, and Jae Kwang SHIM analyzed the data; Young Lan KWAK wrote the manuscript.
References
Avidan MS, Levy JH, van Aken H, Feneck RO, Latimer RD, Ott E, et al. Recombinant human antithrombin III restores heparin responsiveness and decreases activation of coagulation in heparin-resistant patients during cardiopulmonary bypass. J Thorac Cardiovasc Surg 2005; 130: 107–13.
Karmanoukian H, Attuwabi B, Nader ND . Antithrombotic controversies in off-pump coronary bypass. Semin Thorac Cardiovasc Surg 2005; 17: 59–65.
Levy JH . Heparin resistance and antithrombin: should it still be called heparin resistance? J Cardiothorac Vasc Anesth 2004; 18: 129–30.
Cloyd GM, D'Ambra MN, Akins CW . Diminished anticoagulant response to heparin in patients undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 1987; 94: 535–8.
Staples MH, Dunton RF, Karlson KJ, Leonardi HK, Berger RL . Heparin resistance after preoperative heparin therapy or intraaortic balloon pumping. Ann Thorac Surg 1994; 57: 1211–6.
Kaku B, Katsuda S, Taguchi T, Nitta Y, Hiraiwa Y . A case of acute myocardial infarction with repetitive stent thrombosis during emergent percutaneous coronary intervention. Transient decrease in antithrombin III activity and heparin resistance. Int Heart J 2009; 50: 111–9.
Ferguson JJ, Dougherty KG, Gaos CM, Bush HS, Marsh KC, Leachman DR . Relation between procedural activated coagulation time and outcome after percutaneous transluminal coronary angioplasty. J Am Coll Cardiol 1994; 23: 1061–5.
Narins CR, Hillegass WB Jr, Nelson CL, Tcheng JE, Harrington RA, Phillips HR, et al. Relation between activated clotting time during angioplasty and abrupt closure. Circulation 1996; 93: 667–71.
Brener SJ, Moliterno DJ, Lincoff AM, Steinhubl SR, Wolski KE, Topol EJ . Relationship between activated clotting time and ischemic or hemorrhagic complications: analysis of 4 recent randomized clinical trials of percutaneous coronary intervention. Circulation 2004; 110: 994–8.
Tolleson TR, O'Shea JC, Bittl JA, Hillegass WB, Williams KA, Levine G, et al. Relationship between heparin anticoagulation and clinical outcomes in coronary stent intervention: observations from the ESPRIT trial. J Am Coll Cardiol 2003; 41: 386–93.
Ranucci M, Frigiola A, Menicanti L, Cazzaniga A, Soro G, Isgro G . Risk factors for fatal myocardial infarction after coronary bypass graft surgery. Eur J Anaesthesiol 2001; 18: 322–9.
Chan T, Hwang NC, Lim CH . A statistical analysis of factors predisposing patients to heparin resistance. Perfusion 2006; 21: 99–103.
Moller CH, Steinbruchel DA . Platelet function after coronary artery bypass grafting: is there a procoagulant activity after off-pump compared with on-pump surgery? Scand Cardiovasc J 2003; 37: 149–53.
Mariani MA, Gu YJ, Boonstra PW, Grandjean JG, van Oeveren W, Ebels T . Procoagulant activity after off-pump coronary operation: is the current anticoagulation adequate? Ann Thorac Surg 1999; 67: 1370–5.
Englberger L, Streich M, Tevaearai H, Carrel TP . Different anticoagulation strategies in off-pump coronary artery bypass operations: a European survey. Interact Cardiovasc Thorac Surg 2008; 7: 378–82.
Ranucci M, Isgro G, Cazzaniga A, Ditta A, Boncilli A, Cotza M, et al. Different patterns of heparin resistance: therapeutic implications. Perfusion 2002; 17: 199–204.
French JK, White HD . Clinical implications of the new definition of myocardial infarction. Heart 2004; 90: 99–106.
Shroyer AL, Coombs LP, Peterson ED, Eiken MC, DeLong ER, Chen A, et al. The Society of Thoracic Surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg 2003; 75: 1856–64; discussion 1864–5.
Keeley EC, Velez CA, O'Neill WW, Safian RD . Long-term clinical outcome and predictors of major adverse cardiac events after percutaneous interventions on saphenous vein grafts. J Am Coll Cardiol 2001; 38: 659–65.
Avidan MS, Levy JH, Scholz J, Delphin E, Rosseel PM, Howie MB, et al. A phase III, double-blind, placebo-controlled, multicenter study on the efficacy of recombinant human antithrombin in heparin-resistant patients scheduled to undergo cardiac surgery necessitating cardiopulmonary bypass. Anesthesiology 2005; 102: 276–84.
Choi YS, Shim JK, Hong SW, Kim DH, Kim JC, Kwak YL . Risk factors of atrial fibrillation following off-pump coronary artery bypass graft surgery: predictive value of C-reactive protein and transfusion requirement. Eur J Cardiothorac Surg 2009; 36: 838–43.
Tanaka KA, Thourani VH, Williams WH, Duke PG, Levy JH, Guyton RA, et al. Heparin anticoagulation in patients undergoing off-pump and on-pump coronary bypass surgery. J Anesth 2007; 21: 297–303.
Bittl JA, Ahmed WH . Relation between abrupt vessel closure and the anticoagulant response to heparin or bivalirudin during coronary angioplasty. Am J Cardiol 1998; 82: 50P–56P.
Hansen KH, Hughes P, Steinbruchel DA . Antithrombotic- and anticoagulation regimens in OPCAB surgery. A Nordic survey. Scand Cardiovasc J 2005; 39: 369–74.
Raivio P, Kuitunen A, Suojaranta-Ylinen R, Lassila R, Petaja J . Thrombin generation during reperfusion after coronary artery bypass surgery associates with postoperative myocardial damage. J Thromb Haemost 2006; 4: 1523–9.
Na S, Shim JK, Chun DH, Kim DH, Hong SW, Kwak YL . Stabilized infective endocarditis and altered heparin responsiveness during cardiopulmonary bypass. World J Surg 2009; 33: 1862–7.
Lemmer JH Jr, Despotis GJ . Antithrombin III concentrate to treat heparin resistance in patients undergoing cardiac surgery. J Thorac Cardiovasc Surg 2002; 123: 213–7.
Matthai WH Jr, Kurnik PB, Groh WC, Untereker WJ, Siegel JE . Antithrombin activity during the period of percutaneous coronary revascularization: relation to heparin use, thrombotic complications and restenosis. J Am Coll Cardiol 1999; 33: 1248–56.
Loubser PG, McCarthy JJ, Attar M . Coronary thrombosis associated with antithrombin-III deficiency. J Cardiothorac Vasc Anesth 1997; 11: 756–9.
Hashimoto K, Yamagishi M, Sasaki T, Nakano M, Kurosawa H . Heparin and antithrombin III levels during cardiopulmonary bypass: correlation with subclinical plasma coagulation. Ann Thorac Surg 1994; 58: 799–804; discussion 804–5.
Sindermann JR, March KL . Heparin responsiveness in vitro as a prognostic tool for vascular graft stenosis: a tale of two cell types? Circulation 1998; 97: 2486–90.
Refson JS, Schachter M, Patel MK, Hughes AD, Munro E, Chan P, et al. Vein graft stenosis and the heparin responsiveness of human vascular smooth muscle cells. Circulation 1998; 97: 2506–10.
Patti G, Nusca A, Mangiacapra F, Gatto L, D'Ambrosio A, Di Sciascio G . Point-of-care measurement of clopidogrel responsiveness predicts clinical outcome in patients undergoing percutaneous coronary intervention results of the ARMYDA-PRO (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty-Platelet Reactivity Predicts Outcome) study. J Am Coll Cardiol 2008; 52: 1128–33.
Acknowledgements
This study was supported by a faculty research grant (6-2008-0187) of Yonsei University College of Medicine of 2008.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chun, Dh., Baik, Sw., Kim, S. et al. Heparin responsiveness during off-pump coronary artery bypass graft surgery: predictors and clinical implications. Acta Pharmacol Sin 32, 133–138 (2011). https://doi.org/10.1038/aps.2010.180
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2010.180