Abstract
Aim:
Depolarization-induced contraction of smooth muscle is thought to be mediated by Ca2+ influx through voltage-gated L-type Ca2+ channels. We describe a novel contraction mechanism that is independent of Ca2+ entry.
Methods:
Pharmacological experiments were carried out on isolated rat gut longitudinal smooth muscle preparations, measuring isometric contraction strength upon high K+-induced depolarization.
Results:
Treatment with verapamil, which presumably leads to a conformational change in the channel, completely abolished K+-induced contraction, while residual contraction still occurred when Ca2+ entry was blocked with Cd2+. These results were further confirmed by measuring intracellular Ca2+ transients using Fura-2. Co-application of Cd2+ and the ryanodine receptor blocker DHBP further reduced contraction, albeit incompletely. Additional blockage of either phospholipase C (U 73122) or inositol 1,4,5-trisphophate (IP3) receptors (2-APB) abolished most contractions, while sole application of these blockers and Cd2+ (without parallel ryanodine receptor manipulation) also resulted in incomplete contraction block.
Conclusion:
We conclude that there are parallel mechanisms of depolarization-induced smooth muscle contraction via (a) Ca2+ entry and (b) Ca2+ entry-independent, depolarization-induced Ca2+-release through ryanodine receptors and IP3, with the latter being dependent on phospholipase C activation.
Similar content being viewed by others
Introduction
Smooth muscle contraction is widely accepted to be triggered by a rise in cytosolic free Ca2+ concentration ([Ca2+]i), which is regulated by either pharmacomechanical coupling to agonists that induce contraction without membrane depolarization, or by membrane depolarization itself in a process known as electromechanical coupling1, 2, 3. The rise in [Ca2+]i leads to calmodulin-dependent activation of myosin light chain kinase (MLCK) and results in the phosphorylation of the 20-kDa light chain of myosin4, 5. Pharmacomechanical coupling may depend on Ca2+ influx through receptor-operated Ca2+ channels6 or on Ca2+ release from the sarcoplasmic reticulum following an intracellular second messenger cascade involving G protein-coupled receptor-dependent phospholipase C (PLC) activation7. When activated, PLC utilizes membrane-bound phosphatidylinositol 4,5-bisphosphate to produce inositol 1,4,5-trisphophate (IP3), which in turn activates IP3 receptors at the sarcoplasmic reticulum, resulting in IP3-induced Ca2+ release (IICR)8. In addition to these IP3 receptors, [Ca2+]i can also be increased by ryanodine receptors (RyRs) through a mechanism called Ca2+-induced Ca2+ release (CICR). In this process, cytosolic Ca2+ ions can trigger further Ca2+ release9, 10. Alternatively, this may also occur through the Ca2+-dependent activation of the cyclic ADP-ribose pathway7, 11.
Electromechanical coupling, such as high K+-induced contraction, is believed to rely on cell surface voltage-gated Ca2+ channels (VGCCs), which are activated by cell membrane depolarization and cause an increase in [Ca2+]i12. However, it remains unknown whether depolarization-induced contraction in smooth muscle is entirely dependent on the influx of extracellular Ca2+. At the very least, extracellular Ca2+ ions entering the cell through VGCCs might also trigger Ca2+ release from internal stores via RyRs. Another possibility is that depolarization is directly coupled to sarcoplasmic Ca2+ release channels. Indeed, depolarization-induced Ca2+ release (DICR) is known to be essential for excitation-contraction coupling in the skeletal muscle, and this mechanism relies on a mechanical linkage between RyR1 and cell surface voltage sensor Cav1.113, 14. Thus, it is possible that DICR can also account for smooth muscle electromechanical coupling.
In the present study, we assessed the contributions of extracellular versus intracellular Ca2+ during high K+-induced contraction in the smooth muscle of the small intestine. Our data suggest that depolarization-induced contraction involves substantial Ca2+ release from internal stores. Moreover, we found that depolarization without Ca2+ influx into the cell can induce the opening of Ca2+ release channels (ryanodine and IP3 receptors). We conclude that DICR is a physiologically relevant mechanism of electromechanical coupling in gut smooth muscle.
Materials and methods
Preparation and maintenance of gut pieces
Adult male Wistar rats (70–90 d) were deeply anesthetized with diethyl ether and decapitated. All experiments were conducted in accordance with the Guide for the Care and Use of Laboratory Animals. The abdomen was carefully opened and the full-length small intestine was quickly removed. In order to allow the discrimination between the different intestinal segments, three distinct portions were prepared. One portion included the initial 15–20 cm from the stomach and was denoted as the proximal portion. Another portion included the last 15–20 cm before the ileocecal transition and was referred to as the distal portion. The third portion was prepared as the central 15–20 cm and was labeled the middle portion. The proximal, middle and distal portions were subsequently cut into pieces of 1–2 cm in length. Thin nylon threads were sutured to both ends of these pieces to enable longitudinal fixation in the organ bath (Panlab ML0146/C, ADInstruments, Spechbach, Germany). The gut preparations were transferred into a HEPES-buffered storage solution (in mmol/L: 120 NaCl, 4.5 KCl, 26 NaHCO3, 1.2 NaH2PO4, 0.02 CaCl2, 1.0 MgSO4, 0.25 Na2-EDTA, 5.5 glucose, 5 HEPES, pH=7.4) for recovery for 15–60 min at 4 °C before they were fixed into the organ bath. The organ bath (volume 25 mL) was filled with a recording solution that contained (in mmol/L) 120 NaCl, 4.7 KCl, 2.5 CaCl2, 1.2 MgCl2, 30 NaHCO3, 1.2 KH2PO4, 0.5 Na2-EDTA, 5.5 glucose, 2 sodium pyruvate (pH=7.4) and was bubbled with carbogen (95% O2 and 5% CO2). In experiments using CdCl2, KH2PO4 was omitted from the buffer to avoid solubility problems.
Recording isometric contractions and relaxations
After fixation in the organ bath, the preparations were allowed to recover for another 30 min before the experiments were started. During this time the organ bath temperature was raised from room temperature to 37 °C. The initial tension of the pieces of small intestine within the organ bath was adjusted to yield a stable baseline tonus with regular phasic contractions. The gut preparations were challenged with high K+ solution to induce depolarization-induced contraction or with acetylcholine to study cholinergic effects. Isometric contractions and relaxation were measured by force transducers (MLT0201, ADInstruments) and recorded with a bridge amplifier (ML224, ADInstruments) connected to an analog-to-digital converter (Powerlab 4/30, ADInstruments) and analyzed by the Chart 5 software (ADInstruments).
FURA-2 loading and Intracellular Ca2+ measurements
To analyze intracellular Ca2+ transients, the rat gut was cut into small patches and transferred into HEPES-buffered storage solution containing (in mmol/L) 120 NaCl, 26 NaHCO3, 4.5 KCl, 1.2 NaH2PO4, 1 MgSO4, 1.6 CaCl2, 0.25 Na2-EDTA, 5.5 Glucose, 5 HEPES (pH=7.4). After careful removal of the mucosa, gut patches were transferred into a small jar filled with HEPES-buffered loading solution with 10 μmol/L Fura-2 AM (Molecular ProbesTM) and incubated for 60 min at room temperature in the dark followed by a 30 min wash in HEPES-buffered storage solution. For the fluorescence measurement the gut patches were transferred into a perfusion chamber on an inverted fluorescence microscope (Nikon Eclipse FN1, Tokyo, Japan, equipped with an immersion objective: NIR Apo 40x/0,80W DIC N2, Nikon). The patches were perfused with a recording solution containing (in mmol/L) 120 NaCl, 4.7 KCl, 2.5 CaCl2, 1.2 MgCl2, 30 NaHCO3, 1.2 KH2PO4, 0.5 Na2-EDTA, 5.5 glucose, 2 sodium-pyruvate, 0.8 μmol/L atropine, 0.8 μmol/L hexamethonium (pH=7.4, gassed with carbogen) at a flow rate of ∼4 mL/min. Longitudinal smooth muscle cells were visualized using a digital video camera (cooled Retiga-2000RV, QImaging®) and a fluorescence imaging system (ICU and Polychrome V, TILL Photonics by Agilent Technologies) including a software package (TILLvisION 4.0.1.3, TILL Photonics by Agilent Technologies) for data acquisition and analysis. Fura-2 fluorescence (510 nm) was measured at room temperature (22−24 °C) while alternating the two excitation wavelengths (355 and 380 nm) at 2 Hz. The gut patches were challenged with a high K+-containing solution (KCl 90 mmol/L, osmolality corrected by equimolar reduction of NaCl) to evoke depolarization-induced Ca2+ transients.
Chemicals and data analysis
The muscarinic antagonist atropine was purchased from Merck. Verapamil, 1,1′-diheptyl-4,4′-bipyridinium dibromide (DHBP), 2-aminoethoxydiphenylborane (2-APB), 1-[6-[[(17b)-3-methoxyestra-1,3,5(10)-trien-17-yl]amino]hexyl]-1H-pyrrole-2,5-dione (U 73122), and thapsigargin (TG) were purchased from Tocris (Bristol, UK). All other chemicals were obtained from Sigma-Aldrich (Taufkirchen, Germany). DHBP was chosen as a ryanodine receptor blocker because ryanodine itself has both antagonistic and agonistic effects, depending on its dosage15, 16, 17. In a whole muscle preparation, this dosage is difficult to control with bath application; hence the effects of ryanodine would have been less predictable than the effects of DHBP.
Smooth muscle contractions and relaxation were analyzed as the absolute isometric contraction strength values as well as the percentage of the individual high K+-induced isometric contraction strength. We did not observe any differences between the proximal, middle and distal portions in all our experiments, so we pooled the data for our analysis. Statistical analyses were performed using the paired two-tailed Student's t test with a statistical significant difference referred to as P value less than 0.05. All data are presented as the mean±SEM.
Results
Depolarization-induced and acetylcholine-induced contraction
Smooth muscle contraction can be triggered by high K+-induced depolarization (electromechanical coupling) or by acetylcholine application (pharmacomechanical coupling). To investigate viability, rat gut preparations were probed with exogenous acetylcholine to demonstrate intact pharmacological contraction in the longitudinal smooth muscle. Bath application of acetylcholine (1.2 μmol/L) caused a stable tonic contraction that was highly sensitive to the muscarinic receptor antagonist atropine (0.8 μmol/L; Figure 1A, left panel) and less sensitive to the nicotinic receptor antagonist hexamethonium chloride (0.8 μmol/L; Figure 1A, right panel). As shown in Figure 1B, bath application of acetylcholine (1.2 μmol/L) caused a tonic contraction of 17.4±1.5 mN (n=30) that was inverted to a relaxation value of -1.3±1.3 mN following atropine application (n=14, P<0.001). This indicated substantial endogenous tonic acetylcholine release by parasympathetic nerves. A smaller, but significant relaxing effect was achieved with hexamethonium chloride (14.7±2.1 mN, n=16, P<0.05). In order to rule out the possibility that depolarization with high K+ could excite gut parasympathetic nerve fibers leading to acetylcholine release, both atropine and hexamethonium chloride (0.8 μmol/L each) were added to the bath in all of the subsequent experiments.
Acetylcholine-induced and depolarization-induced contraction of gut smooth muscle. (A) Acetylcholine (1.2 μmol/L) evoked strong and long-lasting contraction of gut smooth muscle that was abolished by atropine (0.8 μmol/L), and partly antagonized by hexamethonium chloride (0.8 μmol/L). (B) Bar graph summarizing the acetylcholine (ACh)-induced contraction with and without the muscarinic blocker atropine and the nicotinic blocker hexamethonium, respectively. Note that atropine caused a relaxation (negative force) indicating endogenous ACh release. (C) Depolarization-induced contraction with increasing concentrations of KCl. Equivalent concentrations of NaCl caused relaxation indicating that contraction was not due to the increase of osmolality. (D) Repetitive depolarization with 45 mmol/L KCl induced reproducible contractions in gut smooth muscle. bP<0.05, cP<0.01.
Application of high K+-containing solution to the bath (15–120 mmol/L external K+) caused a dose-dependent contraction of the longitudinal smooth muscle (n=12, Figure 1C, closed circles). As a control for osmolarity changes caused by the application of high K+ concentrations, equivalent amounts of saline solution were applied to the smooth muscle (n=6, Figure 1C, open circles). Intriguingly, increasing osmolarity with saline alone had a strong relaxing, rather than contracting effect indicating that the observed contraction by high K+ was caused by depolarization rather than by the hyperosmolar conditions. In the remaining experiments, 45 mmol/L was used as the standard concentration to study high K+-induced contraction. Repetitive depolarization with 45 mmol/L of K+ induced reproducible contractions in gut smooth muscle (Figure 1D, n=43).
Depolarization-induced contraction requires Ca2+ release from internal stores
Depolarization-induced contraction is mediated by Ca2+ influx through voltage-gated Ca2+ channels, but it may also require Ca2+ release from internal stores. Therefore, we studied high K+-induced contraction before and after depletion of internal Ca2+ stores (Figure 2). At the beginning of the experiment, high K+ application (45 mmol/L) caused a contraction of 16.2±2.4 mN (n=9; Figure 2Aa), which was entirely dependent on a rise in intracellular Ca2+ levels. Indeed, a Ca2+ free solution containing 4 mmol/L EGTA almost abolished this depolarization-induced contraction (0.9±0.2 mN, P<0.001; Figure 2Ab). However, Ca2+ free conditions can also empty internal Ca2+ stores. Thus, we attempted to deplete these stores without changing the external Ca2+ concentration. Depletion of internal Ca2+ stores with pre-application of 10 mmol/L caffeine (activator of ryanodine receptors; Figure 2Ac) or 1 μmol/L thapsigargin (inhibitor of sarcoendoplasmic reticulum Ca2+ ATPase; Figure 2Ad) significantly reduced high K+-induced contractions, although these effects were not complete (caffeine: 2.8±0.6 mN, P<0.01; thapsigargin: 7.4±1.2 mN, P<0.01). Looking at these relative effects, caffeine reduced the contraction strength by 78%±6%, which was significantly greater than the thapsigargin-induced reduction of 52%±5% (P<0.01). Ryanodine receptor blockade with DHBP (100 μmol/L) did not counteract the caffeine effect (data not shown). Whereas internal store depletion by caffeine might have been prevented by DHPB in these experiments, the blocking effect of caffeine on MLCK18 probably occluded any of the ryanodine receptor blocking effects of DHBP. The internal store depletion experiments showed that Ca2+ release from internal stores is required for high K+-induced contraction. Since residual contractile activity may be due to Ca2+ influx through voltage-gated Ca2+ channels, the Ca2+ channel pore blocker CdCl2 (1 mmol/L) was added to the bath containing thapsigargin. Cd2+ and thapsigargin further reduced the high K+-induced contraction significantly (2.8±0.5 mN, P<0.01; Figure 2Ae) as compared with thapsigargin alone. Altogether, thapsigargin and CdCl2 blocked 76%±9% of the initial contraction strength, which was very similar to the effect of caffeine alone.
Depolarization-induced contraction depends on internal Ca2+ stores. (A) Consecutive traces of a representative experiment. High K+ (45 mmol/L) evoked a strong contraction that was almost abolished in Ca2+ free bath solution containing EGTA (4 mmol/L). The high K+-induced contraction was markedly reduced by depletion of internal Ca2+ stores with caffeine (10 mmol/L) or thapsigargin (1 μmol/L). Note the significant difference in residual contraction strength between caffeine and thapsigargin treatment. However, depletion of Ca2+ stores with thapsigargin (1 μmol/L) and inhibition of Ca2+ influx with CdCl2 (1 mmol/L) caused an even more pronounced reduction of the high K+-induced contraction than thapsigargin alone. (B) Bar graph summarizing 9 experiments (mean±SEM). bP<0.05, cP<0.01.
Depolarization-induced contraction involves depolarization-induced Ca2+ release through ryanodine and IP3 receptors via PLC activation
In addition to CICR, Ca2+ release from internal stores may also be evoked by depolarization directly in a process referred to as depolarization-induced Ca2+ release (DICR). To test this, we used Cd2+ to abolish Ca2+ influx through voltage-gated Ca2+ channels without interfering with putative depolarization-induced conformation changes in these channels. As shown in Figure 3, high K+-induced contraction was significantly reduced by 1 mmol/L CdCl2 from 22.2±2.0 mN (Figure 3Aa) to 11.9±1.9 mN (n=16, P<0.001; Figure 3Ab), which was equivalent to a reduction of contraction strength by 46%±7%. In addition, CdCl2 caused a minor but significant delay in the peak latency (9.0±0.8 s versus 6.8±0.4 s). When the ryanodine receptor blocker DHBP (100 μmol/L; Figure 3Ac) or the IP3 receptor blocker 2-APB (100 μmol/L; Figure 3Ad) was added to the CdCl2-containing bath, a more pronounced reduction in the high K+-induced contraction was observed as compared with CdCl2 alone (DHBP: 6.4±1.8 mN, P<0.05; 2-APB: 7.8±1.9 mN, P<0.05). In contrast to their similar effects on contraction strength, the peak latencies of high K+-induced contraction was different between these two blockers. Whereas 2-APB did not have an effect on peak latency (9.1±2.4 s), DHBP significantly delayed the peak to 23.3±4.6 s (P<0.05 compared with the CdCl2-containing bath). Finally, a cocktail consisting of CdCl2, DHBP and 2-APB inhibited smooth muscle contraction even more markedly (4.1±0.9 mN, P<0.05 compared with CdCl2 and DHBP or 2-APB alone; Figure 3Ae). These blockers reduced contraction strength by 79%±5%, which closely resembled the relative reduction observed after caffeine treatment or with co-application of thapsigargin and CdCl2 (Figure 2). Following wash-out, high K+-induced contraction did not fully recover, indicating poor wash-out of DHBP and/or 2-APB (Figure 3Af). To avoid biasing effects due to prolonged drug action, the order of DHBP and 2-APB application was randomized (2-APB after DHBP: n=10, 2-APB before DHBP: n=6). However, no significant differences were observed when comparing the different experimental protocols, and importantly, complete contraction inhibition could not be achieved. However, when the L-type Ca2+ channel blocker verapamil (40 μmol/L), which not only blocks Ca2+ influx but also inhibits conformational changes in the channel19, was applied, virtually no contraction could be observed (0.5±0.2 mN, P<0.001). In a separate set of experiments, we tested the effect of DHBP and/or 2-APB without CdCl2 on high K+-induced contraction. Interestingly, neither DHBP nor 2-APB reduced contraction when applied without CdCl2. The initial high K+-induced contraction value of 17.1±2.5 mN (n=11) was slightly higher following pre-application of DHBP (20.9±3.3 mN) or 2-APB (18.2±3.0 mN). When both DHBP and 2-APB were co-applied, the high K+-induced contraction value was 17.8±3.2 mN (n=11). At the end of the experiment, the high K+-induced contraction fully recovered (18.4±3.1 mN, n=11). In addition, both DHBP and 2-APB relaxed the basal tone of the smooth muscle (−4.3±0.7 mN and −9.0±1.6 mN, respectively) indicating constitutive Ca2+ release under control conditions via both ryanodine receptors and IP3 receptors. Overall, this suggested that unless transmembrane Ca2+ influx is blocked, neither ryanodine receptor nor IP3 receptor blockade alone or in combination prevents contraction. In summary, Ca2+ release from internal stores can be independent of Ca2+ influx through voltage-gated Ca2+ channels. In addition, depolarization-induced Ca2+ release in gut smooth muscle involves both ryanodine and IP3 receptors, probably due to depolarization-induced conformational changes in voltage-gated Ca2+ channels.
Depolarization-induced contraction depends on depolarization-induced Ca2+ release through ryanodine receptors and IP3 receptors. (A) Consecutive traces of a representative experiment. High K+ (45 mmol/L) evoked a strong contraction that was significantly reduced in solution containing 1 mmol/L CdCl2. Additional application of the ryanodine receptor blocker DHBP (100 μmol/L) further reduced the contraction, albeit incompletely. Combined application of CdCl2 and the IP3 receptor blocker 2-APB (100 μmol/L) also incompletely reduced the contraction. Application of CdCl2, DHBP and 2-APB caused a significantly stronger reduction of contraction than CdCl2 with DHBP or 2-APB alone. Verapamil abolished the depolarization-induced contraction. (B) Bar graph summarizing 16 experiments (mean±SEM). bP<0.05, cP<0.01.
Whereas ryanodine receptors directly couple to voltage-gated Ca2+ channels, IP3 receptors require IP3 production through phospholipase C (PLC) activation. Thus, we asked if depolarization-induced conformational changes in voltage-gated Ca2+ channels can lead to IP3 production. As shown in Figure 4, high K+-induced contraction (25.6±2.2 mN; Figure 4Aa) was again significantly reduced by 1 mmol/L CdCl2 treatment to 8.7±1.6 mN (n=17, P<0.001; Figure 4Ab), which also increased the peak latency (from 7.8±0.5 s to 11.7±1.0 s, P<0.01). Similar to the experiments described above, additional application of either the ryanodine receptor blocker DHBP or the PLC blocker U 73122 (5 μmol/L) further reduced this contraction significantly (DHBP: 4.4±0.8 mN, P<0.01, U 73122: 4.0±0.6 mN, P<0.01; Figure 4Ac,d). With respect to peak latencies, U 73122 again had no effect (13.8±1.6 s), whereas DHBP significantly slowed peak contraction (14.7±1.3 s, P<0.05 compared with the CdCl2-containing bath). Finally, the combined application of CdCl2, DHBP and U 73122 further reduced the high K+-induced contraction (3.3±0.6 mN, P<0.05; Figure 4Ae) as compared with CdCl2 and DHBP or U 73122 alone. Interestingly, the relative reduction of contraction strength following CdCl2, DHBP and U 73122 application (85%±4%) was again as high as that observed for caffeine treatment. High K+-induced contraction did not fully recover following wash-out indicating poor removal of these lipophilic drugs from the tissue (Figure 4Af). Therefore, we again changed the order of application between DHBP and U 73122 without obtaining significant differences between these two experimental groups (U 73122 after DHBP: n=14, U 73122 before DHBP: n=3). The application of verapamil (40 μmol/L) at the end of the experiment abolished high K+-induced contraction (0.5±0.2 mN, P<0.001; Figure 4Ag). These results demonstrate again that Ca2+ release from intracellular stores can be independent of Ca2+ entry but can also be triggered by depolarization itself through coupling to ryanodine and IP3 receptors. When pooling all of the experimental results described above, CdCl2 reduced the contraction strength by approximately 56%±5% (n=33), whereas DHBP together with CdCl2 caused a relative reduction of 75%±5%. By contrast, verapamil almost completely abolished smooth muscle contraction (inhibition by 98%±6%).
Depolarization-induced contraction depends on depolarization-induced Ca2+ release through ryanodine receptors and PLC activation. (A) Consecutive traces of a representative experiment. High K+ (45 mmol/L) evoked a strong contraction that was significantly reduced in solution containing 1 mmol/L CdCl2. Additional application of the ryanodine receptor blocker DHBP (100 μmol/L) further reduced the contraction albeit incompletely. Combined application of CdCl2 and the PLC blocker U 73122 (5 μmol/L) also incompletely reduced the contraction. Application of CdCl2, DHBP and U 73122 caused a significantly stronger reduction of contraction than CdCl2 with DHBP or U 73122 alone. Verapamil abolished the depolarization-induced contraction. (B) Bar graph summarizing 17 experiments (mean±SEM). bP<0.05, cP<0.01.
Depolarization-induced contraction is largely paralleled by intracellular Ca2+ transients
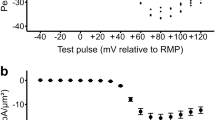
Our findings so far relied on measurements of isometric contraction strength. However, the correlation between the intracellular rise in Ca2+ concentration and contraction strength is uncertain. Thus, we employed FURA-2 recordings in longitudinal smooth muscle cells in situ in order to measure intracellular Ca2+ transients evoked by high K+ bath application. As demonstrated in Figure 5Aa, high K+ solution evoked an increase in intracellular Ca2+ concentration (114.2%±2.3%, n=9). Whereas this increase was significantly reduced in a solution containing 1 mmol/L CdCl2 (103.9%±0.4%, P<0.01, Figure 5Ab), it was almost abolished in a solution containing 40 μmol/L verapamil (101.8%±0.4%, P<0.01 vs CdCl2, Figure 5Ac). These results indicate that inhibition of Ca2+ influx through voltage-gated Ca2+ channels by Cd2+ cannot fully prevent the rise in intracellular Ca2+ concentration. Verapamil, however, showed significantly less Ca2+ transients compared with CdCl2. Hence, these results recapitulate our observations on isometric contraction because the Ca2+ transients with CdCl2 administration was roughly 30% of that obtained in the control situation. Thus, this indicates a parallel reduction of contraction strength with a rise in intracellular Ca2+ concentration in the presence of the Ca2+ channel pore blocker CdCl2.
Depolarization-induced Ca2+ transients are blocked by Cd2+ and verapamil. (A) Consecutive traces of a representative experiment. High K+ (90 mmol/L) evoked a strong increase in intracellular Ca2+ concentration that was significantly blocked in solution containing 1 mmol/L CdCl2 or 40 μmol/L verapamil. Note that the high K+-induced Ca2+ transient in the presence of verapamil was less than that observed in the presence of CdCl2. (B) Image showing longitudinal smooth muscle cells in situ filled with FURA-2AM (excitation wavelength 380 nm). (C) Bar graph summarizing 9 experiments (mean±SEM). bP<0.05, cP<0.01.
Discussion
Role of internal Ca2+ stores in smooth muscle contraction
Smooth muscle contraction is well known to be triggered by a rise in the cytosolic Ca2+ concentration ([Ca2+]i) leading to Ca2+/calmodulin-dependent activation of MLCK, which in turn phosphorylates the 20-kDa light chains of myosin4, 5. This rise in [Ca2+]i can be attained by either Ca2+ entry through VGCCs following depolarization, or through receptor-operated Ca2+ channels following ligand binding. However, additional Ca2+ release from internal Ca2+ stores through Ca2+ release channels appears to be a substantial prerequisite for normal smooth muscle contraction. Thus, we found a 50% reduction in depolarization-induced contraction after the depletion of internal Ca2+ stores with thapsigargin. Moreover, our experiments using Cd2+ ions to block Ca2+ entry into the smooth muscle cells also showed a comparable residual contraction strength that was half the control value. Therefore we conclude that roughly half of the contraction strength in gut smooth muscle is due to Ca2+ entry through Ca2+-permeable channels in the plasma membrane and the other half is due to Ca2+ release from internal stores.
The residual contraction strength with caffeine treatment was only ∼20% of the original amplitude. Interestingly, in addition to activating ryanodine receptors9, 20, 21 caffeine also directly inhibits MLCK18. This probably explains this pronounced reduction in depolarization-induced contraction in the presence of caffeine as compared with thapsigargin alone, which selectively inhibits SERCA22, 23. Thus, caffeine may inhibit all MLCK-dependent and hence Ca2+-dependent mechanisms of smooth muscle contraction. However, there is evidence that these mechanisms may coincide with Ca2+-independent, but Rho kinase-dependent pathways of smooth muscle contraction, which leads to MLCK-independent phosphorylation of myosin-light chain. This is often referred to as Ca2+-sensitization24. Consistent with this idea, the residual contraction strength following caffeine treatment was mirrored by the combined application of CdCl2 with thapsigargin, which abolished Ca2+-dependent mechanisms of smooth muscle contraction. The same holds true for our experiments using CdCl2, DHBP, and 2-APB or U 73122. Interestingly, residual smooth muscle contraction was abolished by verapamil, which only inhibits L-type Ca2+ channels after a large conformational change in the channels19. Therefore, the residual contraction following Cd2+ treatment, which was fully sensitive to verapamil, indicates that Ca2+-independent mechanisms of contraction such as the Rho kinase pathway depend on depolarization-induced conformational changes in L-type Ca2+ channels, but are independent of Ca2+ entry or Ca2+ release. The involvement of additional Ca2+ channel types is unlikely, as the inhibition of T-type, N-type and P/Q-type Ca2+ channels by verapamil occurs at higher concentrations25, 26. Thus, even though T-type and P/Q-type, but not N-type Ca2+ channels are expressed in smooth muscle27, 28, the concentration used in our study probably reflects Ca2+ influx through L-type channels in smooth muscle cells.
Coupling between voltage-gated Ca2+ channels and Ca2+ release
It has been shown in several smooth muscle preparations that Ca2+ ions entering the cell can evoke CICR through direct interaction with ryanodine receptors29, 30. In general, CICR is believed to be related to the cardiac subtype RyR2, whereas direct mechanical coupling has been demonstrated in skeletal muscle between the surface voltage-gate Ca2+ channel Cav1.1 and RyR113. 14, 31, 32. Thus, ryanodine receptors in smooth muscle cells primarily act as intracellular Ca2+ sensors and promote a further increase in [Ca2+]i. In line with this scenario, Ca2+ release through RyRs should be entirely dependent on Ca2+ entry. However, after blocking Ca2+ entry with CdCl2, we obtained a substantial residual contraction of about half of the initial strength. This residual contraction was paralleled by a Ca2+ transient of 30% of the control in a solution containing CdCl2. On the basis of our force measurements, this contraction was caused by Ca2+ release from internal stores because the ryanodine receptor blocker DHBP further reduced this contraction significantly by approximately 70% of the control. But how might voltage-gated Ca2+ channels couple to ryanodine receptors? Smooth muscle cells express all ryanodine receptor subtypes. Among these, the skeletal subtype RyR1 appears to have a significant role in smooth muscle cell function33, 34, 35. Moreover, in airway smooth muscle cells it has recently been shown that the skeletal subtype Cav1.1 may co-localize with RyR136. Thus, it is at least conceivable that in gut smooth muscle cells Cav1.1 may also be functionally present. However, the direct coupling between RyR1 and the predominant smooth muscle VGCC subtype Cav1.2 is still under debate37. Our data support the existence of a coupling mechanism between smooth muscle L-type VGCCs and ryanodine receptors beyond CICR. Further studies are required to elucidate the interconnection between these channels.
In the present study, CdCl2 and DHBP were not able to fully abolish gut smooth muscle contraction. We also observed a significant reduction of contraction by additional inhibition of IP3 receptors. Likewise, inhibition of PLC had the same effect on smooth muscle contraction. From these results we infer that voltage-gated Ca2+ channels couple to G proteins and lead to the PLC-dependent production of IP3, which then acts on IP3-gated Ca2+ release channels at the sarcoplasmic reticulum. Indeed, L-type Ca2+ channels have recently been demonstrated to exhibit metabotropic actions following membrane depolarization. In particular, they appear to be linked to PLC-coupled G proteins enabling IP3-induced Ca2+ release (IICR) from internal stores, which has been termed Ca2+ channel-induced Ca2+ release38, 39. Thus, in addition to the Ca2+ inward current, Ca2+ channels may serve as voltage sensors even in the absence of any Ca2+ influx. Such a mechanism has been found in visceral40, 41 as well as vascular smooth muscle42, 43. Although we could not directly test G protein activation in our preparations, our data at least suggest a metabotropic coupling between L-type Ca2+ channels and IP3-mediated Ca2+ release because DHBP treatment significantly slowed contraction compared with CdCl2 treatment. By contrast, blocking IP3 receptors with 2-APB had no effect itself on peak latencies. This may be interpreted as an induction of fast Ca2+ rise by ryanodine receptors and a significantly slower Ca2+ rise by IP3 receptors, presumably because of the slower kinetics of G protein-dependent and PLC-mediated IP3 production.
Figure 6 summarizes our current knowledge about electromechanical coupling of gut smooth muscle cells. Ca2+ ions entering the cell through VGCC increase cytosolic Ca2+ concentration and also activate CICR through ryanodine receptors (RyR). The cytosolic Ca2+ concentration can be lowered by active transport into internal stores by the sarcoendoplasmic reticulum Ca2+ ATPase (SERCA) or by extrusion out of the cell by the plasma membrane Ca2+ ATPase (PMCA) and the secondarily active Na+-Ca2+-exchanger (NCX), respectively. Caffeine acts as an inhibitor of phosphodiesterase44, 45 and thereby activates SERCA through an increase in cyclic AMP. It also directly inhibits MLCK21. In addition to these well-known cascades, we describe two novel pathways for electromechanical coupling (see dotted arrows). On the one hand, depolarization-dependent activation of voltage-gated Ca2+ channels can open ryanodine receptors without Ca2+ influx and lead to depolarization-induced Ca2+ release (DICR) from internal Ca2+ stores. On the other hand, VGCC activation can cause PLC-dependent IP3 production and Ca2+ release through IP3 receptors. Thus, we conclude that DICR from internal stores, which is independent of Ca2+ entry, is a physiologically relevant mechanism of electromechanical coupling in gut smooth muscle.
Ca2+-induced and depolarization-induced Ca2+ release. This synoptic overview shows the well-known pathways of Ca2+-dependent mechanisms of smooth muscle contraction (black arrows). Thus, Ca2+ entry through L-type voltage-gated Ca2+ channels (VGCC) leads to a rise in cytosolic Ca2+ concentration, which can be enhanced by Ca2+-induced Ca2+ release via ryanodine receptors (RyR), and causes MLCK-dependent contraction. In turn, smooth muscle cells relax when Ca2+ is actively transported into the sarcoplasmic reticulum by SERCA, or when Ca2+ is extruded by the plasma membrane Ca2+ ATPase (PMCA) or by the Na+/Ca2+-exchanger (NCX). The dotted arrows indicate the new pathways demonstrated by the present study. Thus, voltage-dependent conformational changes of VGCCs can directly open RyRs and IP3 receptors without any Ca2+ influx, the latter via PLC activation. bP<0.05, cP<0.01.
Author contribution
Timo KIRSCHSTEIN designed the study, performed research, analyzed data, and wrote the manuscript; Mirko REHBERG performed research, and analyzed data; Rika BAJORAT performed research, analyzed data, and wrote the manuscript; Tursonjan TOKAY performed research, analyzed data, and wrote the manuscript; Katrin PORATH performed research, and analyzed data; Rüdiger KÖHLING designed the study, and wrote the manuscript.
References
Somlyo AP, Himpens B . Cell calcium and its regulation in smooth muscle. FASEB J 1989; 3: 2266–76.
Missiaen L, De Smedt H, Droogmans G, Himpens B, Casteels R . Calcium ion homeostasis in smooth muscle. Pharmacol Ther 1992; 56: 191–231.
Somlyo AP, Somlyo AV . Signal transduction and regulation in smooth muscle. Nature 1994; 372: 231–6.
Colburn JC, Michnoff CH, Hsu LC, Slaughter CA, Kamm KE, Stull JT . Sites phosphorylated in myosin light chain in contracting smooth muscle. J Biol Chem 1988; 263: 19166–73.
Allen BG, Walsh MP . The biochemical basis of the regulation of smooth-muscle contraction. Trends Biochem Sci 1994; 19: 362–8.
Benham CD, Tsien RW . A novel receptor-operated Ca2+-permeable channel activated by ATP in smooth muscle. Nature 1987; 328: 275–8.
Makhlouf GM, Murthy KS . Signal transduction in gastrointestinal smooth muscle. Cell Signal 1997; 9: 269–76.
Berridge MJ . Inositol trisphosphate and calcium signalling. Nature 1993; 361: 315–25.
Guerrero-Hernandez A, Gomez-Viquez L, Guerrero-Serna G, Rueda A . Ryanodine receptors in smooth muscle. Front Biosci 2002; 7: d1676–d1688.
Kotlikoff MI . Calcium-induced calcium release in smooth muscle: the case for loose coupling. Prog Biophys Mol Biol 2003; 83: 171–91.
Kuemmerle JF, Murthy KS, Makhlouf GM . Longitudinal smooth muscle of the mammalian intestine. A model for Ca2+ signaling by cADPR. Cell Biochem Biophys 1998; 28: 31–44.
Bolton TB, Prestwich SA, Zholos AV, Gordienko DV . Excitation-contraction coupling in gastrointestinal and other smooth muscles. Annu Rev Physiol 1999; 61: 85–115.
Rios E, Pizarro G . Voltage sensor of excitation-contraction coupling in skeletal muscle. Physiol Rev 1991; 71: 849–908.
Dulhunty AF . Excitation-contraction coupling from the 1950s into the new millennium. Clin Exp Pharmacol Physiol 2006; 33: 763–72.
Buck E, Zimanyi I, Abramson JJ, Pessah IN . Ryanodine stabilizes multiple conformational states of the skeletal muscle calcium release channel. J Biol Chem 1992; 267: 23560–7.
Rousseau E, Smith JS, Meissner G . Ryanodine modifies conductance and gating behavior of single Ca2+ release channel. Am J Physiol 1987; 253: C364–C368.
Zimanyi I, Buck E, Abramson JJ, Mack MM, Pessah IN . Ryanodine induces persistent inactivation of the Ca2+ release channel from skeletal muscle sarcoplasmic reticulum. Mol Pharmacol 1992; 42: 1049–57.
Ozaki H, Kasai H, Hori M, Sato K, Ishihara H, Karaki H . Direct inhibition of chicken gizzard smooth muscle contractile apparatus by caffeine. Naunyn Schmiedebergs Arch Pharmacol 1990; 341: 262–7.
Awasthi A, Yadav A . Pharmacophoric features and Ca2+ ion holding capacity of verapamil. Bioorg Med Chem Lett 2005; 15: 5412–5.
Luo D, Sun H, Xiao RP, Han Q . Caffeine induced Ca2+ release and capacitative Ca2+ entry in human embryonic kidney (HEK293) cells. Eur J Pharmacol 2005; 509: 109–15.
Morales S, Camello PJ, Mawe GM, Pozo MJ . Characterization of intracellular Ca2+ stores in gallbladder smooth muscle. Am J Physiol Gastrointest Liver Physiol 2005; 288: G507–G513.
Christensen SB, Andersen A, Poulsen JC, Treiman M . Derivatives of thapsigargin as probes of its binding site on endoplasmic reticulum Ca2+ ATPase. Stereoselectivity and important functional groups. FEBS Lett 1993; 335: 345–8.
Poulsen JC, Caspersen C, Mathiasen D, East JM, Tunwell RE, Lai FA, Maeda N, Mikoshiba K, Treiman M . Thapsigargin-sensitive Ca2+-ATPases account for Ca2+ uptake to inositol 1,4,5-trisphosphate-sensitive and caffeine-sensitive Ca2+ stores in adrenal chromaffin cells. Biochem J 1995; 307 ( Pt 3): 749–58.
Murthy KS . Signaling for contraction and relaxation in smooth muscle of the gut. Annu Rev Physiol 2006; 68: 345–74.
Kuga T, Sadoshima J, Tomoike H, Kanaide H, Akaike N, Nakamura M . Actions of Ca2+ antagonists on two types of Ca2+ channels in rat aorta smooth muscle cells in primary culture. Circ Res 1990; 67: 469–80.
Diochot S, Richard S, Baldy-Moulinier M, Nargeot J, Valmier J . Dihydropyridines, phenylalkylamines and benzothiazepines block N-, P/Q- and R-type calcium currents. Pflugers Arch 1995; 431: 10–19.
Andreasen D, Friis UG, Uhrenholt TR, Jensen BL, Skott O, Hansen PB . Coexpression of voltage-dependent calcium channels Cav1.2, 2.1a, and 2.1b in vascular myocytes. Hypertension 2006; 47: 735–41.
Salemme S, Rebolledo A, Speroni F, Petruccelli S, Milesi V . L, P-/Q- and T-type Ca2+ channels in smooth muscle cells from human umbilical artery. Cell Physiol Biochem 2007; 20: 55–64.
Meissner G . Ryanodine receptor/Ca2+ release channels and their regulation by endogenous effectors. Annu Rev Physiol 1994; 56: 485–508.
Fill M, Copello JA . Ryanodine receptor calcium release channels. Physiol Rev 2002; 82: 893–922.
Tanabe T, Beam KG, Powell JA, Numa S . Restoration of excitation-contraction coupling and slow calcium current in dysgenic muscle by dihydropyridine receptor complementary DNA. Nature 1988; 336: 134–9.
Tanabe T, Beam KG, Adams BA, Niidome T, Numa S . Regions of the skeletal muscle dihydropyridine receptor critical for excitation-contraction coupling. Nature 1990; 346: 567–9.
Coussin F, Macrez N, Morel JL, Mironneau J . Requirement of ryanodine receptor subtypes 1 and 2 for Ca2+-induced Ca2+ release in vascular myocytes. J Biol Chem 2000; 275: 9596–603.
Du W, Stiber JA, Rosenberg PB, Meissner G, Eu JP . Ryanodine receptors in muscarinic receptor-mediated bronchoconstriction. J Biol Chem 2005; 280: 26287–94.
Fritz N, Morel JL, Jeyakumar LH, Fleischer S, Allen PD, Mironneau J, Macrez N . RyR1-specific requirement for depolarization-induced Ca2+ sparks in urinary bladder smooth muscle. J Cell Sci 2007; 120: 3784–91.
Du W, McMahon TJ, Zhang ZS, Stiber JA, Meissner G, Eu JP . Excitation-contraction coupling in airway smooth muscle. J Biol Chem 2006; 281: 30143–51.
Essin K, Welling A, Hofmann F, Luft FC, Gollasch M, Moosmang S . Indirect coupling between Cav1.2 channels and ryanodine receptors to generate Ca2+ sparks in murine arterial smooth muscle cells. J Physiol 2007; 584: 205–19.
Valle-Rodriguez A, Lopez-Barneo J, Urena J . Ca2+ channel-sarcoplasmic reticulum coupling: a mechanism of arterial myocyte contraction without Ca2+ influx. EMBO J 2003; 22: 4337–45.
Urena J, Valle-Rodriguez A, Lopez-Barneo J . Metabotropic Ca2+ channel-induced calcium release in vascular smooth muscle. Cell Calcium 2007; 42: 513–20.
Suzuki H, Hirst GD . Regenerative potentials evoked in circular smooth muscle of the antral region of guinea-pig stomach. J Physiol 1999; 517 (Pt 2): 563–73.
van Helden DF, Imtiaz MS, Nurgaliyeva K, von der WP, Dosen PJ . Role of calcium stores and membrane voltage in the generation of slow wave action potentials in guinea-pig gastric pylorus. J Physiol 2000; 524 Pt 1: 245–65.
Itoh T, Seki N, Suzuki S, Ito S, Kajikuri J, Kuriyama H . Membrane hyperpolarization inhibits agonist-induced synthesis of inositol 1,4,5-trisphosphate in rabbit mesenteric artery. J Physiol 1992; 451: 307–28.
Ganitkevich VY, Isenberg G . Membrane potential modulates inositol 1,4,5-trisphosphate-mediated Ca2+ transients in guinea-pig coronary myocytes. J Physiol 1993; 470: 35–44.
Butcher RW, Ho RJ, Meng HC, Sutherland EW . Adenosine 3′,5′-monophosphate in biological materials. II. The measurement of adenosine 3′,5′-monophosphate in tissues and the role of the cyclic nucleotide in the lipolytic response of fat to epinephrine. J Biol Chem 1965; 240: 4515–23.
Butcher RW, Sneyd JG, Park CR, Sutherland EW Jr . Effect of insulin on adenosine 3,5′-monophosphate in the rat epididymal fat pad. J Biol Chem 1966; 241: 1651–3.
Acknowledgements
The authors wish to thank Ulrike Mikkat and Jenny Klostermann for excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kirschstein, T., Rehberg, M., Bajorat, R. et al. High K+-induced contraction requires depolarization-induced Ca2+ release from internal stores in rat gut smooth muscle. Acta Pharmacol Sin 30, 1123–1131 (2009). https://doi.org/10.1038/aps.2009.98
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.98
Keywords
This article is cited by
-
Age-dependent effects of the β3 adrenoceptor agonist CL316,243 on human and rat detrusor muscle strips
Pflügers Archiv - European Journal of Physiology (2024)
-
Influence of lauric acid on the relaxation of corpus cavernosum in streptozotocin-induced diabetic male Wistar rats
Future Journal of Pharmaceutical Sciences (2022)
-
Dandelion extract relaxes mouse airway smooth muscle by blocking VDLCC and NSCC channels
Cell & Bioscience (2020)
-
Involvement of inhibitor kappa B kinase 2 (IKK2) in the regulation of vascular tone
Laboratory Investigation (2018)
-
P2Y receptor-mediated transient relaxation of rat longitudinal ileum preparations involves phospholipase C activation, intracellular Ca2+ release and SK channel activation
Acta Pharmacologica Sinica (2016)