Abstract
Aim:
This study aimed to compare the efficacy and safety between standard and low-dose tirofiban in the treatment of elderly high-risk non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients who underwent percutaneous coronary intervention (PCI).
Methods:
Ninety-four very elderly (≥80 years) high-risk patients with NSTE-ACS were randomly assigned to the standard or the low-dose group. Upstream tirofiban was administered intravenously with a bolus dose of 0.4 μg·kg−1·min−1 over a period of 30 min after the diagnosis had been confirmed, and was followed by a 36−48 h infusion of 0.10 μg·kg−1·min−1 or 0.075 μg·kg−1·min−1. PCI was performed within 24 h of admission. Platelet aggregation inhibition and thrombolysis in myocardial infarction (TIMI) grade flow were assessed. The major adverse cardiac events (MACEs), including death, myocardial infarction, recurrent angina and urgent target-vessel revascularization (TVR), were documented at 7 d, 30 d, and 6 months, and bleeding events were recorded at 7 d.
Results:
Although a significantly higher inhibition of platelet aggregation was observed in the standard-dose group (P<0.05), angiographic PCI success was similar between the two groups (P>0.05). The rate of MACEs was not significantly different at 7 days (2.1% vs 4.4%, P=0.61), 30 days (6.3% vs 8.7%, P=0.71) and 6 months (14.6% vs 17.4%, P=0.71). Major bleeding events were significantly higher in the standard-dose group (10.4% vs 0.0%, P=0.03).
Conclusion:
In very elderly high-risk patients with NSTE-ACS undergoing PCI, low-dose tirofiban offered about the same level of protection from major ischemic events that standard doses did, with less associated bleeding.
Similar content being viewed by others
Introduction
The use of antithrombotic therapies has led to a significant reduction in morbidity and mortality, and several such agents, including aspirin, clopidogrel and heparin, have become the mainstays of treatment for patients with acute coronary syndrome (ACS)1. Treatment with percutaneous coronary intervention (PCI) plus GP IIb/IIIa platelet receptor antagonist has been proven to provide further benefits for high-risk non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients2, 3, 4 and is recommended in recent guidelines5, 6. Although the elderly are known to be at high risk7, they are underrepresented in many clinical trials. Compared with younger patients, the elderly would gain absolute benefits from an early invasive strategy and antithrombotic regimens, but at the cost of increased bleeding8, 9, 10, which has been associated with increased rates of mortality11. GP IIb/IIIa receptor inhibitors (GPI) such as tirofiban have been demonstrated to decrease the number of ischemic events for high-risk ACS patients in several clinical trials2, 3, 4. However, few studies have been conducted to investigate the efficacy and safety of tirofiban in very old patients, and, importantly, further studies are needed to determine the optimal dosing and timing of tirofiban in such patients.
The current study aimed to evaluate the safety and efficacy of standard-dose versus low-dose tirofiban in very elderly (over 80 years) patients with NSTE-ACS who underwent PCI.
Materials and methods
Inclusion and exclusion criteria
Consecutive patients with NSTE-ACS were enrolled into this single-center open-label randomized study from January 2005 to January 2008. Patients were considered eligible for enrollment if they satisfied all of the following criteria: (1) were elderly (age 80 or older); (2) had angina at rest lasting >10 min within 24 h of hospital admission; (3) showed unequivocal changes on ECG during angina: ST-segment depression 0.1 mV or transient ST-segment elevation 0.1 mV in at least 2 contiguous ECG leads; and (4) had coronary arteries with one or more significant lesions suitable for PCI according to coronary angioplasty.
Exclusion criteria were as follows: (1) ST-segment elevation lasting more than 20 min; (2) absence of significant coronary artery disease (CAD) at the angiogram or lesions unsuitable for PCI; (3) relative or absolute contraindications to therapy with aspirin, clopidogrel, or heparin, or known hypersensitivity to any component of tirofiban; (4) concomitant non-cardiac life-threatening disease; (5) severe hemodynamic impairment, cardiogenic shock, or systolic blood pressure of greater than 180 mmHg unresponsive to therapy; or (6) severe renal insufficiency (glomerular filtration rate less than 30 mL/min per 1.73 m2), liver failure, or other serious disease.
Study protocol
When the diagnosis of high-risk NSTE-ACS was confirmed, patients eligible for the study were enrolled and randomized in a 1:1 ratio into the standard-dose group or the low-dose group via a sealed-envelope system. Upstream tirofiban (Wuhan Grand Pharmaceutical Group Co Ltd, China) was administered intravenously with a bolus dose of 0.4 μg·kg−1·min−1 over a period of 30 min and followed by a 36−48 h infusion of 0.10 μg·kg−1·min−1 (in the standard-dose group) or 0.075 μg·kg−1·min−1 (in the low-dose group). All patients underwent PCI within 24 h of admission. Of the 100 patients initially randomized in the study, 3 were excluded at the time of coronary angiography because of three-vessel CAD requiring coronary artery bypass grafting (CABG) (1 in the standard-dose group, 2 in the low-dose group). Another 3 patients were excluded owing to absence of significant CAD at the angiogram (2 in the standard-dose group, 1 in the low-dose group). The infusion of tirofiban was discontinued in patients triaged to CABG surgery. Thus, there were 94 patients in each of the final study groups.
The study protocol was approved by the hospital's ethics committee, and informed written consent was obtained from all patients before catheterization.
Catheterization procedures and medications
PCI was performed according to institutional standards. All coronary angiograms were evaluated by two readers blinded to the clinical status of the patient and the treatment modality. All patients received a loading dose of 300 mg aspirin and 300 mg clopidogrel when tirofiban was administered and were then given 100 mg aspirin and 75 mg clopidogrel every day after PCI. Heparin was given at 40 to 70 U/kg, targeting an activated clotting time of at least 200 s. Enoxaparin (1 mg/kg per 12 h) was administered subcutaneously twice daily after PCI for 5 d.
Angiographic analysis included initial and final TIMI grade flow12. These were performed off-line and by at least 2 blinded independent observers; the TIMI scores were averaged if they were not in agreement.
Laboratory analyses
Creatine kinase-MB (CK-MB) and troponin I (cTnI) levels were measured before and 24 h after PCI. Inhibition of platelet aggregation was measured immediately before the tirofiban bolus and 30 min, 2 h, 6 h, and 24 h after administration of tirofiban. Platelet aggregation was measured by standard light transmission aggregometry using 5 μmol/L adenosine diphosphate as an agonist. Inhibition of platelet aggregation (IPA) was calculated as follows: [(aggregation at baseline-aggregation at time t)/aggregation at baseline]×100.
Endpoints and definitions
The efficacy endpoint was the rate of MACEs, defined as all causes of death, myocardial infarction, recurrent angina and target-vessel revascularization (TVR) at 7 d, 1 month and 6 months of follow-up. The safety endpoint is the incidence of bleeding events at 7 d.
Myocardial infarction (MI) was defined as follows: (1) typical chest pain for longer than 30 min with ECG changes (electrocardiographic ST-segment elevation of 1 mm or greater in 2 or more contiguous electrocardiogram leads, or with new left bundle-branch block) and an elevated CK-MB level or (2) a CK-MB level 3 times the upper limit of normal or a cTnI level above the 99th percentile of the upper reference limit, unaccompanied by chest pain and/or ECG changes. Recurrent ischemia was defined as an ischemic type of discomfort at rest and lasting at least 10 min and is associated with new, horizontal, or downsloping ST-segment deviations. Clinically driven TVR was defined as any CABG surgery or a second PCI of the original target vessel, driven by clinical symptoms of myocardial ischemia with either a positive stress test or electrocardiographic evidence of ischemic changes at rest attributable to the target vessel and the presence of luminal stenosis of more than 70% of the reference luminal diameter by visual estimate. Bleeding (decrease in hemoglobin concentration of at least 3 g/dL or in hematocrit of at least 10%) was classified as major or minor according to the TIMI criteria13. Major bleeding was defined as intracranial bleeding or a decrease in the hemoglobin concentration of 5 g/dL or more or a decrease in hematocrit of 15% or more. Bleeding was considered minor if the hemoglobin concentration decreased by <5 g/dL or the hematocrit decreased by <15%.
Statistical analysis
Assuming a 25% lower total bleeding rate in the low-dose group compared with the standard-dose group, we estimated that 90 patients would provide ≥80% statistical power (1–β≥0.80; α=0.05) to detect such difference. SPSS 12.0 software was used for statistical analysis.
All continuous variables were presented as mean± standard deviation (SD) or median and interquartile range according to their distribution; the Student's t-test was used for variables with a normal distribution and the Wilcoxon rank test was used for variables with a non-normal distribution. Categorical variables were presented as percentages and analyzed by the chi-square test or Fisher's exact test. Kaplan-Meier methods were utilized to estimate endpoints at 7 d, 1 month and 6 months. P values of less than 0.05 were considered statistically significant.
Results
Patient characteristics
The clinical characteristics of the 94 patients enrolled in the study are summarized in Table 1. No statistically significant differences in the baseline distribution of clinical and demographic characteristics between the two groups were found.
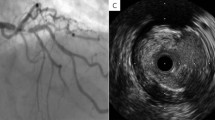
The angiographic characteristics of the patients are shown in Table 2. No significant differences were found in the distribution of the culprit lesion or pre- and post-PCI TIMI-grade flow (TGF) between the two groups. All the patients in the two groups underwent implantation of bare-metal or drug-eluting stents. There was no significant difference in the type of stents between the two groups.
Platelet aggregation testing
Platelet aggregation decreased shortly after tirofiban infusion, with a significantly higher platelet aggregation inhibition in the standard-dose group than in the low-dose group (P<0.05, Figure 1).
Efficacy endpoint
The ischemic events are summarized in Table 3, and the rates of MACEs are shown in Figure 2. The incidence of MACEs was not significantly different between the standard-dose group and the low-dose group at 7 days (2.1% vs 4.4%, P=0.61), at 1 month (6.3% vs 8.7%, P=0.71) and at 6 months (14.6% vs 17.4%, P=0.71).
Safety endpoint
The incidence of major and minor bleeding, bleeding sites, and frequency of transfusion thrombocytopenia are listed in Table 4. The total bleeding rate (29.2% vs 10.8%, P=0.03) and the major bleeding rate (10.4% vs 0%, P=0.03) were significantly higher in the standard group than in the low-dose group. There was no statistically significant difference in minor bleeding events between the two groups.
Discussion
In this single-center study, we compared the efficacy and safety of two different doses of tirofiban on elderly patients with high-risk NSTE-ACS undergoing PCI. A bolus dose of 0.4 μg kg−1·min−1 over a period of 30 min was applied in both groups, but the subsequent maintenance infusion dose varied. To our knowledge, this is the first study to compare different maintenance doses of tirofiban in very elderly people. Our major findings show that, when compared to the standard dose of tirofiban, the low dose provided similar protection from MACEs in very elderly patients with NSTE-ACS who underwent PCI. In addition, the low dose was associated with fewer total bleeding events overall and fewer major bleeding events over 6 months of follow-up.
According to recent guidelines, the use of GPI is strongly recommended in high-risk NSTE-ACS patients when PCI is planned, and eptifibatide or tirofiban is recommended for upstream use (before diagnosis angiography) in these patients. However, in patients not treated upstream, so-called downstream treatments, eptifibatide or abciximab, are recommended instead of tirofiban1, 5, 6. As detailed in these guidelines, tirofiban (bolus dose of 0.4 μg·kg−1·min−1 for 30 minutes, followed by 0.1 μg·kg−1·min−1 of infusion) should be administered before the invasive procedure. The use of tirofiban in patients with ACS further reduces the incidence of death and MI2, 3, 4. However, compared with heparin alone, tirofiban plus heparin increased major and minor bleeding significantly2. In the ACUITY trial15, which compared upstream with downstream approaches, upstream GPI (eptifibatide or tirofiban) initiation before angiography decreased the rate of the composite ischemia endpoint (although not by a statistically significant amount) but resulted in significantly higher rates of major bleeding, minor bleeding, and blood transfusions.
Age is an important determinant of outcomes for patients with ACS. Platelets isolated from older people were more inhibited by antiplatelet therapy16 than those of younger patients. Elderly patients benefit from the invasive strategy of PCI at the cost of an increased number of bleeding events9, 10. In a study designed to evaluate the safety profile of GPI in octogenarians undergoing PCI, the incidence of bleeding and the need for transfusion were higher in the very elderly patients treated with GPI. In NSTE-ACS patients, there is a strong, consistent and dose-related association between bleeding and death11; the mortality was 7.3% in patients with major bleeding compared with 1.1% in patients without major bleeding (RR, 6.71; 95% CI, 4.64−9.71; P<0.001)15. In the clinical reality, guideline-recommended therapies are used less frequently in the elderly17, 18, 19, which is probably based on a generalized consideration of protecting elderly patients from overuse of GPI during invasive interventions. This unjustified treatment paradox prompts an adjustment of the drug dose to maximize the net clinical outcome for the elderly.
Because the coronary anatomy and suitability for PCI are unknown in most patients presenting with ACS, and GPIs decrease adverse events prior to angiography, current guidelines recommend their initiation in patients with ACS either upstream to all patients or selectively in the cardiac catheterization laboratory after angiography has identified those appropriate for PCI, with no clear preference (class I, level of evidence: B). Among the three available GPIs — abciximab, eptifibatide, and tirofiban — only tirofiban is available in China. In our current study, a low dose of tirofiban has been confirmed to yield a net benefit comparable to that of the standard dose, ie, a similar rate of prevention of ischemic events and fewer bleeding events. To obtain more benefit but less risk from the invasive strategy, this adjustment to the standard dose of tirofiban would be more appropriate and practical for elderly patients with high-risk NSTE-ACS in China.
There are several limitations in this study. First, the open-label design may have raised the possibility of bias. We attempted to minimize this potential with the requirement that all ischemic and hemorrhagic events be adjudicated by observers blinded to the treatment assignation. Second, this is a small study, so the results obtained should be further tested in larger randomized blind trials in the future.
Conclusions
In very elderly Chinese patients with high-risk NSTE-ACS, a low dose of tirofiban provides protection from ischemic events similar to that of the standard dose over a 6 month follow-up period, but it significantly reduces the number of major bleeding events.
Author contribution
Yun-lin LIN and Liang-long CHEN designed the research; Yu-kun LUO and Xing-chun ZHENG performed the research; Wei-wei LI analyzed data; Yun-lin LIN and Liang-long CHEN wrote the paper.
References
Harrington RA, Becker RC, Cannon CP, Gutterman D, Lincoff AM, Popma JJ, et al. Antithrombotic therapy for non-ST-segment elevation acute coronary syndromes: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008; 133(6 Suppl): 670S–707S.
Inhibition of the platelet glycoprotein IIb/IIIa receptor with tirofiban in unstable angina and non-Q-wave myocardial infarction. Platelet Receptor Inhibition in Ischemic Syndrome Management in Patients Limited by Unstable Signs and Symptoms (PRISM-PLUS) Study Investigators. N Engl J Med 1998; 338: 1488–97.
Cannon CP, Weintraub WS, Demopoulos LA, Vicari R, Frey MJ, Lakkis N, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med 2001; 344: 1879–87.
Bolognese L, Falsini G, Liistro F, Angioli P, Ducci K, Taddei T, et al. Randomized comparison of upstream tirofiban versus downstream high bolus dose tirofiban or abciximab on tissue-level perfusion and troponin release in high-risk acute coronary syndromes treated with percutaneous coronary interventions: the EVEREST trial. J Am Coll Cardiol 2006; 47: 522–8.
Task Force for Diagnosis and Treatment of Non-ST-Segment Elevation Acute Coronary Syndromes of European Society of Cardiology, Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J 2007; 28: 1598–660.
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol 2007; 50: e1–e157.
Alexander KP, Newby LK, Cannon CP, Armstrong PW, Gibler WB, Rich MW, et al. Acute coronary care in the elderly, part I: Non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation 2007; 115: 2549–69.
Sadeghi HM, Grines CL, Chandra HR, Dixon SR, Boura JA, Dukkipati S, et al. Percutaneous coronary interventions in octogenarians. Glycoprotein IIb/IIIa receptor inhibitors' safety profile. J Am Coll Cardiol 2003; 42: 428–32.
Bach RG, Cannon CP, Weintraub WS, DiBattiste PM, Demopoulos LA, Anderson HV, et al. The effect of routine, early invasive management on outcome for elderly patients with non-ST-segment elevation acute coronary syndromes. Ann Intern Med 2004; 141: 186–95.
Kaehler J, Meinertz T, Hamm CW . Coronary interventions in the elderly. Heart 2006; 92: 1167–71.
Eikelboom JW, Mehta SR, Anand SS, Xie C, Fox KA, Yusuf S . Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation 2006; 114: 774–82.
The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group. N Engl J Med 1985; 312: 932–6.
Rao AK, Pratt C, Berke A, Jaffe A, Ockene I, Schreiber TL, et al. Thrombolysis in myocardial infarction (TIMI) trial-phase I: hemorrhagic manifestations and changes in plasma fibrinogen and the fibrinolytic system in patients treated with recombinant tissue plasminogen activator and streptokinase. J Am Coll Cardiol 1988; 11: 1–11.
Bavry AA, Kumbhani DJ, Rassi AN, Bhatt DL, Askari AT . Benefit of early invasive therapy in acute coronary syndromes: a meta-analysis of contemporary randomized clinical trials. J Am Coll Cardiol 2006; 48: 1319–25.
Stone GW, Bertrand ME, Moses JW, Ohman EM, Lincoff AM, Ware JH, et al. Routine upstream initiation vs deferred selective use of glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: the ACUITY Timing Trial. JAMA 2007; 297: 591–602.
Kimmelstiel C, Badar J, Covic L, Waxman S, Weintraub A, Jacques S, et al. Pharmacodynamics and pharmacokinetics of the platelet GPIIb/IIIa inhibitor tirofiban in patients undergoing percutaneous coronary intervention: implications for adjustment of tirofiban and clopidogrel dosage. Thromb Res 2005; 116: 55–66.
Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J 2005; 149: 67–73.
Alexander KP, Roe MT, Chen AY, Lytle BL, Pollack CV Jr, Foody JM, et al. Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative. J Am Coll Cardiol 2005; 46: 1479–87.
Devlin G, Gore JM, Elliott J, Wijesinghe N, Eagle KA, Avezum A, et al. Management and 6-month outcomes in elderly and very elderly patients with high-risk non-ST-elevation acute coronary syndromes: the Global Registry of Acute Coronary Events. Eur Heart J 2008; 29: 1275–82.
Acknowledgements
We thank Mr Hong-zhi HUANG for language revision.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, Yl., Chen, Ll., Luo, Yk. et al. Benefit of standard versus low-dose tirofiban for percutaneous coronary intervention in very elderly patients with high-risk acute coronary syndrome. Acta Pharmacol Sin 30, 553–558 (2009). https://doi.org/10.1038/aps.2009.38
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.38
Keywords
This article is cited by
-
Safety Profile and Complication Rates in Emergency Off-label Use of Tirofiban in Interventional Neuroradiology
Clinical Neuroradiology (2023)
-
Severe thrombocytopenia and alveolar hemorrhage represent two types of bleeding tendency during tirofiban treatment: case report and literature review
International Journal of Hematology (2012)