Abstract
Aim:
The aim of this study was to test the hypothesis that lower serum sodium may be associated with increased cardiovascular events and all-cause mortality by means of long-term follow-up of subjects with coronary atherosclerosis in a prospective, hospital-based epidemiological study in China.
Methods:
A prospective, hospital-based epidemiological design was used. The study population consisted of 1069 consecutive patients who were scheduled to undergo coronary angiography for suspected or known coronary atherosclerosis. The severity of coronary atherosclerosis was defined using Gensini's score system. Age, sex-adjusted hazard ratios (HR) and 95% confidence intervals (CI) for the quartiles of serum sodium concentration were estimated with Cox proportional hazard models, using quartile 1 as the reference. Cox proportional hazard models were also constructed to estimate the hazard ratios and 95% confidence intervals for all-cause mortality and final end-point events by serum sodium quartile and to adjust for potentially confounding variables. Multivariate models were adjusted for the following variables: age, sex, smoking status, alcohol consumption, body mass index, blood pressure, potassium, chloride, total cholesterol, triglycerides, fasting blood glucose, urea, creatinine, uric acid, and Gensini's score.
Results:
During the median 2.86 years (3011.66 person-years) of follow-up, 176 final end-point events were documented. These events included 79 deaths and 97 readmissions for coronary heart disease. There was a statistically significant inverse association of serum sodium with all-cause mortality (P<0.001). After full adjustment comparing the highest serum sodium quartile to the lowest, there was a non-significant inverse association with all-cause mortality, with an adjusted hazard ratio (95% CI) of 0.67 (0.25–1.80). After adjustment for age and sex, the hazard ratio and 95% CI for final end-point events across increasing quartiles of serum sodium concentration were 1.00, 0.85 (0.59–1.22), 0.52 (0.34–0.82), and 0.31 (0.19–0.49). After full adjustment comparing the highest serum sodium quartile to the lowest, there was a statistically significant inverse association with final end-point events, with an adjusted hazard ratio (95% CI) of 0.46 (0.26–0.81).
Conclusion:
The serum sodium concentration showed a statistically significant negative association with coronary events and all-cause mortality in subjects with coronary atherosclerosis; the actual mechanism underlying this association needs further study.
Similar content being viewed by others
Introduction
Despite 4 decades of declining mortality from cardiovascular disease (CVD) in the United States, CVD remains by far the leading cause of morbidity and mortality1 and it is soon to be the leading cause of morbidity and mortality in the developing world as well2. Government agencies, expert panels and health associations routinely recommend lower sodium intake to reduce blood pressure in order to reduce the risk of cardiovascular disease3, 4.
However, examinations of the relationship between dietary sodium intake and mortality in the National Health and Nutrition Examination Survey (NHANES) I5, II6, and III7 suggested the hypothesis that lower sodium may be associated with increased risk of CVD and all-cause mortality. However, no randomized clinical trial data exist to define the effect of different serum sodium levels on the risk of CVD events or mortality.
In a previous study, we found that the concentration of serum sodium was significantly and negatively associated with the severity of coronary atherosclerosis, as measured by Gensini's score based on coronary angiography8. However, the study could not assess the long-term cardiovascular morbidity and all-cause mortality consequences of lower serum sodium. Of concern is the fact that lower sodium can generate increased activity of the renin-angiotensin and sympathetic nervous systems, as well as increased insulin resistance; each of these could have adverse effects on cardiovascular risk9, 10, 11.
Accordingly, we decided to test the hypothesis that lower serum sodium may be associated with an increased risk of cardiovascular events and all-cause mortality. We conducted long-term follow-up in a prospective, hospital-based epidemiological study in China and also examined evidence for the competing hypothesis that higher serum sodium is associated with increased mortality risk.
Materials and methods
Study design, study sample, and follow-up
A prospective, hospital-based epidemiological design was used to assess the association between serum sodium concentration and the prognosis of subjects with coronary atherosclerosis. This study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University and informed consent was obtained from each patient. The study was conducted in accordance with the principles of the Declaration of Helsinki. The study population consisted of 1432 consecutive patients (1034 males and 398 females) who were to undergo coronary angiography for suspected or known coronary atherosclerosis at the First Affiliated Hospital of Nanjing Medical University in China from 2nd February 2004 to 12th May 2006. Patients with spastic angina pectoris (ie, acetylcholine-positive) were excluded. Patients with infectious processes within 2 weeks before catheterization, heart failure (Killip Class≥2 after acute myocardial infarction), hepatic dysfunction, vascular disease (aortitis treated with prednisolone), familial hypercholesterolemia, thyroid dysfunction, or adrenal dysfunction were also excluded. Among the 1432 subjects, data regarding the potassium, sodium, and chloride concentrations were obtained for 1197 subjects; 235 subjects failed to undergo the measurements. During follow-up, 161 subjects were lost due to a change of telephone number and/or address. Therefore, we excluded 363 subjects who had incomplete data on potassium, sodium, and chloride levels, were lost to follow-up, or both. Thus, the final study cohort consisted of 1069 participants. Among the 1069 subjects, 821 subjects had undergone coronary angiography. However, due to a variety of reasons, 248 subjects failed to undergo coronary angiography.
The follow-up of the aforementioned cohort was conducted in November 2007. The interval time between baseline and follow-up ranged from 1.53 to 3.80 years, and the median follow up time was 2.86 years. In this study, an independent end-point committee evaluated all reported events in order to obtain uniform judgments of major end-points. The end-point committee met regularly and made final decisions about the end-points. The work of the end-point committee was documented on a separate case record form.
The diagnostic criteria for end-points for the purposes of follow-up were as follows: (1) All-cause mortality, including all specified causes as well as unknown causes; (2) readmission for coronary heart disease; (3) definite acute myocardial infarction; and (4) undergoing revascularization of the coronary artery (including percutaneous coronary intervention and coronary artery bypass graft). The final outcome variable in the follow-up was a combination of the above four criteria. Among the 1069 subjects, 53 subjects died from coronary heart disease, 26 subjects died from non-coronary heart disease, and there were a total of 79 death events. A total of 97 subjects were readmitted for coronary heart disease; among these 97 subjects, 42 subjects underwent a revascularization operation and 6 subjects suffered from acute myocardial infarction. Overall, there were 176 final end-point events.
Methods
Coronary angiography Coronary arteries were cannulated using the Judkins technique12 with 5F catheters, and coronary angiography was performed from several projections. The severity of coronary atherosclerosis was defined using Gensini's score system, based on the hypothesis that the severity of coronary heart disease should be considered a product of the functional effects of vascular narrowing and the extent of the area perfused by the involved vessel or vessels. Therefore, Gensini's score was computed by assigning a severity score to each coronary stenosis according to the degree of luminal narrowing and its geographic importance. Reductions in lumen diameter and the roentgenographic appearance of concentric lesions and eccentric plaques were evaluated (reductions of 25%, 50%, 75%, 90%, 99%, and complete occlusion were given Gensini's scores of 1, 2, 4, 8, 16, and 32, respectively). Each principal vascular segment was assigned a multiplier depending on the myocardial area supplied by that segment: left main coronary artery, ×5; proximal segment of left anterior descending coronary artery (LAD), ×2.5; proximal segment of the circumflex artery, ×2.5; mid-segment of the LAD, ×1.5; right coronary artery, distal segment of the LAD, posterolateral artery, or obtuse marginal artery, ×1; and others, ×0.513.
Cigarette smoking and alcohol intake Cigarette smoking and alcohol intake were assessed by means of a standardized questionnaire. Patients' smoking status was classified as either “never smoking” or “smoking” (the latter group included both former and current smokers). Subjects who reported consuming at least 50 g/week of alcohol were considered current drinkers. Alcohol intake status was classified as either “never drinking” or “drinking” (including both former and current drinkers).
Laboratory measurements The 12-h fasting blood samples were drawn in the morning. All laboratory measurements were conducted at the central clinical laboratory of the First Affiliated Hospital of Nanjing Medical University. The concentrations of potassium (mmol/L), sodium (mmol/L), and chloride (mmol/L) were measured with an Ion Selective Electrode Analyzer (Medica EasyLyte PLUS, Bedford, MA, USA). The levels of total cholesterol (mmol/L), triglycerides (mmol/L), fasting blood glucose (mmol/L), urea (mmol/L), creatinine (μmol/L), and uric acid (μmol/L) were determined by enzymatic procedures on an automated autoanalyzer (AU 2700 Olympus, 1st Chemical Ltd, Japan).
Statistical methods
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS for Windows, version 10.0, 1999, SPSS Inc, Chicago, IL). Data on body mass index (BMI) were normally distributed and presented as means±SD, and comparisons were conducted by analysis of variance. However skewed data (including age, blood pressure, potassium, sodium, chloride, total cholesterol, triglycerides, fasting blood glucose, urea, creatinine, uric acid, and Gensini's score) were expressed in median and quartile ranges, and comparisons were conducted using the Kruskal-Wallis H test. For categorical variables such as smoking and drinking status, comparisons between patient groups were conducted by Chi-squared analysis. The Spearman two-way correlation and partial correlation tests were employed to assess the relationship between two quantitative variables.
Age- and sex-adjusted hazard ratios (HR) and 95% confidence intervals (CI) for the quartiles of serum sodium concentration were estimated with Cox proportional hazard models, using quartile 1 as the reference. Cox proportional hazard models were also constructed to estimate the hazard ratios and 95% confidence intervals of all-cause mortality and final end-point events by serum sodium quartile and to adjust for potentially confounding variables. Multivariate models were adjusted for the following variables: age, sex, smoking status, drinking status, body mass index, blood pressure, potassium, chloride, total cholesterol, triglycerides, fasting blood glucose, urea, creatinine, uric acid, and Gensini's score. Interaction product terms of serum sodium with each of the above listed covariates were created and tested, along with the main effects terms in the fully adjusted models.
Results
Baseline characteristics by serum sodium quartile
Table 1 presents the baseline characteristics of the study population, grouped by serum sodium quartile. Almost all characteristics were significantly different between quartiles or nearly so, except for smoking status, drinking status, cholesterol level, urea level, and uric acid level. The low serum sodium quartile group was more likely to be older and male and have a higher glucose level, a higher creatinine level, and a higher Gensini's score. The high serum sodium quartile group was more likely to have a higher body mass index, higher systolic blood pressure, a higher potassium level, and a higher chloride level.
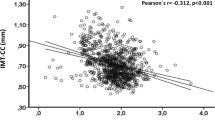
Spearman and partial correlations between sodium concentration and Gensini's score, anthropometric measurements, and biochemical characteristics in patients
Table 2 shows the results of Spearman correlations among serum sodium and Gensini's score, anthropometric measurements, and biochemical characteristics in patients. The results indicated that the concentration of sodium was significantly correlated with age (P<0.001), BMI (P<0.01), SBP (P<0.001), DBP (P<0.01), fasting blood glucose (P<0.001), creatinine (P<0.01), potassium (P<0.01), chloride (P<0.001) and Gensini's score (P<0.001). However, there was no significant correlation of sodium level with total cholesterol, triglycerides, urea, or uric acid.
Because serum sodium is highly correlated with age and gender, and because age and gender are correlated with disease risk, the correlation coefficients between serum sodium and other outcomes should be adjusted for age and gender. Table 3 shows the results of partial correlations among sodium and Gensini's score, anthropometric measurements, and biochemical characteristics of the study population, controlling for age and gender. The results indicated that the concentration of serum sodium is significantly correlated with BMI (P<0.01), SBP (P<0.01), fasting blood glucose (P<0.001), potassium (P<0.001), chloride (P<0.001) and Gensini's score (P<0.001).
Age- and sex-adjusted and multivariate-adjusted hazard ratios for all-cause mortality by serum sodium quartile
During the median 2.86 years (3011.66 person-years) of follow-up, 79 deaths were recorded, among which 53 were related to coronary heart disease and 26 were from other causes. Table 4 provides age- and sex-adjusted and multivariate-adjusted hazard ratios and 95% confidence intervals (CI) for all-cause mortality by serum sodium quartile. There was a statistically significant inverse association of serum sodium with all-cause mortality (P<0.001). After full adjustment comparing the highest serum sodium quartile to the lowest, there was a non-significant inverse association with all-cause mortality, with an adjusted hazard ratio (95% CI) of 0.67 (0.25–1.80).
Age- and sex-adjusted and multivariate-adjusted hazard ratios for final end-point events by serum sodium quartile
During the median 2.86 years (3011.66 person-years) of follow-up, we documented 176 final end-point events. These events included 79 deaths and 97 readmissions for coronary heart disease. Table 5 shows age- and sex-adjusted and multivariate-adjusted hazard ratios and 95% confidence intervals (CI) for final end-point events by serum sodium quartile. After adjustment for age and sex, the hazard ratios and 95% confidence intervals (CI) for final end-point events across increasing quartiles of serum sodium concentration were 1.00, 0.85 (0.59–1.22), 0.52 (0.34–0.82), and 0.31 (0.19–0.49). After full adjustment comparing the highest sodium serum quartile to the lowest, there was a significant inverse association of serum sodium with final end-point events, with an adjusted hazard ratio (95% CI) of 0.46 (0.26–0.81).
Discussion
The present study indicates that the concentration of serum sodium is significantly and negatively associated with the severity of coronary atherosclerosis, as measured by Gensini's score based on coronary angiography. During the median 2.86 years (3011.66 person-years) of follow-up, there was a statistically significant inverse association of serum sodium with all-cause mortality (P<0.001). After full adjustment comparing the highest serum sodium quartile to the lowest, there was a significant inverse association of serum sodium with the final end-point events, and the adjusted hazard ratio (95% CI) was 0.46 (0.26–0.81). Therefore, we confirmed the hypothesis that lower serum sodium may be associated with increased cardiovascular events and all-cause mortality over long-term follow-up in China. To the best of our knowledge, this is the first study directly linking sodium concentration to subsequent morbidity and mortality in subjects with coronary atherosclerosis. These findings conflict with widely held popular belief, but they may be consistent with the biologically plausible hypothesis.
Under normal conditions, serum sodium concentrations are maintained within the narrow range of 135-145 mmol/L despite great variation in water and salt intake. Sodium and its accompanying anions, principally chloride and bicarbonate, account for 86% of extracellular fluid osmolality, which is normally 285–295 mosm/kg. Blood pressure is the most powerful predictor of stroke and other cardiovascular events. The importance of salt (sodium chloride) intake in determining blood pressure and the incidence of hypertension is well established. Furthermore, randomized controlled clinical trials of moderate reductions in salt intake show a dose-dependent cause-effect relationship and lack of a threshold effect within the usual levels of salt intake in populations worldwide14. The effect is independent of age, sex, ethnic origin, baseline blood pressure, and body mass index. However, in the present study, the associations between lower serum sodium and increased cardiovascular events and all-cause mortality are significant when adjusted for blood pressure and other risk factors. Prospective studies15, 16, 17, 18 indicate that higher salt intake predicts the incidence of cardiovascular events. Although widespread support exists for reducing salt intake to prevent cardiovascular disease, the lack of large and long-term randomized trials on the effects of salt intake reduction on clinical outcomes has encouraged some people to argue against a policy of salt intake reduction in populations6.
Observed associations of lower sodium with higher mortality in the Third National Health and Nutrition Examination Survey (NHANES III) were modest and mostly insignificant. These findings also suggest that higher sodium is unlikely to be independently associated with higher CVD or all-cause mortality in the general US adult population7. The data from the present study are consistent with the hypothesis that lower serum sodium is associated with increased cardiovascular disease and all-cause mortality, and the observed associations reached statistical significance. Sodium restriction is one of the most widely publicized non-pharmacological recommendations for cardiovascular disease prevention. The data here cannot sustain a conclusion that lower sodium is harmful. However, these findings, along with the inconsistent results of other epidemiological studies, do not lend support to any universal prescription for salt intake. More likely, optimal sodium intake will vary based upon genetic, behavioral, and environmental circumstances.
The mechanism that may account for the relationship between serum sodium level and the subsequent morbidity and mortality of subjects with coronary atherosclerosis remains unknown. However, at the baseline of the study, the serum concentration of sodium was significantly and negatively correlated with age, fasting blood glucose, creatinine, and Gensini's score. The above-mentioned variables were also risk factors for coronary atherosclerosis and prognosis. Another reason that may accounts for the inverse relationship between the prognosis of subjects with coronary atherosclerosis and their sodium level was the activation of the renin-angiotensin system (RAS). The sodium depletion observed in patients with greater coronary disease risk may be a cause or a consequence of renin-angiotensin system (RAS) activation. Activation of the RAS may exert numerous adverse effects on the cardiovascular system19. Under normal circumstances, the RAS modulates volume and vasoconstriction to maintain pressure. As part of this physiologic process, there is an inverse relation between sodium intake and activity of the RAS. Thus, a 100 mmol/24 h reduction in sodium intake generates a threefold increase in plasma renin activity — a measure of RAS activity20. Although this mechanism is appropriate to sustain BP, an elevated RAS also has adverse effects on the vascular endothelium and smooth muscle cells and stimulates inflammatory agents. The net result is atherogenic21.
A limitation of the present study is that the subjects were from one center rather than multiple centers, which may result in selective bias; however, the large sample size of this study may have minimized this bias. Because human blood sodium levels fluctuate, the other limitation is that we only measured blood sodium level on admission, and the patients' urinary sodium level and sodium intake level were not measured. Therefore, the clinical significance of the findings in the present study requires further investigation.
In sum, the data are consistent with the hypothesis that lower serum sodium may be associated with an increased risk of cardiovascular events and all-cause mortality. These conclusions were obtained from long-term follow-up of a prospective hospital-based epidemiological cohort in China. However, the actual mechanism underlying the association needs further study. Furthermore, the results raise questions regarding the likelihood that a survival advantage will result from a universal recommendation for lower dietary sodium intake.
Conflict of interest
The authors have no financial conflict of interest to disclose.
Author contribution
En-zhi JIA conducted the data analysis; Zhen-xia XU contributed to the drafting of the paper; Zhi-jian YANG designed the study. Tie-bing ZHU, Lian-sheng WANG, Bo CHEN, Ke-jiang CAO, Jun HUANG, Wen-zhu MA, and Xiang LU collected the data.
References
American Heart Association. Heart disease and stroke statistics: 2005 Update. Dallas, Tex: American Heart Association; 2004.
Murray CJL, Lopez AD . Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet 1997; 349: 1498–504.
Joint National Committee for the Prevention, Detection, Evaluation, and treatment of High Blood Pressure. The Seventh Report of the Joint National Committee for the Prevention, Detection, Evaluation, and treatment of High Blood Pressure (JNC VII). JAMA 2003; 289: 2560–72.
Pearson TA, Blair SN, Daniels SR, Eckel RH, Fair JM, Fortmann SP, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 Update: consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. American Heart Association Science Advisory and Coordinating Committee. Circulation 2002; 106: 388–91.
Alderman MH, Cohen H, Madhavan S . Dietary sodium intake and mortality: National Health and Nutrition Examination Survey (NHANES I). Lancet 1998; 351: 781–5.
Cohen HW, Hailpern SM, Fang J, Alderman MH . Sodium intake and mortality in the NHANES II follow-up study. Am J Med 2006; 119: 275e7–14.
Cohen HW, Hailpern SM, Alderman MH . Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III). J Gen Intern Med 2008; 23: 1297–302.
Jia EZ, Yang ZJ, Zhu TB, Wang LS, Chen B, Cao KJ, et al. Serum sodium concentration is significantly associated with the angiographic characteristics of coronary atherosclerosis. Acta Pharmacol Sin 2007; 28: 1136–42.
Alderman MH, Madhavan S, Ooi WL, Cohen H, Sealey JE, Laragh JH . Association of the rennin-sodium profile with the risk of myocardial infarction in patients with hypertension. N Engl J Med 1991; 324: 1098–104.
Grassi G, Dell'Oro R, Seravalle G, Foglia G, Trevano FQ, Mancia G . Short- and long-term neuroadrenergic effects of moderate dietary sodium restriction in essential hypertension. Circulation 2002; 106: 1957–61.
Petrie JR, Morris AD, Minamisawa K, Hilditch TE, Elliott HL, Small M, et al. Dietary sodium restriction impairs insulin sensitivity in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 1998; 83: 1552–7.
Judkins MP . A percutaneous transfemoral technique. Radiology 1967; 89: 815–21.
Gensini GG . A more meaningful scoring system for determinating the severity of coronary heart disease. Am J Cardiol 1983; 51: 606.
He FJ, MacGregor GA . How far should salt intake be reduced? Hypertension 2003; 42: 1093–9.
Sasaki S, Zhang XH, Kesteloot H . Dietary sodium, potassium, saturated fat, alcohol and stroke mortality. Stroke 1995; 26: 783–9.
He J, Ogden LG, Vupputuri S, Bazzano LA, Loria C, Whelton PK . Dietary sodium intake and subsequent risk of cardiovascular disease in overweight adults. JAMA 1999; 282: 2027–34.
Tuomilehto J, Jousilahti P, Rastenyte D, Moltchanov V, Tanskanen A, Pietinen P, et al. Urinary sodium excretion and cardiovascular mortality in Finland: a prospective study. Lancet 2001; 357: 848–51.
Nagata C, Takatsuka N, Shimizu N, Shimizu H . Sodium intake and risk of death from stroke in Japanese men and women. Stroke 2004; 35: 1543–7.
Grote K, Drexler H, Schieffer B . Renin-angiotensin system and atherosclerosis. Nephrol Dial Transplant 2004; 19: 770–3.
Graudal NA, Gallie AM, Gared P . Effects of sodium restriction on blood pressure, rennin, aldosterone, catecholamines, cholesterols, and triglyceride — a meta analysis. JAMA 1998; 279: 1383–91.
Dzau VJ . Tissue angiotensin and pathobiology of vascular disease-A unifying hypothesis. Hypertension 2001; 37: 1047–52.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No 30400173).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Jia, Ez., Xu, Zx., Yang, Zj. et al. Association of serum sodium concentration with coronary atherosclerosis in China: follow-up study. Acta Pharmacol Sin 30, 494–500 (2009). https://doi.org/10.1038/aps.2009.17
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.17