Abstract
Aim:
To explore the action of doxorubicin on vascular smooth muscle cells.
Methods:
Isometric tension of denuded or intact thoracic aortic vessels was recorded and [Ca2+]i in isolated aortic smooth muscle cells was measured by using Fluo-3.
Results:
Doxorubicin induced phasic and tonic contractions in denuded vessels and increased levels of [Ca2+]i in single muscle cells. Treatment with 10 μmol/L ryanodine had no effect on basal tension, but it did abolish doxorubicin-induced phasic contraction. Treatment with 10 mmol/L caffeine induced a transient phasic contraction only, and the effect was not significantly altered by ryanodine, the omission of extracellular Ca2+ or both. Phenylephrine induced rhythmic contraction (RC) in intact vessels. Treatment with 100 μmol/L doxorubicin enhanced RC amplitude, but 1 mmol/L doxorubicin abolished RC, with an increase in maximal tension. Caffeine at 100 μmol/L increased the frequency of the RC only. In the presence of 100 μmol/L caffeine, however, 100 μmol/L doxorubicin abolished the RC and decreased its maximal tension. Treatment with 10 μmol/L ryanodine abolished the RC, with an increase in the maximal tension. In Ca2+-free solution, doxorubicin induced a transient [Ca2+]i increase that could be abolished by ryanodine pretreatment in single muscle cells. The doxorubicin-induced increase in [Ca2+]i was suppressed by nifedipine and potentiated by ryanodine and charybdotoxin.
Conclusion:
Doxorubicin not only releases Ca2+ from the sarcoplasmic reticulum but also promotes the entry of extracellular Ca2+ into vascular smooth muscle cells.
Similar content being viewed by others
Introduction
Doxorubicin, an anticancer drug, has been proven to be able to bind to Ca2+ release channels (ryanodine receptors, RyRs) of the sarcoplasmic reticulum (SR) of myocardium and to cause dual (stimulatory or inhibitory) effects on the contraction and transient [Ca2+]i of cardiac myocytes depending on the [Ca2+]i loading of the myocyte, the frequency of electrical stimulation, the temperature, and the concentration of doxorubicin 1, 2, 3, 4, 5, 6, 7. In vascular smooth muscle cells, a study performed with skinned rabbit mesenteric smooth muscle fibers has demonstrated that doxorubicin in the micromolar range can elicit a release of Ca2+ from the SR and a concomitant vasoconstriction, essentially similar to its effect on skinned skeletal muscle cells8. Moreover, an experimental study with aortas taken from rats chronically treated with low doses of doxorubicin has demonstrated that the contractile response to norepinephrine of thoracic aortic vessel is significantly attenuated, suggesting that doxorubicin at clinical dosage can affect vascular smooth muscle function9. Therefore, further investigating the effects of doxorubicin on vessel contraction and [Ca2+]i change in vascular smooth muscle cells will help to understand its toxicity in the cardiovascular system.
Rhythmic contraction (RC) in isolated vessels has been observed in physiological and pathophysiological conditions, although clarification of the functional roles in physiology and pathophysiology still remains a challenge. Studies on RC have been undertaken for more than 150 years10, 11, 12, 13, after the first report by Jones regarding the veins of bats' wings in 185211. To date, the mechanism of RC is still not very clear, and plenty of cellular components of the vascular smooth muscle cell have been reported to participate in generating RC; these include RyR and the Ca2+-pump of SR, the L-type Ca2+ channel, the K+ channel, Na+, K+-ATPase and the nitric oxide (NO)-cGMP system. Moreover, the mechanism of RC generation displays slight variations in different vascular beds or species12, 13, 14, 15. In a previous study, Jiang et al found that an α-adrenergic receptor agonist, phenylephrine (PE), can evoke spontaneous RC in isolated intact aortas of C57BL/6 mice, and that this PE-induced RC is related to RyR of the SR of vascular smooth muscle cells10.
In the present study, we used fresh isolated aortic vessel rings and single cells to investigate the effects of doxorubicin on vessel tension and [Ca2+]i elevation. PE-induced RC was also compared to address the effects of doxorubicin on RyR of the SR of vascular smooth muscle cells.
Materials and methods
Animals and tissue preparation
Male C57BL/6 mice were anaesthetized with an intraperitoneal injection of sodium pentobarbital (150 mg/kg) together with sodium heparin (100 IU/kg, ip), to prevent intravascular coagulation. The thoracic aorta was quickly dissected free and placed in Krebs Henseleit solution, which consisted of (in mmol/L): NaCl 118, KCl 4.7, CaCl2 2.5, KH2PO4 1.2, MgSO4 (7 H2O) 1.2, NaHCO3 25.2 and glucose 11.1. By means of a dissecting microscope, adhering perivascular tissue was carefully removed, and the descending thoracic aorta was cut into 2 mm-long rings. All experiments complied with national guidelines and were approved by the Institutional Animal Care and Use Committee.
Tension measurement
The vessel rings with or without endothelium were mounted onto two thin stainless steel holders, one of which was connected to a force displacement transducer and the other to a movable device that allowed the application of passive tension from 550 to 600 mg, a range that was determined to be the optimal resting tension for obtaining maximal active tension induced by a 60 mmol/L K+ solution. The mounted rings were kept in 2-mL organ baths containing the Krebs Henseleit solution, kept at 37 °C and continuously bubbled with a gas mixture of 95% O2 and 5% CO2 to maintain a pH of 7.4. The isometric tension was recorded and analyzed by a data acquisition and analysis system (BL-420E+, Chengdu Technology & Market Corp). After an equilibration period of 60 min, the contractile function of the vessel was tested twice by replacing the Krebs Henseleit solution with 60 mmol/L K+ solution that was prepared by exchanging NaCl with an equimolar amount of KCl, and the second contraction was taken as the reference contraction. Prolonged exposure to 10 μmol/L phenylephrine (PE) evoked spontaneous rhythemic contraction (RC), which was recorded at approximately 15 min. The amplitude of RC was measured as the mean of the last three oscillations and expressed as a percentage of the maximal tension. Each drug was studied on thoracic aortic segments from at least 4 mice.
Vascular smooth muscle cell preparation
The thoracic aortic segments obtained by the above method were placed in ice-cold modified Ca2+-free physiological salt solution (PSS) containing (in mmol/L) NaCl 55, sodium glutamate 80, KCl 5.6, HEPES 10, MgCl2 2, and glucose 10. The vessel was opened longitudinally, and the smooth muscle layer was obtained by tearing out adherent adventitia under a dissection microscope. Then the smooth muscle layer was cut into many scraps and incubated in a plastic tube with Ca2+-free PSS containing type IA collagenase 2 g/L, papain 0.5 g/L, ovalbumin 5 g/L, and 1,4-dithiothreitol 1.75 g/L, at 37 °C for 35 min. After being washed twice in Ca2+-free PSS for 10 min, the tissue masses were dispersed with a Pasteur pipette using gentle up-down force, and the cell suspension was kept at 4 °C.
Measurement of [Ca2+]i
In order to measure [Ca2+]i, the cells were seeded onto the coverslip of the 2-mL chamber, and 20 min later they were incubated in Ringer's solution (in mmol/L) NaCl 135, KCl 5.6, MgCl2 1, CaCl2 2, HEPES 10, and glucose 10, pH 7.4 with NaOH containing 5 μmol/L acetoxymethyl ester of Fluo-3 and 2.5 mg/L pluronic acid for 20 min16. Consequently, the fluorescence was scanned with a Leica TCS SP2 laser-scanning confocal microscope (Leica Microsystems AG, Germany), and the average fractional fluorescence (F/F0) of the acquisition area (5 s) was measured ratiometrically (488:520 nm) using an LCS quantitative fluorescence measurement program (Leica Confocal Software, Germany) at room temperature (22–23 °C). Only the spiral-shaped and well-attached cells were selected for the experiment.
Drugs
Type IA collagenase, papain, ovalbumin, phenylephrine, doxorubicin, caffeine, nifedipine, charybdotoxin (Sigma Chemical, St Louis, MO, USA), ryanodine (Wako Pure Chemical Industries, Japan), acetoxymethyl ester of Fluo-3, and pluronic acid (Molecular Probes, Eugene, USA) were dissolved in distilled water or Ca2+-free PSS. All subsequent dilutions were made with Krebs Henseleit solution. Similar dilutions of the solvents into the Krebs Henseleit solution were used as controls and had no effect on either the basal tension or the evoked tension of the vessel. All concentrations given are the final molar concentrations in the organ chambers.
Statistics
Data were expressed as means±SEM. The two-tailed paired-samples t-test was used to compare results in treated and untreated aortas, and the two-tailed independent samples t-test was used to compare the results in different groups. Differences were considered significant with a value of P<0.05. In [Ca2+]i measurements, n represents the number of experiments.
Results
Effects of doxorubicin, ryanodine, and caffeine on vasomotion in denuded aortic vessels
Doxorubicin 10 μmol/L induced a small contraction (8±1.0 mg, n=4 from 4 mice), but 100 μmol/L doxorubicin induced a large two-phase contraction, ie, an initial phasic contraction (21.2±2.1 mg, n=6 from 5 mice) and a later tonic contraction (40±5.6 mg, n=6 from 5 mice, Figure 1B) in denuded aortic vessels. In a different experimental group, in which the denuded vessels were pretreated with 10 μmol/L ryanodine for 10 min, there was no significant induction of contraction per se; the initial phasic contraction was abolished but the later tonic contraction that was induced by 100 μmol/L doxorubicin increased robustly (406±38 mg, n=6 from 6 mice, P>0.01 vs 100 μmol/L doxorubicin alone, Figure 1C). However, replacement of the physiological bath solution with Ca2+-free bath solution had no significant effect on the initial phasic contraction (19±2.4 mg, n=6 from 5 mice, P>0.05), but it did abolish the later tonic contraction induced by 100 μmol/L doxorubicin (Figure 1D). Furthermore, pretreatment of the denuded vessels with 10 μmol/L ryanodine in Ca2+-free bath solution abolished both the phasic contraction and the tonic contraction induced by 100 μmol/L doxorubicin (Figure 1E).
The contraction induced by doxorubicin in denuded thoracic aortic vessels. (A) control without any treatment; (B) 100 μmol/L doxorubicin induced two-phase contraction; (C) pretreatment of vessels with 10 μmol/L ryanodine for 10 min abolished initial phasic contraction but strongly increased later tonic contraction induced by 100 μmol/L doxorubicin. The scale in (C) is special for the later contraction behind the dashed line; (D) in Ca2+-free bath solution, 100 μmol/L doxorubicin induced only the initial phasic contraction; (E) pretreatment of vessels with 10 μmol/L ryanodine in Ca2+-free bath solution cancelled doxorubicin-induced two-phase contraction.
Treatment with 10 mmol/L caffeine induced a transient contraction only (223±18 mg, n=6 from 6 mice), and this effect was not significantly affected by removal of Ca2+ from the bath solution (230±21mg, n=6 from 6 mice), pretreatment of the denuded vessels with 10 μmol/L ryanodine (236±24 mg, n=6 from 6 mice), or both (225±19 mg, n=6 from 5 mice; Figure 2).
The contraction induced by caffeine in denuded thoracic aortic vessels. (A) 10 mmol/L caffeine induced a transient phasic contraction; (B) pretreatment of vessels with 10 μmol/L ryanodine for 10 min or (C) Ca2+-free bath solution or both (D) did not significantly affect caffeine-induced transient phasic contraction.
Effects of doxorubicin, caffeine, and ryanodine on PE-induced RC in intact aortic vessels
Spontaneous RC occurred 3−5 min after exposure to 10 μmol/L PE in intact aortas. Approximately 10 min after PE-induced RC, administration of 100 μmol/L doxorubicin significantly enhanced the amplitude of PE-induced RC and also resulted in a transient decrease in maximal tension (Figure 3A and Table 1). Furthermore, this increased amplitude of PE-induced RC was below the maximal tension before doxorubicin treatment. Therefore, the vessel tension spent more time below the maximal tension. In other words, doxorubicin at a 100 μmol/L concentration just enhanced vessel relaxation. In another group, 1 mmol/L doxorubicin abolished PE-induced RC while notably enhancing the maximal tension (Figure 3B, Table 1).
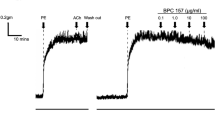
In caffeine group experiments, approximately 10 min after the occurrence of PE-induced RC in the intact aortic vessels, administration of 100 μmol/L caffeine did not significantly affect the amplitude of PE-induced RC, and it slightly increased the maximal tension, possibly due to the release of Ca2+ from the SR; however, it increased its frequency notably (from 1.01±0.17 to 1.58±0.15 per minute, n=6 from 6 mice; Figure 4A). Thirty minutes after washing out the caffeine, repeated application of PE elicited RC similar to that before the administration of caffeine (Figure 4B). In another experimental group, pretreatment of the intact vessels with 100 μmol/L caffeine for 10 min accelerated the occurrence of PE-induced RC, and subsequent administration of 100 μmol/L doxorubicin abolished PE-induced RC and significantly diminished its maximal tension (Figure 4C, Table 1).
The effects of caffeine on PE-induced RC in intact thoracic aortic vessels. (A) 100 μmol/L caffeine increased the frequency of PE-induced RC; (B) PE-induced RC after washout of caffeine described in (A) in the same vessel; (C) 100 μmol/L doxorubicin abolished PE-induced RC and significantly inhibited its maximal tension.
In the ryanodine group experiments, approximately 10 min after the occurrence of PE-induced RC in the intact aortic vessels, administration of 10 μmol/L ryanodine induced dual effects on PE-induced RC: the amplitude of PE-induced RC, a measure of capacity to improve vessel relaxation, was temporarily enhanced at first (from 11.6±1.2 to 17.3±2, n=6 from 6 mice, P<0.05), and then PE-induced RC was abolished (Figure 5A and Table 1). Furthermore, in another group, pretreatment with 10 μmol/L ryanodine also abolished PE-induced RC (dashed line shown in Figure 5C). Thirty minutes after washout, the vessel tension returned to baseline, and repeated application of PE significantly augmented the amplitude of PE-induced RC; however, this enhanced RC was not found in the parallel control group (Figure 5B). This enhanced RC resulted in the vessel tension spending more time below maximal tension, therefore enhancing vessel relaxation (Figure 5C and Table 1).
The effects of ryanodine on PE-induced RC in intact thoracic aortic vessels. (A) 10 μmol/L ryanodine initially enhanced the amplitude of PE-induced RC and then abolished it; (B) PE-induced RC of the parallel control for (C) in a different vessel; (C) the dashed line shows that 10 μmol/L ryanodine abolished PE-induced RC. Thirty minutes after washout of ryanodine, repeated application of PE strikingly augmented the amplitude of PE-induced RC.
Doxorubicin increases cell [Ca2+]i
To further investigate the effect of doxorubicin on vascular smooth muscle cells, we employed [Ca2+]i measurement with fast Ca2+ indicator Fluo-3/AM in freshly isolated aortic smooth muscle cells of mice. Figures 6A and B show that 10 μmol/L doxorubicin induced a small [Ca2+]i elevation, and 100 μmol/L doxorubicin significantly enhanced [Ca2+]i in the aortic smooth muscle cells. Exposure of the cells to 10 μmol/L ryanodine for 10 min strongly enhanced doxorubicin-induced Ca2+ influx (Figure 6C). When the cells were presented in Ca2+-free solution, doxorubicin only induced a transient elevation of [Ca2+]i (Figure 6D). With pretreatment of the cells with 10 μmol/L ryanodine in Ca2+-free solution, the doxorubicin-induced increase in [Ca2+]i was abolished (Figure 6E).
The effects of doxorubicin on [Ca2+]i of isolated aortic vascular smooth muscle cells. (A and B) 10 and 100 μmol/L doxorubicin induced sustained [Ca2+]i increases; (C) with pretreatment of the cells with 10 μmol/L ryanodine for 10 min, initial transient [Ca2+]i was inhibited and the later increase in [Ca2+]i was enhanced; (D) in Ca2+-free bath solution, 100 μmol/L doxorubicin only induced an initial increase in transient [Ca2+]i; (E) pretreatment of the cells with 10 μmol/L ryanodine in Ca2+-free bath solution abolished the increase in [Ca2+]i induced by 100 μmol/L doxorubicin. Data are shown as means±SEM (on average five experiments, with each one including 10−20 cells from 4−5 mice).
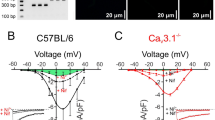
Considering the linkage between RyR, Ca2+-activated K+ (KCa) channels, and voltage-dependent Ca2+ channels, the corresponding inhibitors were used to verify involvement in the doxorubicin-induced increase in [Ca2+]i. The cells were pretreated with the voltage-dependent Ca2+ channel inhibitor nifedipine (1 μmol/L) for 10 min. Treatment with 100 μmol/L doxorubicin was still capable of inducing an initial transient and later sustained increases in [Ca2+]i, but the later maximal [Ca2+]i increase was notably suppressed compared with the increase with doxorubicin treatment alone (Figure 7A). More interestingly, in another group, pretreatment with KCa channel inhibitor charybdotoxin (ChTX, 100 nmol/L) markedly enhanced the doxorubicin-induced increase in [Ca2+]i in vascular smooth muscle cells (Figure 7B).
The effects of nifedipine and charybdotoxin on doxorubicin-induced [Ca2+]i increases in isolated aortic vascular smooth muscle cells. (A) Pretreatment with 1 μmol/L nifedipine for 10 min suppressed the increase in [Ca2+]i induced by 100 μmol/L doxorubicin; (B) 100 nmol/L charybdotoxin (ChTX) enhanced the increase in [Ca2+]i induced by 100 μmol/L doxorubicin. Data are shown as means±SEM (on average four experiments, with each one including 10−20 cells from 4 mice).
Discussion
[Ca2+]i concentration is an important factor for the initiation and control of the contraction of vascular smooth muscle, and it is regulated by both the entry of extracellular Ca2+ through voltage-dependent Ca2+ channels and Ca2+-permeable non-selective cation channels such as transient receptor potential (TRP) channels on the cell membrane and the release of Ca2+ from SR. The Ca2+ released from SR seems to be mainly contributed to initial phasic contraction, while the Ca2+ that enters through voltage-dependent Ca2+ channels and/or Ca2+-permeable non-selective cation channels on the cell membrane contributes to later tonic contraction17, 18, 19.
In the present study, 100 μmol/L doxorubicin was shown to induce both phasic and tonic contractions in the denuded vessels. Treatment with 100 μmol/L doxorubicin was also shown to increase the [Ca2+]i of the aortic smooth muscle cells as measured by the application of Fluo-3, which is consistent with the results from the vasomotion experiments. Furthermore, doxorubicin-induced two-phase contractions and [Ca2+]i elevation were notably blocked by ryanodine and omission of Ca2+ from the bath solution, respectively. In addition, doxorubicin-induced [Ca2+]i elevation was also suppressed by a voltage-dependent Ca2+ channel inhibitor and reversely potentiated by blocking RyR and KCa channels. Taken together, these results indicate that doxorubicin is capable of inducing Ca2+ release from SR and promoting extracellular Ca2+ influx. Interestingly, the later effect of doxorubicin has also been observed in myocardium2.
Unlike treatment with doxorubicin (100 μmol/L), 10 mmol/L caffeine induced only a transient contraction in the denuded vessels, either in normal bath solution or in Ca2+-free bath solution, and its effects were not significantly affected by ryanodine (10 μmol/L). These phenomena imply that caffeine does not directly influence extracellular Ca2+ influx.
Among the three agents examined in the present study, 10 μmol/L ryanodine failed to induce both vessel contraction and an increase in the transient [Ca2+]i of the cells. The data from previous studies indicate that the effects of ryanodine on vessel contraction and transient [Ca2+]i are determined by at least three factors, ie, the type of vessel, the basal tension of the vessel, and the concentration of ryanodine. Significant ryanodine-induced vessel contraction and/or increase in transient [Ca2+]i have been observed in dog cerebral arteries with basal tone at 1−100 μmol/L20, in fetal rabbit distal (but not proximal) pulmonary artery smooth muscle cells at 50 μmol/L21, and in rat femoral arteries at 30 nmol/L−30 μmol/L22; the absence of an effect of ryanodine on vessel contraction and/or transient [Ca2+]i has been shown in the ferret portal vein at a dose of 10 μmol/L17, in the aorta of C57BL/6 mice at 10 μmol/L10, and in rat aortas at 10 μmol/L23. Therefore, one should be very cautious to compare the effects of ryanodine on the vasomotion and/or transient [Ca2+]i of cells and to explain the interaction between ryanodine and other inhibitors of RyRs in different vascular smooth muscles.
In vascular smooth muscle cells, three types of RyR isoforms, RyR1, RyR2, and RyR3, have been identified so far24, and experimental data show that RyR1 and RyR2 contribute to Ca2+ release underlying a single spark, whereas RyR3 down-regulates the activity of RyR1 and RyR2 by controlling the basal Ca2+ frequency24, 25. Moreover, growing evidence demonstrates that [Ca2+]i released from the SR of vascular smooth muscle cells contributes not only to the regulation of contraction but also to the regulation of relaxation. Ca2+-dependent relaxation is mediated by discretely localized Ca2+ release events through RyR channels in the SR of the cells. These local increases in Ca2+ concentration in close proximity to the cell membrane, termed sparks, stimulate nearby KCa channels, causing spontaneous transient outward K+ currents, the hyperpolarizing currents that close voltage-dependent Ca2+ channels and decrease global [Ca2+]i and vasoconstriction26, 27. An earlier study demonstrates that PE-induced RC is a good model for indirect observation of Ca2+-dependent relaxation10. Therefore, in this study, we compared the effects of doxorubicin on PE-induced RC with those of ryanodine and caffeine.
Depending on concentration, ryanodine exhibits two opposite effects on RyR channels. In the range of nanomolar to micromolar, ryanodine activates RyR channels, inducing Ca2+ release from SR; however, at higher concentrations, (micromolar to millimolar), ryanodine may block RyR channels, inhibiting Ca2+ release28. The data from this study showed that 10 μmol/L ryanodine abolished PE-induced RC, as observed in earlier studies10, 13. Surprisingly, after washout of ryanodine, repeated administration of PE elicited much greater RC to enhance vessel relaxation than that of the previous application of PE in the absence of ryanodine. These phenomena imply that: (1) ryanodine, at very high concentrations of 10 μmol/L, blocks all subtypes of RyRs equally so that the Ca2+ sparks in the cells and RC of the vessel do not occur in the presence of ryanodine24; (2) after washout of raynodine with normal solution, a residual effect of ryanodine modifies RyR1-2 to be more sensitive to Ca2+. Repeated application of PE after washout of ryanodine therefore induces more Ca2+ release from the SR and subsequently enhances the opening of KCa channels and relaxation of the vessel. A recent study has demonstrated that ryanodine is able to increase the sensitivity of RyR2 to Ca2+ activation by approximately 1000-fold28.
As observed in rat aortas13, our results showed that 100 μmol/L caffeine did not influence the amplitude of PE-induced RC but increased its frequency and that, after washing out the caffeine, repeated administration of PE elicited RC similar to that of the previous application of PE in the absence of caffeine; this suggests that caffeine, unlike ryanodine, may only activate RyR1-2 but does not change their sensitivity to Ca2+. An earlier study targeting RyR3 by the application of the antisense oligonucleotides has demonstrated that the deletion of RyR3 does not affect caffeine-induced responses in the vascular smooth muscle cells29.
Because PE-induced RC is directly related to Ca2+ release from SR, the finding that 100 μmol/L doxorubicin enhanced the amplitude of PE-induced RC to improve vessel relaxation in association with a transient decrease in the maximal tension suggests that 100 μmol/L doxorubicin mainly promotes Ca2+ release from SR to regulate PE-induced RC. By contrast, 1 mmol/L doxorubicin abolished PE-induced RC, with an increase in the maximal tension, implying that 1 mmol/L doxorubicin perhaps induced extracellular Ca2+ entry strongly and inhibited PE-induced RC owing to a higher vessel contraction effect. Furthermore, the finding that 100 μmol/L doxorubicin abolished PE-induced RC and inhibited the maximal tension in the presence of 100 μmol/L caffeine indicates that doxorubicin has a synergic effect with caffeine to impair/deplete Ca2+ stores. Together, these data imply that doxorubicin may only activate RyR1-2 with caffeine. It is definitely necessary to probe the differences in receptor type and affinity for the three agents in future studies
The results of our study show that the mechanism by which doxorubicin moderates [Ca2+]i is complicated. Even when voltage-dependent Ca2+ channels were inhibited with nifedipine, 100 μmol/L doxorubicin was still able to stimulate an initial transient and to sustain later increases in [Ca2+]i. Moreover, if the Ca2+ store was depleted by thapsigargin, an inhibitor of SR Ca2+ ATPase, doxorubicin could still induce an increase in [Ca2+]i (data not shown). These findings indicate that doxorubicin can also induce Ca2+ influx by activating Ca2+-permeable non-selective cation channels besides voltage-dependent Ca2+ channels. On the one hand, it is well known that non-selective cation channels can also permeate monovalent Na+ ions to depolarize the membrane. On the other hand, to date, there is no evidence showing that doxorubicin can directly activate voltage-dependent Ca2+ channels. Thus, it is possible that doxorubicin indirectly activates voltage-dependent Ca2+ channels by enhancing non-selective cation channels, leading to membrane depolarization. Our data also show that doxorubicin-induced [Ca2+]i increases were markedly enhanced if the cells were pretreated with 10 μmol/L ryanodine or ChTX. The results suggest that 100 μmol/L doxorubicin may stimulate RyR channels to activate KCa channels, inducing membrane repolarization via close voltage-dependent Ca2+ channels. This pathway forms a negative feedback loop to avoid higher [Ca2+]i loading. However, at very high concentrations of doxorubicin, Ca2+ influx will have a dominant effect, leading to a huge increase in [Ca2+]i. Indeed, further work is needed to clarify the mechanism of doxorubicin's effects on [Ca2+]i in vascular smooth muscle cells.
In conclusion, 100 μmol/L doxorubicin induced both phasic and tonic contractions of the vessels by enhancing initial and later [Ca2+]i; these effects were abolished by ryanodine and the deletion of Ca2+ from the bath solution, respectively. These results indicate that doxorubicin is able to induce Ca2+ release from the SR of vascular smooth muscle cells and promote the entry of extracellular Ca2+ via voltage-dependent Ca2+ channels and non-selective cation channels. The mechanism by which doxorubicin triggers Ca2+ release from the SR of vascular smooth muscle cells is completely different from that of ryanodine or caffeine because both rynaodine and caffeine only act on the SR, without inducing Ca2+ entry, and rynaodine has dual effects on RyR channels. In addition, the present study indicates that vasoconstrictor-induced RC is a useful model for the indirect observation of changes in the activity of the SR.
Author contribution
Bing SHEN, Kai-he YE, Chun-ling YE, and Jia-hua JIANG designed the study; Bing SHEN, Kai-he YE, and Lan ZHUANG performed the experiments; Bing SHEN, Kai-he YE, Chun-ling YE analyzed the data; Bing SHEN and Jia-hua JIANG wrote the manuscript.
References
Jiang J, Temma K, Akera T . Doxorubicin-induced changes in intracellular Ca2+ transients observed in cardiac myocytes isolated from guinea-pig heart. Can J Physiol Pharmacol 1994; 72: 622–31.
Matsushita T, Okamato M, Toyama J, Kodama I, Ito S, Fukutomi T, et al. Adriamycin causes dual inotropic effects through complex modulation of myocardial Ca2+ handling. Jpn Circ J 2000; 64: 65–71.
Ondrias K, Borgatta L, Kim DH, Ehrlich BE . Biphasic effects of doxorubicin on the calcium release channel from sarcoplasmic reticulum of cardiac muscle. Circ Res 1990; 67: 1167–74.
Saeki K, Obi I, Ogiku N, Shigekawa M, Imagawa T, Matsumoto T . Doxorubicin directly binds to the cardiac-type ryanodine receptor. Life Sci 2002; 70: 2377–89.
Temma K, Akera T, Akihito C, Ozawa S, Kondo H . Cellular Ca2+ loading and inotropic effects of doxorubicin in atrial muscle preparations isolated from rat or guinea-pig hearts. Eur J Pharmacol 1994; 252: 173–81.
Temma K, Chugun A, Akera T, Hara Y, Sasaki T, Kondo H . Ca2+ overloading causes the negative inotropic effect of doxorubicin in myocytes isolated from guinea-pig hearts. Eur J Pharmacol 1997; 322: 235–42.
Temma K, Chugun A, Hara Y, Sasaki T, Kondo H . Biphasic positive inotropic actions of doxorubicin in isolated guinea pig hearts: relation to Ca2+ release from the sarcoplasmic reticulum. Gen Pharmacol 1999; 33: 229–36.
Kanmura Y, Raeymaekers L, Casteels R . Effects of doxorubicin and ruthenium red on intracellular Ca2+ stores in skinned rabbit mesenteric smooth-muscle fibres. Cell Calcium 1989; 10: 433–9.
Dalske HF, Hardy K . Effect of low-dose doxorubicin on calcium content and norepinephrine response in rat aorta. Eur J Cancer Clin Oncol 1988; 24: 979–83.
Jiang J, Thorén P, Caligiuri G, Hansson GK, Pernow J . Enhanced phenylephrine-induced rhythmic activity in the atherosclerotic mouse aorta via an increase in opening of KCa channels: relation to Kv channels and nitric oxide. Br J Pharmacol 1999; 128: 637–46.
Jones TW . Discovery that the veins of the bat's wing are endowed with rhythmical contractility and that onward flow of blood is accelerated by each contraction. Phil Trans R Soc Lond 1852; 131: 136.
Shen B, Ye CL, Ye KH, Liu JJ, Sun P, Jiang JH . Mechanism underlying enhanced endothelium-dependent vasodilatation in thoracic aorta of early stage streptozotocin-induced diabetic mice. Acta Pharmacol Sin 2003; 24: 422–8.
Gustafsson H, Nilsson H . Rhythmic contractions of isolated small arteries from rat: role of calcium. Acta Physiol Scand 1993; 149: 283–91.
Gustafsson H, Nilsson H . Rhythmic contractions in isolated small arteries of rat: role of K+ channels and the Na+, K+-pump. Acta Physiol Scand 1994; 150: 161–70.
Gustafsson H, Mulvany MJ, Nilsson H . Rhythmic contractions of isolated small arteries from rat: influence of the endothelium. Acta Physiol Scand 1993; 148: 153–63.
Porter VA, Bonev AD, Knot HJ, Heppner TJ, Stevenson AS, Kleppisch T, et al. Frequency modulation of Ca2+ sparks is involved in regulation of arterial diameter by cyclic nucleotides. Am J Physiol 1998; 274: C1346–55.
Abe F, Karaki H, Endoh M . Effects of cyclopiazonic acid and ryanodine on cytosolic calcium and contraction in vascular smooth muscle. Br J Pharmacol 1996; 118: 1711–6.
Asano M, Nomura Y . Ca2+ movement from leaky sarcoplasmic reticulum during contraction of rat arterial smooth muscles. Eur J Pharmacol 2000; 404: 327–39.
Hisayama T, Takayanagi I, Okamoto Y . Ryanodine reveals multiple contractile and relaxant mechanisms in vascular smooth muscle: simultaneous measurements of mechanical activity and of cytoplasmic free Ca2+ level with Fura-2. Br J Pharmacol 1990; 100: 677–84.
Asano M, Kuwako M, Nomura Y, Suzuki Y, Shibuya M, Sugita K, et al. Possible mechanism of the potent vasoconstrictor responses to ryanodine in dog cerebral arteries. Eur J Pharmacol 1996; 311: 53–60.
Porter VA, Reeve HL, Cornfield DN . Fetal rabbit pulmonary artery smooth muscle cell response to ryanodine is developmentally regulated. Am J Physiol 2000; 279: L751–7.
Kojima M, Dohi Y, Sato K . Ryanodine-induced contraction in femoral artery from spontaneously hypertensive rats. Eur J Pharmacol 1994; 254: 159–65.
Shima H, Blaustein MP . Modulation of evoked contractions in rat arteries by ryanodine, thapsigargin, and cyclopiazonic acid. Circ Res 1992; 70: 968–77.
Lohn M, Jessner W, Furstenau M, Wellner M, Sorrentino V, Haller H, et al. Regulation of calcium sparks and spontaneous transient outward currents by RyR3 in arterial vascular smooth muscle cells. Circ Res 2001; 89: 1051–7.
Jiang D, Xiao B, Li X, Chen SR . Smooth muscle tissues express a major dominant negative splice variant of the type 3 Ca2+ release channel (ryanodine receptor). J Biol Chem 2002; 278: 4763–9.
Jaggar JH, Wellman GC, Heppner TJ, Porter VA, Perez GJ, Gollasch M, et al. Ca2+ channels, ryanodine receptors and Ca2+-activated K+ channels: a functional unit for regulating arterial tone. Acta Physiol Scand 1998; 164: 577–87.
Perez GJ, Bonev AD, Patlak JB, Nelson MT . Functional coupling of ryanodine receptors to KCa channels in smooth muscle cells from rat cerebral arteries. J Gen Physiol 1999; 113: 229–38.
Masumiya H, Li P, Zhang L, Chen SR . Ryanodine sensitizes the Ca2+ release channel (ryanodine receptor) to Ca2+ activation. J Biol Chem 2001; 276: 39727–35.
Coussin F, Macrez N, Morel JL, Mironneau J . Requirement of ryanodine receptor subtypes 1 and 2 for Ca2+-induced Ca2+ release in vascular myocytes. J Biol Chem 2000; 275: 9596–603.
Acknowledgements
This project was supported by the National Natural Science Foundation of China (No 30070873).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shen, B., Ye, Cl., Ye, Kh. et al. Doxorubicin-induced vasomotion and [Ca2+]i elevation in vascular smooth muscle cells from C57BL/6 mice. Acta Pharmacol Sin 30, 1488–1495 (2009). https://doi.org/10.1038/aps.2009.145
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.145
Keywords
This article is cited by
-
Doxorubicin alters G-protein coupled receptor-mediated vasocontraction in rat coronary arteries
Naunyn-Schmiedeberg's Archives of Pharmacology (2024)
-
GLP-1 receptor activation and Epac2 link atrial natriuretic peptide secretion to control of blood pressure
Nature Medicine (2013)