Abstract
Aim:
Cobratoxin (CTX), the long-chain α-neurotoxin from Thailand cobra venom, has been demonstrated to have analgesic action in rodent pain models. The present study evaluated the anti-inflammatory and anti-nociceptive effects of CTX on adjuvant arthritis (AA) in rats.
Methods:
Arthritis was induced by injection of complete Freund's adjuvant (CFA) in rats. Paw swelling and hyperalgesia of AA rats were measured at various times after CFA administration. Tumor necrosis factor-α (TNF-α), interleukin-1 (IL-1), interleukin-2 (IL-2) and interleukin-10 (IL-10) levels in serum were determined with ELISA. Histopathological changes in synoviocytes were examined under a microscope. Involvement of the cholinergic system in the effects of CTX was examined by pretreatment of animals with the α7 nicotinic receptor (α7-nAChR) antagonist methyllycaconitine (MLA).
Results:
CFA induced marked paw swelling and reduced thresholds of mechanical and cold-induced paw withdrawal. The levels of TNF-α, IL-1 and IL-2 in the serum of AA rats were increased, whereas the level of IL-10 was decreased. Histopathological examination of synoviocytes showed pronounced inflammation and accumulation of collagen. The administration of CTX (17.0 μg/kg, ip) significantly reduced paw swelling and mechanical and thermal hyperalgesia. CTX also reduced the production of TNF-α, IL-1, and IL-2 but increased the production of IL-10 and altered pathohistological changes. The analgesic and anti-inflammatory efficacy of CTX was significantly reduced by MLA (3 mg/kg, sc).
Conclusion:
These results indicate that CTX has a beneficial effect on CFA-induced arthritis by modulating the production of inflammatory cytokines. α7-nAChR appears to mediate the anti-nociceptive and anti-inflammatory actions of CTX.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a systemic inflammatory disorder that affects approximately 1% of the population worldwide. It is characterized by joint swelling, synovial membrane inflammation and cartilage destruction. The severity and disease progression of RA are governed by multiple factors including immune, genetic and environmental factors 1, 2. Multiple components of immunity and inflammation play a role in the onset and progression of the disease, including T and B lymphocytes, neutrophils, monocytes and the vascular endothelium.
Several lines of recent evidence have suggested that proinflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-1 (IL-1) play a pivotal role in the pathogenesis of RA because they are increased in the synovial tissue, synovial fluid and serum of RA patients. IL-1 and TNF-α contribute to synoviocyte self-proliferation and increase the production of tissue enzymes such as matrix metalloproteinases via chondrocytes and synovial cells, resulting in cartilage degradation 3, 4, 5. In the process of bone erosion, TNF-α triggers the production of other cytokines and endothelial adhesion molecules, stimulates collagenase and induces osteoclast differentiation 6. Furthermore, TNF-α exerts its arthritogenic potency through the induction of IL-1. Therefore, IL-1, IL-2, and TNF-α have been shown to be dominant players in the induction of inflammation and bone erosion 7, 8. In fact, anti-TNF-α antibodies and soluble TNF-α receptors have been proven to be effective in ameliorating RA 9.
Snake venom, which contains small basic peptides, phospholipase A2 (PLA2), and PLA2 homologs, has a significant effect on RA. Studies have shown that the Bothrops atrox venom peptide, batroxobin, caused a significant decrease in the fibrinogen level, whereas it had no effect on paw swelling 10. Crotalus durissus terrificus venom, which contains crotoxin as a major active component, administered subcutaneously before or after subplantar injection of carrageenan into the mouse right hind paw significantly inhibited edema and migration of polymorphonuclear cells to the peritoneal cavity 11, 12. Cobra venoms contain high levels of neurotoxins that target nicotinic acetylcholine receptors. Cobratoxin (CTX), a long-chain curaremimetic toxin from Thailand cobra venom, is composed of about 71 amino acids. The characteristic structure of CTX is a polypeptide chain organized in three major loops emerging like the fingers of a hand from a “palm” knotted together by the five disulfide bonds 13, 14. CTX has significant affinity for neuronal nicotinic acetylcholine receptor (nAChR) containing the alpha7 subunit 15, 16, 17. Alpha7 nicotinic acetylcholine receptors (α7-nAChR) are localized mainly presynaptically in the peripheral nervous system and also have high-affinity sites within the brain. It is also known that α7-nAChR can conduct Ca2+ ions, thereby directly impacting neurotransmitter release 18. A previous study found that CTX exhibited a dose-dependent analgesic action in mice as determined by both the hot-plate and the acetic acid writhing tests. The analgesic effects of CTX were antagonized by atropine, but not naloxone. These results indicated that CTX produced potent opioid-independent analgesia 19. Recently, we also found that CTX exhibited a dose-dependent analgesic action in formalin-induced phase 1 and phase 2 pain responses and inhibited enhancement of c-Fos-positive cells in the spinal cord (Liu et al., manuscript submitted). However, its anti-inflammatory potential remains to be determined.
The present study, therefore, was designed to examine whether ip administration of CTX has anti-inflammatory effects in the rat adjuvant arthritis model, induced using complete Freund's adjuvant (CFA). In order to reveal the immunological influences of CTX, the serum levels of TNF-α, IL-1, IL-2, and IL-10 were measured and the histopathological changes in the joints of these AA rats were investigated. Furthermore, the involvement of the cholinergic system in the effect of CTX was examined by pretreatment of animals with methyllycaconitine (MLA), an α7-nAChR antagonist.
Materials and methods
Animals
Male Sprague-Dawley rats weighing 180–220 g were purchased from the Experimental Animal Center of Soochow University. The animals were fed ad libitum and housed in a room with a controlled ambient temperature (22±2 °C), humidity (50%±10%), and a 12-h light/dark cycle. Animals were acclimated to the housing conditions and handled for 3–4 days before experiments. All experiments were performed between 08:00 AM and 4:00 PM. All experimental procedures were conducted according to the NIH Guidelines for the Care and Use of Laboratory Animals (NIH Publications No 80–23, revised 1996). The experimental protocols were approved by the Local Committee on Animal Care and Use at Soochow University.
Reagents
CTX (99% pure), provided by ReceptoPharm (Plantation, FL, USA), was dissolved in saline and administered ip at doses of 8.5 and 17.0 μg/kg. ELISA kits for TNF-α, IL-1, IL-2, and IL-10 were all purchased from Boster Biological Technology (Wuhan, China). CFA and methyllycaconitine (MLA) were purchased from Sigma.
Induction of arthritis
Male Sprague-Dawley rats were used in this study. Knee joint inflammation was induced by an intra-articular injection of 100 μL CFA. As a control, 100 μL of saline was injected. Procedures were performed under anesthesia with sodium pentobarbital (50 mg/kg, ip). The circumference of the knee joint was measured using a flexible tape meter.
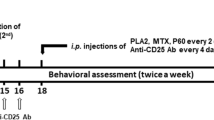
CTX treatments
CTX (8.5, 17.0 μg/kg) or saline (control) was administered ip. To study the effects of CTX on phase Ι (first inflammatory reaction) in AA rats, CTX (8.5, 17.0 μg/kg) or saline was administered once daily for 3 d before administration of CFA. The last dose of CTX was administered 3 h before treatment with CFA. To study the effects of CTX or saline on the phase II response (secondary inflammatory reaction) in AA rats, CTX (8.5, 17.0 μg/kg) was administered for 9 d (began at the 11th and ended at the 19th day) after the administration of CFA. MLA (3.0 mg/kg), dissolved in 0.9% saline and prepared freshly on the days of the experiment, was injected s.c. 2 h after the last injection of CTX. The dose of MLA was selected based on previous studies known to block α7-nAChR 20, 21.
Nociceptive behavioral tests
Mechanical paw withdrawal tests Rats were placed under a clear plastic cage on an elevated plastic mesh floor (1 cm2 perforations) and were allowed to acclimate for 15 min before testing. Calibrated Von Frey monofilaments (North Coast Medical Co, USA) were used to deliver punctuated mechanical stimuli of varying intensities to the plantar surface of both hindpaws. Withdrawal response thresholds (g) for each hindpaw were determined using the up-down method described by Chaplan and colleagues 22. Each stimulus was applied for a duration of 1–2 s, with an interstimulus interval of 5 s. Care was taken to stimulate random locations on the plantar surface. Only robust and immediate withdrawal responses from the stimulus were counted. The mechanical force (in grams) applied by monofilament that produced a 50% withdrawal response was recorded as the threshold.
Cold plate test For assessment of hyperalgesia to cold stimulus in AA rats, a cold plate Analgesia Meter (homemade experimental device with temperature maintained at 2 °C) was used. Latency was defined as the length of time after the rats were placed on a cold plate (2 °C) before a hind paw began to shake. In all situations, the right paw injected with CFA reacted first.
Measurement of serum levels of TNF-α, IL-1, IL-2 and IL-10
The concentrations of TNF-α, IL-1, IL-2, and IL-10 in serum were determined with ELISA kits. On day 19 after CFA injection, rats were anesthetized with sodium pentobarbital (50 mg/kg, ip). Blood was collected and stored at 4 °C for 30 min and then centrifuged at 3 000×g for 10 min. Supernatant was collected and stored at -20 °C until analysis. The levels of TNF-α, IL-1, IL-2, and IL-10 were determined using a commercially available enzyme immunoassay kits (Boster Biological Technology, Wuhan, China). Measurement was completed using an enzyme-linked immunosorbent assay with an absorbency maximum at 450 nm.
Assessment of synovial membrane pathology
On day 19 after CFA injection, rats were killed for dissection of their synovial membranes. Specimens were fixed for 6 h in 4% glutaraldehyde in PBS, decalcified and returned to 30% sucrose solution and submitted to routine paraffin embedding. Tissue sections were stained using hematoxylin and eosin (HE) or van Gieson's stain (VG).
Statistical analysis
Unless stated otherwise, data are expressed as means±SD and evaluated using ANOVA. Analysis of variance for repeated measurement was used where applicable. The post hoc test was also used with Student's Newman Keuls test when appropriate. P<0.05 was considered statistically significant. Calculations were performed using the SPSS 10.0 statistical package.
Results
Effects of CTX on edema in the hind paw of adjuvant-induced arthritic rats
Figure 1 shows the measurements of circumference of knee joints after the administration of CFA. The CFA-injected paw remained swollen for more than 19 days. The curves of edema plotted against time could be divided into two phases. In the first phase, edema increased and reached a peak 3 days after CFA injection. Edema slowly subsided until the 9th day, when the paw began to swell again, and reached a second peak on the 11th day. Pre-treatment (3 d prior to CFA) or post-treatment (started on the 11th day after CFA) with CTX (17.0 μg/kg, ip) significantly reduced CFA-induced paw edema compared with the group treated with CFA+saline.
Effects of pre- and post-treatment with CTX on paw edema induced by CFA. Rats were treated with CTX (8.5, 17.0 μg/kg, ip) or saline once daily for 3 days before administration of CFA once daily for 9 days from the 11th to the 19th days after CFA injection. Paw edema was determined by measuring the circumference of the paw using a flexible tape measure 6, 18, and 24 h after CFA injection. Data represent the mean±SD (n=6). cP<0.01 compared with saline group; eP<0.05, fP<0.01 compared with saline+CFA-treated group. (A) pre-treatment with CTX once per day for 3 days before injection of CFA. (B) post-treatment with CTX for 9 days from the 11th day to the 19th day after CFA injection.
For pre-treatments with CTX, edema was inhibited by 43% and 12% at 6 h (CTX 17.0 μg/kg and 8.5 μg/kg, respectively) and by 22% and 15% at 18 h (CTX 17.0 μg/kg and 8.5 μg/kg, respectively; Figure 1A). In phase II of CFA-induced adjuvant arthritis, CTX was administered on days 11-19 after the injection of CFA. There was a significant difference between the CTX- and saline-treated groups on the 11th and 19th day post-CFA. The most significant inhibition of CFA-induced edema (by 47% reduction) was observed on the 11th day after CFA administration (Figure 1B).
Effects of CTX on hyperalgesia in adjuvant-induced arthritic rats
CFA induced marked mechanical hyperalgesia, as evidenced by reduced nociceptive thresholds 11–19 days after CFA administration. This CFA-induced mechanical hyperalgesia was inhibited by post-treatment with CTX (17.0 μg/kg, ip, once daily from the 11th to the 19th day after CFA injection; Figure 2A).
Effects of CTX on hyperalgesia in AA rats. Rats were treated with CTX (17.0 μg/kg, ip) once daily for 9 days from the 11th to the 19th day after CFA injection. Hyperalgesia was determined using Von Frey's Filaments test and a cold plate test. Data represent the mean±SD (n=6). bP<0.05, cP<0.01 compared to saline group; eP<0.05, fP<0.01 compared to saline+CFA-treated group. (A) Von Frey's Filaments test; (B) Cold plate test.
CFA also induced marked thermal hyperalgesia, as evidenced by reduced paw withdrawal latency, compared with the control group 11–19 days after administering CFA. CTX greatly increased paw withdrawal latency (Figure 2B). These results indicate that CTX inhibits arthritic pain.
Effects of CTX treatment on levels of cytokines in AA rats
A significant increase in the concentrations of the proinflammatory cytokines IL-1, IL-2, and TNF-α occurred in the serum of arthritic animals on the 19th day after CFA treatment (Figures 3A–C). Post-treatment with CTX (17.0 μg/kg, ip, starting on the 11th and ending on the 19th day after CFA) had a marked inhibitory effect on the expression of cytokines induced by CFA. However, serum IL-10 concentration decreased compared with that of saline control rats after CFA treatment. Post-treatment with CTX significantly reversed the CFA-induced decline in IL-10 (Figure 3D).
Effects of post-treatment with CTX on cytokine levels in the serum of AA rats. Rats were treated with CTX (17.0 μg/kg, ip) once daily for 9 days from the 11th to the 19th day after CFA injection. On day 19 after CFA injection, the rats were anesthetized with sodium pentobarbital (50 mg/kg, ip), and blood was collected. The concentrations of TNF-α, IL-1, IL-2, and IL-10 in serum were determined with ELISA kits. Data represent the mean±SD (n=6). bP<0.01 compared with saline group; eP<0.05 compared with saline+CFA-treated group.
Effects of CTX on histopathology of synovium in AA rats
Histopathological analysis of the synovium of AA rats using HE staining showed clear inflammatory cell infiltration, edema and pannus formation. These abnormalities were significantly alleviated in AA rats after the administration of CTX (once daily from the 11th to the19th day after CFA; Figures 4A–4C). Furthermore, VG staining showed marked hyperplastic cartilage, which was significantly inhibited by the administration of CTX (once daily from the 11th to the 19th day after CFA; Figures 4D–4F).
Effects of post-treatment with CTX on histological alterations of synovium. Rats were treated with CTX (17.0 μg/kg, ip) once daily for 9 days from the 11th to the 19th day after CFA injection. On day 19 after CFA injection, rats were killed and synovial membranes were removed. Tissue sections were stained with hematoxylin and eosin (HE) or van Gieson's stain (VG). (A) Saline group: normal articular cartilage and absence of infiltrate in the synovium (HE stain, ×400); (B) Saline+CFA-treated group: marked infiltration of inflammatory cells and pannus formation (HE stain, ×100); (C) CTX+CFA-treated group: minor infiltration of inflammatory cells (HE stain, ×100); (D) Saline group: normal collagen (VG stain, ×100); (E) Saline+CFA-treated group: hyperplastic collagen in the synovium (VG stain, ×100); (F) CTX+CFA-treated group: decreased hyperplastic collagen (VG stain, ×100).
Effects of MLA on CTX's anti-inflammatory action in AA rats
To show that CTX's anti-inflammatory activity is mediated by the nicotinic cholinergic system, MLA (3.0 mg/kg, sc), an α7-nAChR antagonist, was administered 2 h after the injection of CTX, and CFA-induced paw edema was assessed 6–42 h after CFA administration. When used alone, MLA (3.0 mg/kg, sc) had no effect (11%) on CFA-induced paw edema, whereas CTX alone significantly inhibited CFA-induced paw edema in rats 42 h after CFA treatment (39% reduction). MLA antagonized the inhibitory effects of CTX on CFA-induced paw edema (Figures 5A and B). These results indicate that MLA could inhibit CTX's anti-inflammatory action.
Effects of MLA on CTX's anti-inflammation effects (A) and CFA-induced paw edema (B) in AA rats. Rats were treated with CTX (17.0 μg/kg, ip) or saline once daily for 3 days before the administration of CFA. MLA (3.0 mg/kg) or saline was given 2 h after the injection of CTX. Paw edema was determined by measuring the circumference of the paw using a flexible tape measure 6, 24, and 42 h after CFA injection. Data represent the mean±SD of 6 rats. cP<0.01 vs saline group; eP<0.05, fP<0.01 vs saline+CFA-treated group.
Effects of MLA on CTX's anti-nociceptive effects in AA rats
Rats were treated with CTX (17.0 μg/kg, ip) or saline once daily for 3 days before administration of CFA. CFA induced marked mechanical hyperalgesia, as evidenced by reduced nociceptive thresholds compared with saline groups at 6, 24, and 42 h after administration of CFA. This CFA-induced mechanical hyperalgesia was inhibited by CTX (17.0 μg/kg, ip). MLA (3.0 mg/kg) did not affect mechanical hyperalgesia induced by CFA, but it did robustly inhibit the effects of CTX's anti-nociceptive effect in rats at 6 h, 24 h, and 42 h after CFA administration (Figures 6A and 6B).
Effects of MLA on CTX's anti-nociceptive effects (A) and CFA-induced mechanical hyperalgesia (B) in AA rats. Rats were treated with CTX (17.0 μg/kg, ip) or saline once daily for 3 d before the administration of CFA. MLA (3.0 mg/kg), or saline was given 2 h after the injection of CTX. Paw withdrawal thresholds were measured using Von Frey's Filaments test at 6, 24, and 42 h after administration of CFA. Data represent the mean±SD of 6 rats. cP<0.01 vs saline group; eP<0.05, fP<0.01 vs saline+CFA-treated group.
Discussion
AA has been used as a model of sub-chronic or chronic inflammation in rats and is of considerable relevance to the study of pathophysiological and pharmacological control of inflammatory processes, as well as for the evaluation of the analgesic potential or anti-inflammatory effects of drugs 23, 24. AA elicits joint swelling, synovial membrane inflammation, and cartilage destruction. In addition, it is marked by increased sensitivity of the affected paw to pressure or thermal stimulus. The arthritis observed in rats is associated with a hyperalgesic phenomenon and spontaneous behaviors, such as protecting the affected paw and avoiding putting body weight on the paw. The hyperalgesia is more evident during the acute inflammatory phase 25. The present study demonstrates that CFA containing killed M tuberculosis induced AA in rats with joint swelling, hyperalgesia and synovial membrane inflammation. This effect of CFA is consistent with the results of other studies that have examined the action of CFA-induced AA in rats 26. Treatment of AA rats with CTX inhibited paw swelling, hyperalgesia, joint inflammation and, importantly, damage to the synovium, indicating that CTX might be an effective treatment for rheumatoid arthritis.
The pro-inflammatory cytokines TNF-α, IL-1, and IL-2 have been shown to play an important role in the pathophysiology of arthritis development in animal models and humans. It was reported that increased expression of inflammatory cytokines, including TNF-α and IL-1β, was observed in the bone region of the knee joint or serum samples from human osteoarthritis or rheumatoid arthritic patients 27. TNF-α and IL-1β enhance the proliferation of fibroblasts, stimulate the production of PGE2 28, and increase the expression of other cytokines and synthesis of collagen by synovial cells, contributing to cartilage and bone destruction 29. Thus, various strategies to block their activity are now being clinically applied and have been shown to be effective in the treatment of experimental arthritis 30. In the present study, the anti-inflammatory action of CTX is associated with significantly reduced IL-1 and TNF-α levels in the sera of AA rats.
It has been suggested that the anti-inflammatory cytokine IL-10 is an important factor in resolving chronic inflammation. IL-10 inhibits the production of proinflammatory cytokines including IL-1, TNF-α, and IL-2 31, 32. IL-10 administration suppressed the progression of arthritis in animal models, and clinical improvement has been reported in rheumatoid patients treated with recombinant human IL-10 33, 34. In this report, consistent with previous studies, a decrease in IL-10 levels in the serum of AA rats was found 35. The administration of CTX markedly increased IL-10 levels. Although this increased production of IL-10 cannot be definitively attributed to CTX's anti-arthritis actions, it is clear that CTX shifts the balance of the cytokine parameters in the serum away from pro-inflammatory cytokines (TNF-α, IL-1, and IL-2) and toward the production of anti-inflammatory cytokines such as IL-10.
A number of recent studies have indicated that the cholinergic anti-inflammatory pathway is an important regulator of cytokine-mediated damage in local and systemic experimental diseases such as arthritis and pancreatitis. Intracerebroventricular administration of muscarinic receptor agonists significantly decreased serum TNF-α levels, indicating that muscarinic brain networks regulate the cytokine-controlling function of the vagus nerve 36. Epibatidine, a potent agonist of nAChRs, has structural and functional characteristics similar to that of acetylcholine and nicotine and it attenuated increases in joint circumference and pain-related behaviors induced by injecting a mixture of kaolin and carrageenan into the knee joint. The effects of epibatidine were altered by mecamylamine, a nicotinic receptor antagonist 37. The administration of α7-nAChR agonists inhibits not only TNF-α but also IL-1, IL-6, IL-8, and high mobility group box1 (HMGB1) 38. Furthermore, a number of studies indicate that cholinergic signaling mediated by α7-nAChR has been found in cytokine-producing cells. Cholinergic signals derived from vagus nerve stimulation inhibit the release of TNF, IL-1, HMGB1, and other cytokines by transducing cellular signals that inhibit the nuclear activity of NF-κB 38.
In contrast to the roles of nicotinic cholinergic receptors agonists discussed earlier, the present study indicates that CTX, which may be a nicotinic antagonist, also has a role in inflammatory relief 19, 39. As far as we know, no reports demonstrate that CTX interacts with any receptor other than AChR. In the present study, α7-nAChR antagonism was induced by MLA, which was ineffective in AA rats by itself. However, co-administration of MLA with CTX antagonized the analgesic and anti-inflammatory effects of CTX in AA rats. Previous studies have shown similar results with atropine, a muscarinic cholinergic receptor antagonist. In the hot-plate and acetic acid writhing tests, atropine antagonized the analgesic effects of CTX. We also recently found that atropine antagonized the analgesic action of CTX and canceled the inhibitory effect of CTX on formalin-induced c-Fos expression in the spinal cord of formalin-evoked rat pain models (Liu et al., manuscript submitted). These results indicate that CTX produced potent analgesia or anti-inflammatory effects, which may be mediated by activation of acetylcholine receptors. Therefore, we presume that CTX might exert its activity through α7-nAChR. This possibility, however, needs further investigation.
In summary, the present study demonstrates that the ip administration of CTX, a long chain α-neurotoxin, has distal anti-inflammatory effects in addition to providing anti-nociception in the rat adjuvant arthritis model, possibly by inhibiting the release of cytokines including TNF-α and IL-1 and by preventing joint destruction, which is mediated by activation of the acetylcholine receptor. The positive effect of CTX in rats with AA due to the modulation of inflammatory cytokines and the ability to control pain may be beneficial to human subjects with rheumatoid arthritis.
Author contributions
Zheng-hong QIN, Yan-li LIU designed research; Yan-li LIU, Hai-ming LIN, Rong ZOU, and Jun-chao WU performed research; Rong HAN, Laurence N RAYMOND, Paul F REID contributed new analytical tools and reagents; Yan-li LIU analyzed data; Yan-li LIU, Zheng-hong QIN, Paul F REID wrote the paper.
References
Firestein GS . Evolving concepts of rheumatoid arthritis. Nature 2003; 423: 356–61.
Schwab JH . Bacterial cell-wall induced arthritis: models of chronic recurrent polyarthritis and reactivation of monoarticular arthritis. In: Henderson B, Edwards JCW, Pettipher ER, editors. Mechanisms and models in rheumatoid arthritis. San Diego (CA): Academic Press; 1995. p 431–46.
Chu CQ, Field M, Feldmann M, Maini RN . Localization of tumor necrosis factor alpha in synovial tissues and at the cartilage-pannus junction in patients with rheumatoid arthritis. Arthrit Rheum 1991; 34: 1125–32.
Pelletier JP, Faure MP, Di Battista JA, Wilhelm S, Visco D, Martel-Pelletier J . Coordinate synthesis of stromelysin, interleukin-1, and oncogene proteins in experimental osteoarthritis. An immunohistochemical study. Am J Pathol 1993; 142: 95–105.
Niki Y, Yamada H, Kikuchi T, Toyama Y, Matsumoto H . Membrane-associated IL-1 contributes to chronic synovitis and cartilage destruction in human IL-1 alpha transgenic mice. J Immunol 2004; 172: 577–84.
Bazzoni F, Beutler B . The tumor necrosis factor ligand and receptor families. New Engl J Med 1996; 334: 1717–25.
Bonecchi R, Bianchi G, Bordignon PP, D'Ambrosio D, Lang R, Borsatti A, et al. Differential expression of chemokine receptors and chemotactic responsiveness of type 1 T helper cells (Th1s) and Th2s. J Exp Med 1998; 187: 129–34.
Joosten LAB, Helsen MMA, Saxne T, Van de Loo FAJ, Van de Berg WB . IL-1β blockade prevents cartilage and bone destruction in murine type II collagen-induced arthritis, whereas TNF-α blockade only ameliorates joint inflammation. J Immunol 1999;163: 5049–55.
Newton RC, Decicco CP . Therapeutic potential and strategies for inhibiting tumor necrosis factor-alpha. J Med Chem 1999; 42: 2295–314.
Hirschelmann R, Schade R, Bekemeier H . Acute phase reaction in rats: independent change of acute phase protein plasma concentration and macroscopic inflammation in primary rat adjuvant inflammation. Agents Actions 1990; 30: 412–7.
Nunes FP, Sampaio SC, Santoro ML, Sousa-e-Silva MC . Long-lasting anti-inflammatory properties of Crotalus durissus terrificus snake venom in mice. Toxicon 2007; 49: 1090–8.
Farsky SH, Antunes E, Mello SB . Pro and antiinflammatory properties of toxins from animal venoms. Curr Drug Targets Inflamm Aller 2005; 4: 401–11.
Anti S, Servent D, Menez A . Variability among the sites by which curaremimetic toxins bind to torpedo acetylcholine receptor, as revealed by identification of the functional residues of alpha-cobratoxin. J Biol Chem 1999; 274: 34851–8.
Betzel C, Lange G, Pal GP, Wilson KS, Maelicke A, Saenger W . The refined crystal structure of α-cobratoxin from Naja naja siamensis at 2.4-A resolution. J Biol Chem 1991; 266: 21530–6.
Lukas RJ . Diversity and patterns of regulation of nicotinic receptor subtypes. Ann NY Acad Sci 1955; 757: 153–8.
Servent D, Anti-Delbeke S, Gaillard C, Corringer PJ, Changeux JP, Menenz A . Molecular characterization of the specificity of interactions of various neurotoxins on two distinct nicotinic acetylcholine receptors. Eur J Pharmacol 2000; 393: 197–204.
Dajas-Bailador F, Costa G, Dajas F, Emmett S . Effects of α-bungarotoxin, α-cobratoxin and fasciculin on the nicotine-evoked release of dopamine in the rat striatum in vivo. Neurochem Int 1998; 33: 307–12.
Lena C, Changeux JP . Role of Ca2+ ions in nicotinic facilitation of GABA release in mouse thalamus. J Neurosci 1997; 17: 576–85.
Chen ZX, Zhang HL, Gu ZL, Chen BW, Han R, Rein PF, et al. A long-form α-neurotoxin from cobra venom produces potent opioid independent analgesia. Acta Pharmacol Sin 2006; 27: 402–8.
Chilton M, Mastropaolo J, Rosse RB, Bellack AS, Deutsch SI . Behavioral consequences of methyllycaconitine in mice: a model of α7 nicotinic acetylcholine receptor deficiency. Life Sci 2004; 74: 3133–9.
Chipana C, Camarasa J, Pubill D, Escubedo E . Protection against MDMA-induced dopaminergic neurotoxicity in mice by methyllycaconitine: involvement of nicotinic receptors. Neuropharmacology 2006; 51: 885–95.
Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL . Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 1994; 53: 55–63.
Butler SH, Godefroy F, Besson JM, Weil-Fugazza J . A limited arthritic model for chronic pain studies in the rat. Pain 1992; 8: 73–81.
Besson JM, Guilbaud G . The arthritic rat as a model of clinical pain? In: International Congress Series 837. Excepta Medica. Amsterdam: Elsevier; 1988. p 257–7.
Calvino B, Crepon-Bernard MA, Le Bars D . Parallel clinical and behavioral studies of adjuvant-induced arthritis in the rat: possible relationship with “chronic pain”. Behav Brain Res 1987; 24: 11–29.
Zhang L, Li J, Yu SC, Jin Y, Lv XW, Zou YH, et al. Therapeutic effects and mechanisms of total flavonoids of Turpinia Arguta seen on adjuvant arthritis in rats. J Ethnopharmacol 2008; 116: 167–72.
Kaneko M, Tomita T, Nakase T, Ohsawa Y, Seki H, Takeuchi E, et al. Expression of proteinases and inflammatory cytokines in subchondral bone regions in the destructive joint in rheumatoid arthritis. Rheumatology 2001; 40: 247–55.
Arend WP, Dayer JM . Inhibition of the production and effects of interleukin-1 and tumor necrosis factor-α in rheumatoid arthritis. Arthr Rheum 1995; 38: 151–60.
Dayer JM, Fenner H . The role of cytokines and their inhibitors in arthritis. Baillieres Clin Rheumatol 1992; 6: 485–516.
Moreland LW, Schiff MH, Baumgartner SW, Tindall EA, Fleisch-mann RM, Bulpitt K, et al. Etanercept therapy in rheumatoid arthritis. A randomized, controlled trial. Ann Intern Med 1999; 130: 478–86.
Persson S, Mikulowska A, Narula S, O'Garra A, Holmdahl R . Interleukin-10 suppresses the development of collagen type II-induced arthritis and ameliorates sustained arthritis in rats. Scand J Immunol 1996; 44: 607–14.
Keystone E, Wherry J, Grint P . IL-10 as a therapeutic strategy in the treatment of rheumatoid arthritis. Rheum Dis Clin North Am 1998; 24: 629–39.
Katsikis PD, Chu C, Brennan FM, Maini RN, Feldmann M . Immumoregulatory role of interleukin 10 in rheumatoid arthritis. J Exp Med 1994; 179: 1517–27.
Keystone E, Wherry J, Grint P . IL-10 as a therapeutic strategy in the treatment of rheumatoid arthritis. Rheum Dis Clin North Am 1998; 24: 629–39.
Barsante MM, Roffe E, Yokoro CM, Tafuri WL, Souza DG, Pinho V, et al. Anti-inflammatory and analgesic effects of atorvastatin in a rat model of adjuvant-induced arthritis. Eur J Pharmacol 2005; 516: 282–9.
Pavllov VA, Ochani M, Gallowitsch-Puerta M, Ochani K, Huston JM, Czura CJ, et al. Central muscarinic cholinergic regulation of the systemic inflammatory response during endotoxemia. Proc Natl Acad Sci USA 2006; 103: 5219–23.
Lawand NB, Lu Y, Westlund KN . Nicotinic cholinergic receptor: potential targets for inflammatory pain relief. Pain 1999; 80: 291–9.
Wang H, Liao H, Ochani M, Justiniani M, Lin X, Yang L, et al. Cholinergic agonists inhibit HMGB1 release and improve survival in experimental sepsis. Nat Med 2004; 10: 1216–21.
Hibbs RE, Johnson DA, Shi J, Hansen SB, Taylor P . Structural dynamics of the alpha-neurotoxin-acetylcholine-binding protein complex: hydrodynamic and fluorescence anisotropy decay analyses. Biochemistry 2005; 44: 16602–11.
Acknowledgements
This work was supported by Pre-research Funding of Soochow University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, Yl., Lin, Hm., Zou, R. et al. Suppression of complete Freund's adjuvant-induced adjuvant arthritis by cobratoxin. Acta Pharmacol Sin 30, 219–227 (2009). https://doi.org/10.1038/aps.2008.20
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2008.20
Keywords
This article is cited by
-
Contribution of P2X4 receptor in pain associated with rheumatoid arthritis: a review
Purinergic Signalling (2021)
-
Anti-arthritic Effect of the Spirocyclopiperazinium Salt Compound LXM-15 in Rats and Its Underlying Mechanism
Inflammation (2020)
-
Therapeutic benefits of Indole-3-Carbinol in adjuvant-induced arthritis and its protective effect against methotrexate induced-hepatic toxicity
BMC Complementary and Alternative Medicine (2018)
-
Anti-arthritic property of crude extracts of Piptadeniastrum africanum (Mimosaceae) in complete Freund’s adjuvant-induced arthritis in rats
BMC Complementary and Alternative Medicine (2017)
-
Naja naja atra venom ameliorates pulmonary fibrosis by inhibiting inflammatory response and oxidative stress
BMC Complementary and Alternative Medicine (2014)