Abstract
An overview of the national organisation of prenatal diagnosis (PND) in Spain is presented. Although PND is technically well developed and the number of prenatal services seems to be adequate, the uneven distribution between regions is reflected in a different prevalence reduction of chromosomal disorders and congenital malformations. Only about 41% of pregnant women use PND, with a wide range (14–64%) between regions. There is no national policy in PND or maternal serum screening for Down’s syndrome, but local policies. As clinical genetics is not an officially recognised speciality, there is a shortage of clinical geneticists and it is difficult to organise PND activities and regulate them by law.
Similar content being viewed by others
Introduction
Spain has a total area of 509, 990 km2 and 39 million inhabitants, with uneven distribution and not much racial diversity. The territory is divided in 17 regions (15 peninsular and 2 groups of islands) with their own parliaments and a considerable degree of autonomy.
The birth rate was 9.2 per thousand in 1995 (357),197 births) with a great reduction during the last 15 years. The number of women being pregnant at the age of 35 years or older is about 40,000, with great differences between regions. Prenatal diagnosis (PND) was included among the services offered by the National Health Service (NHS) in 1985 through an Anteproject on Prenatal Diagnosis coming together with the legalisation of therapeutic abortion. Although the social coverage is good, as 98% of the women are registered with the social security system, coverage by the private sector has increased in recent years, mainly in reproductive medicine, with about 6–20% of the women using private services.
PND is technically well developed in Spain with an adequate number of cytogenetics and molecular laboratories available, although rather unevenly distributed, as the majority of the clinical and diagnostic centres are in large cities.
Clinical genetics is not an independent specialty, which makes it difficult to organise PND activities and regulate them by a law.
Sources of Information
National
A National Registry of Congenital Malformations has been operating on a national basis since 1976. This register, called ‘Estudio colaborativo español de malformaciones congénitas’ (ECEMC) is headed by Dr. Martinez Frías in Madrid, and it is designed as a case-control study. Chromosome analysis for children with two defects, born in regions without genetic services was included in 1981. Afterwards a multidisciplinary study was conducted through a complex computer system, and a telephone information service about teratogens, directed to doctors and users, was set up. Epidemiologic analyses of newborns with congenital defects using only dysmorphism as the criterion were performed.
The information about cases and controls is provided by 101 hospitals from all the regions throughout Spain and the results of the study are published in Boletin del ECEMC (Journal of Dysmorphology and Epidemiology) edited by Dr. Martinez Frías.
The registry and studies have been funded by the Ministry of Health, ONCE Foundation, Foundation 1000 for research about congenital defects, and commercial laboratories.
No data on PND are registered systematically in Spain. Partial information about PND is collected by the Spanish Association of Prenatal Diagnosis and published in its journal Progress in Prenatal Diagnosis. As the data have not yet been computerised, no databases are available.
Regional
A register of congenital malformations with the same information as ECEMC has recently been started in Murcia; another register of congenital malformations has been initiated in Euskadi as well as a register of congenital defects in Barcelona.
National Scientistic Associations
-
— Spanish Society of Human Genetics;
-
— Spanish Association of Prenatal Diagnosis;
-
— Ultrasound Section of the Spanish Society of Gynaecology and Obstetrics;
-
— Spanish Society of Perinatal Medicine
Family Associations
Down, Prader-Willi, cystic fibrosis, muscular diseases, retinitis pigmentosa, fragile X (only in Barcelona), cri du chat and spina bifida.
Scientific Meetings
The mentioned scientific associations hold annual or biannual national scientific meetings covering all aspects of PND. In some regions there are also annual regional workshops on PND for family doctors and nurses.
Impact of Prenatal Diagnosis on the Prevalence of Chromosomal Disorders and Severe Malformations
Chromosomal Disorders
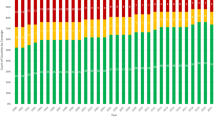
The prevalence has significantly decreased owing to more information available about the risk of congenital malformations and chromosomal disorders, and the more extensive use of PND to which pregnant women over 35 (or 38) years have access.
The global prevalence of Down’s syndrome at birth has been reduced from 1/714 (1986–1990) to 1/789 (1991–1995), with differences in reduction between different regions attributable to the different average mothers’ ages and different uptake of PND and termination of pregnancies. However, this reduction is observed only in the group of mothers over 35 years (from 1/166 to 1/238), whereas in the group of mothers younger than 35 years there is no reduction as a consequence of the increment of births among women between 31 and 34 years in the last period.
Other Congenital Defects
The evolution of the prevalence of 16 congenital defects at birth has been studied and the following was observed:
-
(a)
reduction in the prevalence for neural tube defects (anencephalia, spina bifida and encephalocele) from 1980 5 years before approval of the abortion law, till December 1993 (table 1), mainly due to PND and periconceptional intake of folic acid;
-
(b)
hydrocephalia also showed a significant decrease but only in isolated malformation cases, and an increase in polymalformative syndrome cases. This is due to better PND techniques, particularly ultrasound;
-
(c)
anophthalmia/microphthalmia have decreased as a result of the indirect impact of PND, as these conditions are detected together with other severe anomalies, and
-
(d)
Omphalocele has decreased owing to the impact of PND in polymalformed fetuses with this defect.
Table 1 Prevalence of newborns with neural tube defects in Spain in three periods of time
Psychosocial Impact of Prenatal Diagnosis
As in Spain it is not regulated who should be involved in pretest counselling or counselling after a positive finding, this task is performed by geneticists or obstetricians depending on the centre. After termination of pregnancy, in most cases there is not support.
Available Diagnostic Procedures
Although policies are decided locally, leading to uneven availability of prenatal services, the general recommended indications for prenatal diagnostic procedures are listed in table 2.
Fetal Karyotyping
It is available nationally in 47 centres, of which 28 belong to public institutions, unevenly distributed between different regions (fig. 1). Fetal karyotyping using conventional banding techniques is routinely performed in all PND, including analysis for monogenic diseases. Fluorescence in situ hybridisation (FISH) analysis is available in some laboratories to solve structural rearrangements and to diagnose microdeletion syndromes, and other laboratories can send their cases.
Biochemical Serum Screening
This is a controversial issue in Spain due to the lack of organised regional programmes with adequate guidelines. Three regions are now elaborating programmes. Until 1994, a regional programme for neural tube defects and aneuploidies was operating in Asturias. The screening is done in some public hospitals only for their patients, and in some private laboratories at the request of private clinics.
Ultrasound Screening/Diagnosis
Routine ultrasound screening is not standard practice in all regions, and the recommended three per pregnancy cannot be done everywhere in the national health system because facilities of equipment and specialists are not sufficient. As a high proportion of pregnancies are followed in private clinics, data about the proportion of pregnancies screened are not available.
Detailed — high-resolution, real-time — ultrasound investigations are available in large hospitals and are targeted at pregnancies with increased risk.
Metabolic Disorders Diagnosis
It is centralised in three reference laboratories, two in Madrid and one in Barcelona.
Molecular Diagnosis
It is performed in 24 public and 3 private centres (figure 1), and the conditions currently diagnosed in utero are listed in table 3.
Current Methods in Use for Prenatal Diagnosis
We have only got exact figures from 27 cytogenetics laboratories about the number of prenatal procedures in 1994, and they are listed in table 4.
Amniocentesis
Amniocentesis is in use in most hospitals, even those which have no cytogenetic laboratories, and more than 90% of diagnoses are made by this technique.
Choriocentesis
Choriocentesis is performed in about 17 centres, but the proportion of users is very low, especially in private centres.
Cordocentesis
Cordocentesis is performed only in 10 large hospitals and is restricted to specific cases.
Professional Guidelines
-
— Handbook for Prenatal Diagnosis (Ministry of Health, Madrid, 1989).
-
— Recomendaciones y Protocolos en Diagnóstico Prenatal. Report of the European Study Group on Prenatal Diagnosis (EAPM). Progresos en Diagnóstico Prenatal, vol. 5 (1993).
-
— Protocolos de Procedimientos Diagnósticos y Terapeuticos. Obstetricia. Medicina Materno Infantil (SEGO, Madrid, Spain).
-
— Guidelines for Cytogenetics Laboratories. Progresos en Diagnóstico Prenatal, vol. 8 (1996).
Areas under Development
Interphase Cytogenetics
This area is in rapid growth. The main cytogenetics laboratories both public and private use FISH to confirm or complete diagnosis. For routine diagnosis FISH is only used in a few private centres.
Small laboratories which do not perform FISH and need it to confirm a cytogenetic diagnosis can send samples or slides to others.
Fetal Cells in the Maternal Circulation
This procedure is under investigation, and some genetics centres have elaborated research projects to be funded by Research Funds from the Ministry of Health.
First-Trimester Biochemical Screening
We have no confirmation that biochemical screening in the first trimester is being performed in any region.
Amniofiltration, cervix samples, and early amniocentesis are being developed in one or two hospitals in Madrid and Barcelona.
Funding Arrangements for Prenatal Diagnosis
In a workshop organised by the Ministry of Health in 1986, special funds were allocated for improving PND units and creating new ones. Since 1991, PND is part of the health services in hospitals and depends on their general budget, with a few exceptions where it is still considered a programme and subsidised by special regional funds.
In the last decade, the main prenatal units have benefited from technological development through research grants from different public and private institutions.
Current Legislation Surrounding Prenatal Diagnosis
Termination of Pregnancy
Following article 417bis of ‘Ley orgánica 9/1985’ of July 5, 1985, a pregnancy may be terminated by or under the supervision of a doctor in medicine in an authorised private or public centre or institution (Royal decree of November 21, 1986, No 2409/1986) with the consent of the pregnant woman when one of the following circumstances occurs:
-
(1)
To avoid a serious threat to the life or physical or mental health of the pregnant woman as stated in a report submitted before the intervention by a medical specialist who cannot be the physician performing or under whose supervision the abortion is performed. In emergency cases, when the risk to the pregnant woman is great, her consent is not required.
-
(2)
When the pregnancy is the result of a previously declared rape. The termination must be carried out during the first 12 weeks of gestation.
-
(3)
When the fetus has been previously diagnosed by two specialists, neither of whom is performing the abortion, as having a possible, severe mental or physical handicap. In these cases, the termination must be performed during the first 22 weeks of gestation.
If an abortion is performed where none of these conditions exists, the aborted woman will not be prosecuted.
Article 417bis is maintained in use by the new Penal Code of 8th November 1995 which came into effect on May 24, 1996, with the addition of the following articles:
Article 144: Any one performing an abortion without the consent of the woman or by means of violence, threats or deception may be prosecuted.
Article 145: When an abortion is practised with the consent of the woman but where none of the legally permitted conditions exist, the abortionist may be prosecuted.
Article 146: Criminal charges may be brought if the termination is the result of medical malpractice.
Pre-implantation Diagnosis
‘Ley 35/1988’, November 22, 1988: Assisted Reproduction Techniques. This law regulates the human reproduction techniques: AI, FIV, TE, TIG when they are performed by a specialist in authorised public or private medical centres.
The purpose of human reproduction techniques is to facilitate the procreation in sterile couples.
These techniques may be used for the treatment and prevention of genetic disorders. Investigation and experimentation are possible under determined conditions (Articles 14, 15, 16, 17).
The new Penal Code enlarges new articles concerning genetic manipulation and reproduction which are summarised as follows:
Article 159: (1) The manipulation of human genes in such a way that the genotype is altered may only occur when the intention is the elimination or the improvement of a serious illness.
Criminal charges may be brought if alteration of the genotype was caused by negligence.
Article 161: (1) The fecundation of human ovules may only be for human procreation and not for other purposes. (2) The creation of identical human beings, cloning or any other procedure concerning the selection of the race is not permitted.
Article 162: Assisted reproduction in a woman may not occur without her consent.
Present Problems and the Future
Our current problems which could have repercussions in the near future are mainly based on insufficient and/or inadequate information and deficient organisation of PND.
Although the public has more information through the media and demand for PND is growing, at the present time the majority of the communities (except Catalonia and Basque Provinces) have no policy concerning PND.
The average coverage for advanced maternal age is approximately 41% (range 14–64%) considering only those regions in which the procedures are available. Of the almost 60% of pregnant women who do not have invasive
PND, we do not know in what proportion it is the result of a deliberate decision and in what proportion it is due to insufficient information.
There is no national policy concerning maternal serum screening for Down’s syndrome, and the lack of information about the meaning of the screening results in unnecessary anxiety caused by misinformation and bad advice.
Teaching in human genetics is not officially included in the programme of medical students in most of the Spanish universities. As a consequence, the level of knowledge in human genetics of Spanish physicians is poor and so the risk identification at the first health level and the decision to carry out a specific prenatal test are not always adequate.
As clinical genetics is not an officially recognised speciality, there is a shortage of clinical geneticists which has led to the employment of non-specialists in this field. As concerns termination of pregnancy, there are many problems because public centres which perform it are very few and concentrated in large cities. This means that about 85% of terminations for an affected fetus involve the need for travelling long distances from home, and getting a sample for confirming results is very difficult.
Another important problem is the general reduction of public budget for research work in the last 2 years.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gabarrón, J., Ramos, C. Prenatal Diagnosis in Spain. Eur J Hum Genet 5 (Suppl 1), 64–69 (1997). https://doi.org/10.1007/BF03405965
Issue Date:
DOI: https://doi.org/10.1007/BF03405965