Abstract
Prenatal diagnosis (PND) is very developed in France, especially in the area of ultrasound (US) screening. The activity is regulated by law, and laboratories have to be authorised to perform any type of prenatal biological test if the purpose is to diagnose fetal defects. There are 70 cytogenetics laboratories and 50 biochemistry laboratories performing serum marker screening, about half of them being private. PND of chromosomal anomalies is offered to women over 37 years of age, to women who already had a child with a chromosomal anomaly, in case of abnormal US findings, if one of the parents has a balanced chromosomal anomaly and if the risk of chromosomal anomaly is higher than 1:250 according to the serum markers. Half of the trisomy 21 cases are now detected prenatally and pregnancies terminated. Fetal cell sampling is performed by amniocentesis in 70% of cases, by chorionic villus sampling in 7% of cases and by fetal blood sampling in 23% of cases. There are no professional guidelines and no quality assessment networks for any of the techniques in use. PND is regulated by two major laws: the Law on Abortion (1975) and the Law on Bioethics (1994).
Similar content being viewed by others
France is a country of 58 million inhabitants and 760,000 births per year. The life expectancy of women is 81 years and of men 73 years. The birth rate is 13.4 per thousand and the fertility rate 1.8 per woman. Sixty-seven percent of the mothers are of French origin and only 3% of all the pregnant women do not speak French. The social coverage is good: 97% of the women are registered with the social security system.
General practitioners (GPs) represent 54% of all physicians. GPs follow up 40% of the pregnancies during the two first trimesters. The first prenatal visit takes place during the first trimester in 95% of the pregnancies. Pregnancies are followed up exclusively in private practices in 42% of cases, exclusively in public hospitals in 37% of cases, the others being followed up by both systems. Half of the maternity hospitals are public and half are private.
Prenatal diagnosis (PND) is very developed in France, especially in the area of ultrasound (US) screening. The activity is regulated by law, and laboratories have to be authorised to perform any type of prenatal biological test if the purpose is to diagnose fetal defects.
Medical genetics is an independent medical specialty since 1995. There are 70 cytogenetics laboratories and 50 biochemistry laboratories performing serum marker screening (a maximum of 70 has been defined by law for the future). Half of these laboratories are private. In addition, there are 62 clinics offering genetic counselling.
Sources of Information
At the National Level
National data on cytogenetics laboratory activity in the field of PND are available for the period 1980–1991 [1]. During that period, the notification of all karyotypes performed was mandatory for the laboratories in order to be paid directly. The same applied for biochemical tests and for molecular tests. As of January 1992, fetal karyotypes were considered as ordinary medical tests and reimbursed for four indications: maternal age 38 and over, previous child with a chromosomal anomaly, parent with a constitutional chromosomal anomaly, and abnormal US findings. From then on, they were no longer notified to the Ministry of Health.
In 1994, the new Law on Bioethics was voted, which clearly defined the organisation of prenatal diagnostic activities. Notifications of all laboratory tests in the prenatal period were mandatory once a year for every authorised laboratory. The national data will be available again starting from 1994. Therefore, there is a gap of 2 years, for which the number of fetal karyotypes performed was estimated by a mailed survey.
There is no national birth defects registry.
At the Regional Level
Four regions are systematically surveyed by a birth defects registry, which also includes the terminations of pregnancy. The four regions are: Paris, Bas-Rhin (Strasbourg), Bouches-du-Rhône (Marseille) and Centre-Est-Auvergne (Lyon and Clermont-Ferrand). Data are available from 1980. The registries establish an annual report and their data are also published in the Eurocat and in the Clearinghouse for Birth Defects Monitoring System annual reports.
At the Local Level
There is a French network of departments of fetal medicine (Club de Médecine Fœtale). The participants in this network share their data by using the same software to computerise them. They discuss their data once a year and publish specific studies. The data are accessible upon request.
Impact of PND
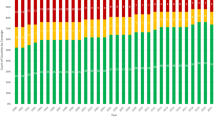
PND of chromosomal anomalies started in 1972 in one laboratory. In 1976, five laboratories were performing them. In 1980, the percentage of women aged 38 and over who had fetal karyotypes was 13%. This percentage increased slowly to reach 64% in 1992 (table 1). Since then this rate has stabilised. Until 1985, the four reasons accepted to obtain a fetal karyotype were: maternal age ≥ 38, previous child with a chromosomal anomaly, parenal chromosomal anomaly and fetal sexing for X-linked conditions. In 1985, it was decided to also financially support karyotypes performed because of abnormal US findings. In 1990, the discussion on whether to introduce maternal serum marker screening started, with a pilot study on 22,000 pregnancies [2]. At the end of the pilot phase, no decision was taken, but the 14 initial laboratories kept on offering those tests and a few more started. In 1994, 11% of all the pregnancies were tested, and in 1995 20%, despite the fact that the fetal karyotypes generated by this screening policy were not reimbursed, a situation which changed on January 1, 1997. A leaflet on serum screening was issued by the Ministry of Health in 1996 and sent to all GPs, gynaecologists, obstetricians and midwives (110),000 professionals). This leaflet includes recommendations on good practices.
The number of fetal karyotypes performed in France was 36,000 in 1990, 41,200 in 1991 and 50,000 in 1994, representing 6% of all the pregnancies. The reasons why these karyotypes were performed are mentioned in table 2. The impact of PND of chromosomal anomalies is increasing every year. The data for the years 1989–1992 are shown in table 3. Half of the trisomy 21 cases are now detected prenatally and the pregnancies terminated [3–9]. In women younger than 35, this proportion is 25% whereas it is 82.7% in women over 40 (table 4). Nonetheless, the prevalence rate at birth has barely decreased (table 5) due to the fact that women now have their children at older ages. In fact, many diagnoses are done late in pregnancy through US screening (table 6), especially in young women.
The efficacy of prenatal screening by US for some major anomalies is also known thanks to the registries of birth defects [10, 11]. The proportion of terminated pregnancies is shown in table 7. A very significant proportion of these major malformations are now reasons for terminating pregnancies.
For the Mendelian disorders, the impact of PND cannot be evaluated. Only the total number of prenatal tests for Mendelian conditions during the period 1980–1990 is available from the Ministry of Health: metabolic diseases: 1,300 tests; haemoglobinopathies: 689 tests; haemophilia: 177 tests; X-linked conditions: 419 tests, and cystic fibrosis: 334 tests [12].
Diagnostic Procedures Available
In France there are 70 cytogenetics laboratories offering PND.
Maternal serum screening for Down syndrome was introduced in 1990. A study of the practices was performed in 1995. The survey showed that 11 % of all pregnant women had a serum screening in 1994, 20% in 1995, with significant differences between regions. The test was prescribed by 12.3% of the GPs and 68.4% of the obstetricians. Gestational age was determined by sonography for 93% of the pregnancies followed by obstetricians and 61 % of the pregnancies followed by GPs. Among the 32 laboratories which were active in 1994, 9 used a simple test (hCG), 12 a double test, and 11 a triple test (hCG+AFP+uE3). Half of the laboratories were involved in a quality control network. The cut-off risk level for amniocentesis (AC) was 1/250 in 13 laboratories and 1/100 in the others (this was the cut-off level chosen during the pilot study in 1990–1991). The risk was calculated using a software by only 19 laboratories. This survey demonstrates a widespread diffusion of the test despite the fact that it was not yet reimbursed, but also that the practice is far from optimal. It also shows that guidelines had to be issued and diffused among the professionals involved in this type of screening. These guidelines were sent in December 1996. They state that serum screening should be offered to all women prior to the 15th week and performed between 15 and 18 weeks, independent of their ages; that gestational age should be carefully estimated; that a US examination should be done to detect twin pregnancies and/or major malformations; that the woman has to formally agree on the test, which can be performed only by an authorised laboratory; that an AC should be offered to all women having a risk equal to or greater than 1:250 and that the woman’s decision about having or not having the test and the AC must be respected.
The conditions which are currently diagnosed using molecular biology techniques are listed in table 8. The list of laboratories performing prenatal tests is available at the internet address: https://doi.org/www.infobiogen.fr/orphanet/
Current Methods in Use for PND
Fetal cell sampling is performed by AC in 70% of cases, by chorionic villus sampling in 7% of cases and by fetal blood sampling in 23% of cases (table 9).
Fluorescence in situ hybridisation (FISH) is now currently used by 75% of cytogenetics laboratories for PND purposes.
US screening is widely used. 96% of the pregnant women had 3 US exams and more in 1994.
There are no professional guidelines and no quality assessment networks for any of the techniques in use, except for serum marker screening.
Areas under Development
FISH on interphase nuclei is being developed and evaluated in 15 French laboratories. Five laboratories are involved in a research programme on fetal cells in maternal blood. Serum marker screening at the first trimester is being evaluated in 13 laboratories. Other areas of research are: polymerase chain reaction and primed in situ labelling on interphase nuclei. Several obstetric departments are evaluating sonography during the first trimester in comparison or in conjunction with serum marker screening. Several biochemistry laboratories are testing new serum markers.
Funding Arrangements for PND
All the tests are reimbursed by the social security system for all the indications defined by the National Committee of Nomenclature of medical acts. Three US examinations are reimbursed per pregnancy if the pregnancy is normal (one per trimester). For abnormal pregnancies, the number is not limited.
Current Legislation Surrounding PND
PND is regulated by two major laws: the Law on Abortion and the Law on Bioethics.
The abortion law was voted in 1975. It authorises every woman to freely choose to abort until 10 weeks of pregnancy. After this time limit, the termination of pregnancy is allowed only for the woman’s safety or if the fetus is affected by a severe condition, for which no treatment is available. No time limit is fixed for this. The authorisation to terminate the pregnancy is delivered by two court experts, one of them being an expert in fetal medicine.
The bioethics law was voted on July 29, 1994. This law states that any investigation performed in order to make a prenatal diagnosis of a birth defect may only be performed by a laboratory which has obtained formal agreement for this activity. Authorised laboratories have to produce an annual report on their activities and can loose their agreement if their activities are not judged satisfactory. The committee which evaluates the activities of all the laboratories advises the Minister of Health. To be authorised, a laboratory has to belong to a multidisciplinary network including medical geneticists, sonographists, obstetricians, paediatricians, surgeons, cytogeneticists, molecular biologists and pathologists, in order to guarantee the multidisciplinary approach of all the decisions.
According to the bioethics law, pre-implantation diagnosis can be performed only if a physician working in a multidisciplinary network has verified that the couple, given the family history, has a high probability of giving birth to a child with a genetic condition of sufficient severity to be incurable at the time of diagnosis. The laboratories offering pre-implantation testing have to be authorised by the Ministry of Health. The criteria for being authorised are still in the process of definition and should be published by 1997. At the present time, no pre-implantation diagnosis is performed in France, but some patients have obtained such a diagnosis in other European countries and their test was financially supported by the French social security system.
Problems Faced by the Professionals
The problems mentioned by the professionals are the new financial constraints due to the economic crisis and the lack of positions available for new collaborators. They also miss professional guidelines.
References
Briard ML: Le diagnostic prénatal en France: Un modèle original. Expérience de l’Association Française pour le Dépistage et la Prévention des Handicaps de l’Enfant; in Moatti JP, Mawas C (eds): Evaluation des Innovations Technologiques et Décisions en Santé Publique. Paris, Editions INSERM, 1992, pp 171–185.
Aymé S, Briard M-L, Farriaux J-P: Antenatal maternal serum screening for Down syndrome: Results of the French prospective pilot study on 22,410 pregnancies. Excerpta Medica Int Congr Ser 1994;1041:349–352.
Aymé S, Julian C, Macquart-Moulin G, Moatti J-P, Mattei J-F: Prenatal diagnosis of birth defects: Accessibility, acceptability and effectiveness in the Bouches-du-Rhône area, France; in Duru G, Engelbrecht R, Flagle CD, Van Eimeren W (eds): System Science in Health Care 3. The Major Health Care Problems, vol 140, in Médecine Légale et Toxicologie Médicale. Lyon, Masson, 1988, pp 307–309.
Moatti J-P, Julian C, Le Galès C, Macquart-Moulin G, Mattei J-F, Aymé S: Economic assessment of prenatal diagnosis by amniocentesis: A ‘revealed preference’ approach for measurement of benefit of prevention; in Duru G, Engelbrecht R, Flagle CD, Van Eimeren W (eds): System Science in Health Care 3. The Major Health Care Problems, vol 140, in Médecine Légale et Toxicologie Médicale. Lyon, Masson, 1988, pp 325–328.
Julian C, Huard P, Gouvernet J, Mattei J-F, Aymé S: Physicians acceptability of termination of pregnancy after prenatal diagnosis in Southern France. Prenat Diagn 1989;9:77–89.
Moatti J-P, LeGales C, Julian C, Durbec J-P, Mattei J-F, Aymé S: Socio-cultural inequities in access to prenatal diagnosis: The role of insurance coverage and regulatory policies. Prenat Diagn 1990;10:313–325.
Julian C, Macquart-Moulin G, Moatti J-P, Loundou A, Aurran Y, Chabal F, Aymé S: Attitudes of women of childbearing age towards prenatal diagnosis in southeastern France. Prenat Diagn 1993;13:613–627.
Julian C, Macquart-Moulin G, Moatti J-P, Aurran Y, Chabal F, Aymé S: Reasons for women’s non uptake of amniocentesis. Prenat Diagn 1994;14:859–864.
Julian-Reynier C, Aurran Y, Dumaret A, Maron A, Chabal F, Giraud F, Aymé S: Attitudes toward Down syndrome: A population-based study of 280 cases. J Med Genet 1995,32:597–599.
Julian C, Philip N, Scheiner C, Aurran Y, Chabal F, Maron A, Gombert A, Aymé S: Impact of prenatal diagnosis by ultrasound on the prevalence of congenital anomalies at birth. J Epidemiol Community Health 1994;48:290–296.
Julian-Reynier C, Macquart-Moulin G, Philip N, Scheiner C, Potier A, Gambarelli D, Aymé S: Fetal abnormalities detected by sonography in low risk pregnancies: Discrepancies between pre- and post-termination findings. Fetal Diagn Ther 1994;9:310–320.
Briard ML, Farriaux JP: Diagnostic anténatal biologique: Les enjeux et les statistiques françaises. Immunoanal Biol Spec 1992;33:15–22.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aymé, S., Morichon, N., Goujard, J. et al. Prenatal Diagnosis in France. Eur J Hum Genet 5 (Suppl 1), 26–31 (1997). https://doi.org/10.1007/BF03405957
Issue Date:
DOI: https://doi.org/10.1007/BF03405957