Abstract
We have investigated 8 patients from 7 unrelated families with lamellar ichthyosis (LI) for defects in the keratinocyte transglutaminase (TGK) gene. We have characterized three novel homozygous mutations and a previously reported splice acceptor site mutation. One patient showed a C-to-T change in the binding site for the transcription factor Sp1 within the promoter region. Another patient had a Gly143-to-Glu mutation in exon 3 and a third patient, affected with a particular form of LI sparing the four limbs, demonstrated a Val382-to-Met mutation within exon 7. These three patients exhibited drastically reduced transglutaminase activity and an absence of detectable TGK polypeptide, as assessed by immunofluorescence and immunoblotting. Northern blot analysis showed that the Sp1 site mutation was associated with profound reduction of TGK transcript levels whereas normal transcript levels were observed for the two missense mutations. We hypothesize that the Sp1 site mutation impairs transcription of the TGK gene, whereas the two missense mutations induce structural changes leading to protein instability. Linkage to TGK was excluded in another family and no evidence for TGK defect was found in 3 other patients. These results further support the involvement of TGK in some patients with LI. They identify a TGK mutation as a cause for non-generalized LI and further delineate the molecular mechanisms underlying TGK deficiency in LI.
Similar content being viewed by others
Introduction
Lamellar ichthyosis (LI) (Mendelian Inheritance in Man No. 242100) is a severe inherited disorder of keratinization characterized by generalized hyperkeratosis and variable redness of the skin [1, 2]. LI is transmitted in an autosomal recessive pattern with an estimated prevalence of 1/200,000. Newborns often present encased in a thick stratum corneum (collodion membrane) which may lead to life-threatening complications. Later patients develop large, thick scales covering the entire body with variable severe ectropion, scaring alopecia, palmoplantar keratoderma and decreased sweating.
The pathogenesis of LI involves accelerated turnover and abnormal terminal differentiation of the epidermis resulting in marked thickening of the stratum corneum. The final stages of epidermal differentiation implicate the formation of the cornified cell envelope, a specialized structure in the cell periphery of terminally differentiated keratinocytes which assumes protective functions [3]. Cell envelope formation develops at the cytoplasmic side of the plasma membrane of the stratum granulosum cells and is completed in corneocytes of the stratum corneum. This process involves the sequential deposition of structural precursor proteins such as involucrin, small prolinerich proteins and loricrin which are covalently cross-linked by transglutaminase 1 (TGM1, also termed keratinocyte transglutaminase, or TGK) and transglutaminase 3 (TGM3) [3–7].
Immunohistologic studies by Hohl et al. [8] and Lavrijsen et al. [9] have reported absent or diminished membrane-bound and cytoplasmic expression of keratinocyte transglutaminase (TGK) in skin of LI patients, as detected by the anti-TGK antibody B.C1. These results raised the possibility that the pathophysiology of LI may involve deficient expression of TGK resulting in impaired cross-linkage and deposition of precursor structural proteins of the cell envelope. The demonstration by Russel et al. [10] of genetic linkage between LI and the transglutaminase 1 locus (TGM1) on chromosome 14q11 further supported the implication of TGK in the disease. The TGK gene encodes the 92-kD keratinocyte transglutaminase, a membrane-bound protein belonging to the superfamily of transglutaminase (TG) proteins which catalyse ε-(γ-glutamyl) lysine isopeptide bonds [11, 12]. A structural model has been proposed for TGK on the basis of the X-ray crystal structure of human blood coagulation factor XIIIa, another member of the TG family. This model, common to all TGs, comprises an amino terminal activation peptide, a β-sandwich domain, a core domain containing the catalytic site and barrel 1 and barrel 2 domains [13]. The description of the first TGK mutations associated with TGK deficiency in LI demonstrated the direct involvement of the gene in the disease [14, 15]. A number of mutations of the TGK gene have now been identified in LI patients [16–20]. These mutations predict premature termination codons (PTCs) or amino acid substitutions which are thought to impair cross-linking of precursor proteins by TGK to form a functional cornified cell envelope. However, normal TGK expression and activity have been reported in LI patients with no detectable TGK mutation [21]. Moreover, a number of LI families have been shown to be unlinked to the TGM1 locus [16, 18], providing evidence for locus heterogeneity of the disease. Genetic heterogeneity of the disease was further supported by the evidence in three families of Moroccan origin for another disease locus on chromosome 2q33–35 [22].
In this article, we report on the analysis of the TGK gene in 8 patients with LI. After testing for linkage to the TGM1 locus, the 15 exons and flanking intronic regions were screened for mutations by heteroduplex analysis. We identified three novel homozygous mutations and a previously reported splice site mutation. The consequences of the new defects on TGK transcript levels and TGK expression and activity were investigated. Linkage to the TGM1 locus was excluded in a further family, and no evidence for the involvement of TGK was found in 3 other patients studied.
Materials and Methods
Patients
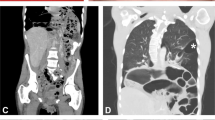
Eight patients from 7 unrelated families presenting with LI were studied, family C having 2 affected children (fig. 1). All families but 1 (family D) were from consanguineous marriages. Patients were of French, Iranian, Moroccan, Portuguese or Tunisian origin. The diagnosis was established through examination by the same dermatologist and review of medical records. All patients had a history of collodion babies at birth, and a life-threatening neonatal presentation was noted in the case of patient 1. Patients showed no extracutaneous manifestations associated with ichthyosis. Five patients (A4, C5, C6, 1 and 2) developed severe generalised LI with large and thick scales and required systemic retinoid treatment. Patients A4 and 1 were particularly severely affected with persistent ectropion and considerably thickened epidermis only partially improved by retinoid treatment. Two patients (D5 and 3) presented with moderate LI with finer scaling and variable erythema. Patient B5 presented with a particular form of LI made of large dark-brown scales affecting the trunk, the neck and the scalp but sparing remarkably the face and the four limbs (fig. 2). Peripheral blood samples were collected for DNA extraction from all members of the nuclear families A-D and from patients 1, 2 and 3. The parents of patient 3 were not available for the study.
Pedigrees of LI families with the results of haplotype analysis of the TGK gene using the (CA) repeat in intron 14. Double bar denotes a consanguineous marriage. Patient 3 had a cousin, aged 24 years, from a consanguineous marriage, affected with LI. Individuals marked by an asterisk were not available for the study.
Genotype Analysis
Linkage of the disease to the TGM1 locus on chromosome 14q11 was tested by using the polymorphic (CA) repeat located within intron 14 of the gene [11]. Genomic DNA was extracted from peripheral blood cells [23] and the CA repeat was amplified using primers described in table 1b. PCR products were separated on denaturing Polyacrylamide gel (Sequagel, National Diagnostics) and transferred to positive-charged Nylon membrane (Pall). Primers were end-labelled with α32P-dCTP using terminal transferase (Boehringer Mannheim) and hybridized to membranes for 2 h at 42°C in Church buffer [24]. Membranes were washed in 2 × SSC, 0.1 % SDS at room temperature, and exposed to X-ray film.
Mutation Screening
The 15 exons and flanking intronic regions of the TGK gene were amplified from genomic DNA by PCR using specific primer pairs (table 1a). Heteroduplex analysis was performed by means of conformation-sensitive gel electrophoresis (CSGE) using Ganguly’s protocol [25]. The gel contained 10% polyacrylamide:bis(acryoyl)piperazine (99:1), 15 % formamide, 10% ethylene glycol made with a glycerol tolerant buffer TTE (Tris 89 mM, Taurine 7 mM, EDTA 0.1 mM). Samples were prepared by mixing PCR products from the patients and a normal control in a 2:1 ratio. After denaturation at 98°C for 5 min and annealing at 68°C for 1 h to favour the formation of heteroduplexes, the samples were subjected to electrophoresis at 500 V for 16 h. The gel was staining with ethidium bromide (2 µg/ml), and DNA was visualised on UV light.
Sequence A nalysis
DNA fragments showing altered electrophoretic mobility were directly sequenced. PCR products were purified from low-melting gel and cycle sequencing amplification was performed in the forward and reverse orientations using ABI PRISM Dye Terminator mix and AmpliTaq DNA Polymerase FS (Perkin Elmer). After precipitation, products were loaded on an ABI 373 automated sequencer and the sequences were analysed with Factura and Navigator softwares (Applied Biosystems).
Restriction-Endonuclease A nalysis
Amplified genomic DNA was cleaved with the appropriate restriction enzymes (AciI, BpmI, MaeIII, MspI and SacII) according to the manufacturer’s recommendations (New England Biolabs and Boehringer Mannheim) and analysed by 2% agarose gel electrophoresis.
Keratinocyte Culture
Keratinocytes were cultured from skin biopsies obtained from patients 1, A4, B5, C5 and C6 as described by Rheinwald and Green [26]. The cells were grown in the presence of 200 µg/ml CaCl2 and were collected 5 days after confluency.
Immunofluorescence Staining
Indirect immunofluorescence staining was performed on cryosections of punch skin biopsies with the use of the mouse monoclonal antibody B.C1 to TGK [5, 27] diluted 1:1 and a fluorescein isothiocyanate (FITC)-labelled anti-mouse antibody (Dako, Glostrup, Denmark).
Transglutaminase Activity
Transglutaminase (TG) activity was measured in membrane and cytosolic fraction from cultured keratinocytes. Cells were lysed by sonication in 20 mM sodium phosphate pH 7.2, 0.5 mM EDTA, 10 mM DTT, 50 µg/ml phenylmethylsulphonylfluoride. After centrifugation at 25,000 g at 4° C for 30 min, the supernatant was taken as the cytosolic fraction. The pellet was re-extracted by sonication with the same buffer plus 1% Triton X-100. After incubation for 10 min at 37° C, the lysate was centrifuged again and the supernatant (membrane fraction) taken for measuring the TG activity as described in [28]. TG activity was expressed as picomoles 3H-putrescine incorporated into dimethylcaseine per hour and milligram protein.
Immunoblot Analysis
Western blot analysis was carried out from cultured keratinocytes as described [5, 27]. Cells were lysed by sonication in 10 mM Tris-HC1 pH 7.4, 5 mM EDTA, 50 µg/ml phenylmethylsulphonylfluoride, 1 µg/ml E-64, 1 µg/ml pepstatin, 1 µg/ml leupeptin. The supernatant obtained after centrifugation at 25,000 g for 30 min was taken as the cytosolic fraction. The membrane fraction was obtained after sonication of the cell pellet in the same buffer plus 1 % Triton X-100 and centrifugation. Forty micrograms of protein was electrophoresed through a 10% SDS Polyacrylamide separation gel and 4%/4 M urea concentration gel. After partial renaturation, the gel was electroblotted to nitrocellulose. Detection of TGK protein was carried out with antibody B.C1 and the ECL detection kit (Amersham) according to the manufacturer’s instructions. Protein content was determined with the Bradford assay (BioRad) using bovine serum albumin as standard.
Northern Blot Analysis
Total RNA was extracted from differentiating keratinocytes in culture using the guanidium thiocyanate method described by Chomczynski and Sacchi [29]. Thirty micrograms of total RNA were separated through a 1 % agarose gel containing 6% formaldehyde and transferred to a positively charged Nylon membrane (Pall). The membrane was pre-hybridized at 42°C for 6 h in a solution containing 50% formamide, 4 × SSC, 8% dextran sulfate, 1 × Denhardt’s solution and 200 µg/ml degraded herring sperm DNA. A cDNA probe for TGK spanning exons 3–7 (table 1c) was radiolabeled with α32P-dCTP and hybridized to the membrane at 42° C for 16 h. Filters were washed in a solution containing 0.5 × SSC and 0.5% SDS for 30 min at room temperature and for 30 min at 65°C followed by autoradiography at −70°C. The membrane was rehybridized with a cDNA probe for the ubiquitously expressed glyceraldehyde 3-phos-phate dehydrogenase (GAPDH) gene to compare the amount of RNA loaded per lane.
Results
Linkage Study
Genotype analysis was performed in families A-D and in the inbred patients 1, 2, 3 using the (CA) repeat within intron 14 of TGK gene (fig. 1). Haplotype analysis in the consanguineous families A, B and C showed that patients A4, B5, C5 and C6 were homozygous at the TGM1 locus with no recombination between the disease locus and this marker in the unaffected offspring. This result was consistent with linkage of the disease to the TGM1 locus in these families partially or fully informative for this marker. In contrast, linkage to the TGM1 locus could be excluded in family D in which the affected offspring D5 shared the same genotype as her unaffected brother D4 (fig. 1). Homozygosity mapping analysis in patients 1, 2 and 3 showed that these patients were homozygous for the (CA) repeat in TGK (fig. 1). This result was compatible with linkage, although one or both parents of these patients being untyped, the possibility of both parents being uninformative for this marker could not be excluded.
Identification of TGK Mutations in Patients A4, B5, 1 and 2
To screen for mutations within the TGK gene, the 15 exons and flanking intronic sequences of the gene were amplified by PCR and run on CSGE. Fragments showing an abnormal migration pattern were sequenced.
Family A. Analysis of exon 1 in patient A4 showed a heteroduplex band in comparison to the control (fig. 3). Direct sequencing of this amplified genomic fragment revealed a C-to-T homozygous substitution at nucleotide position −86 in exon 1 (fig. 4). This change is localised at the second base of a CCGCCC motif which is the reverse complement sequence of the recognition site for the Sp1 transcription factor. Sequencing of the family members showed that both parents (A1 and A2) are heterozygous carriers for this mutation and that the unaffected offspring A3 had not inherited this mutation. These results are consistent with an autosomal recessive inheritance of the disease in this family. This mutation designated ‘−86 C→T’ abolishes a restriction enzyme site for AciI (CCGC) and yields digestion fragments of 218 and 309 bp from the mutant allele, and 218, 283 and 26 bp from a normal allele.
Sequence analysis of TGK mutations in patients A4, B5 and 1. The sequence obtained in the control (top) and the patients (bottom) are shown. Patient A4 displayed a homozygous C-to-T transition at position −86 bp of the promoter region of the TGK gene, numbering as in Yamanashi et al. [12]. Patient B5 was homozygous for a G-to-A transition changing valine codon 382 into a methionine codon. Patient 1 was homozygous for a G-to-A transition changing glycine codon 143 for a glutamic acid. Numbering of the amino acids refers to the genomic sequence in Genbank/EMBL No. M86360. The mutations are indicated by an arrow head. Patient 2 displayed a homozygous A-to-G mutation in the splice acceptor site of intron 5 previously reported in Huber et al. [14] (data not shown).
Family B. Patient B5 showed a heteroduplex on analysis of exon 7 (fig. 3). Sequence analysis of genomic DNA revealed a homozygous G-to-A substitution which predicts the conversion of valine codon 382 (GTG) to a codon for methionine (ATG) (fig. 4). This mutation, V382M, abolishes a restriction enzyme site for MaeIII (GTNAC) leaving the mutant allele uncut (523 bp) and giving digestion fragments of 140 and 383 bp for a normal allele. Restriction enzyme analysis with MaeIII was used to confirm the mutation in the patient and his family. Both parents (B1 and B2) and the unaffected brother (B4) of the patient were heterozygous carriers for this mutation, the patient (B5) was homozygous for the mutated allele, and his unaffected sister (B3) was homozygous for the normal allele.
Patient 1. CSGE analysis of exon 3 in patient 1 showed a heteroduplex band (fig. 3) and subsequent sequencing of genomic DNA showed a homozygous G-to-A substitution changing glycine codon 143 (GGG) to a codon for glutamic acid (GAG) (fig. 4). This mutation, designated G143E, abolishes a SacII restriction site (CCGCGG) resulting in an uncut 273 bp fragment in the mutant allele, and in 134 and 139 bp fragments in a normal allele. Digestion of PCR amplified genomic DNA with SacII confirmed the presence of this mutation on both alleles in patient 1 and established the patient’s father as a heterozygote carrier. The patient’s mother was not available for the study.
Patient 2. Patient 2 showed a heteroduplex band on CSGE analysis of exons 5–6 (fig. 3). Sequence analysis of the genomic fragment revealed a homozygous A-to-G mutation occurring at the invariant splice acceptor site sequence AG of intron 5. This mutation creates a new restriction site for the enzyme MspI and yields digestion fragments of 43, 48, 93 and 302 bp in the mutant allele, and 48, 93 and 345 bp in a normal allele. Digestion with MspI confirmed that patient 2 was homozygous for this change and that her mother carried the mutation. The father’s DNA was not available. This mutation has previously been described in patients with LI and has been shown to result in retention of intron 5 [14].
Complete screening of the 15 exons of TGK in patients A4, B5, 1 and 2 failed to detect any other nucleotide variation. To investigate whether the mutations that we identified could represent silent polymorphisms, we screened for their presence in 50 unrelated control individuals. Restriction analysis of corresponding amplified genomic fragments did not detect any of these mutations in the tested controls.
Absence of Detectable TGK Mutation in Patients C5, C6, D5 and 3
The 15 exons and flanking intronic sequences of the TGK gene were also amplified by PCR in patients C5, C6, D5 and 3, and screened for mutation using CSGE. CSGE analysis showed a normal migration pattern in these patients, except for patient D5 who displayed a shift in exon 7. Direct sequencing of exon 7 in this patient revealed a homozygous C-to-A substitution at the third base of glycine codon 381 (GGC) in comparison with the control. This variation, which does not predict a change of the encoded amino acid, creates a BpmI (or GsuI) site (CTGGAG) producing new digestion fragments of 123 and 400 bp. Restriction analysis was used to confirm this change in the patient and to screen for its presence in 50 control individuals. We found this variation to be present in 18% of the alleles tested, indicating that it is a polymorphism not associated with LI. In fact, the published sequence for glycine codon 381 in Genbank M86360 is (GGA) and thus corresponds to the rarer allele. Finally, direct sequencing of the 15 exons and flanking intronic regions of the TGK gene in patients C5, C6 and 3 showed no nucleotide variation in comparison with the control. In particular, none of the previously reported TGK mutations could be identified.
Immunofluorescence Staining, Transglutaminase Activity and Immunoblot Analysis
Protein studies were carried out in patients A4, B5, C5, C6 and 1. Skin biopsies from the other patients were not available for the study. Indirect immunofluorescence staining of skin biopsies with antibody B.C1 showed absence of staining in patients A4, B5 and 1, and normal staining for patients C5 and C6 (data not shown). TG activity assays and detection of TGK polypeptide by immunoblot were carried out from cultured keratinocytes as described in Methods. TG assays showed a profound reduction of membrane-bound as well as cytosolic TG activity in patients A4, B5 and 1 when compared to the controls (table 2). TG activity of both affected and unaffected skin from patients B5 was severely reduced. In contrast, TG activity was normal in patients C5 and C6 (data not shown). Immunoblot analysis of cytoplasmic and membrane keratinocyte extracts using the B.C1 monoclonal antibody revealed no detectable TGK protein in patients A4, B5 (affected and unaffected skin) and in patient 1 in comparison with the control (fig. 5a).
Expression of TGK polypeptide and TGK mRNA isolated from cultured keratinocytes from patients A4, B5, 1 and a control. a Immunoblot of cytosolic (lanes 1, 4, 6, 8 and 10) and membrane (lanes 2, 5, 7, 9 and 11) extracts from patient A4 (lanes 4 and 5), patient 1 (lanes 6 and 7), patient B5 (affected skin, lanes 8 and 9), patient B5 (non-affected skin, lanes 10 and 11), and unaffected control (lanes 1 and 2). No protein was loaded in lane 3. Protein (40 µg) from each extract was run on a 10% SDS-polyacrylamide gel and TGK protein was detected with antibody B.C1 [5, 28] and the ECL-Kit (Amersham). Molecular sizes (kilodaltons) are indicated on the left. b Northern blot analysis of 30 µg of total RNA hybridized with a α32P-dCTP-labelled TGM1 cDNA probe as described in Methods. TGM1 transcripts (2.8 kb in size) were clearly detectable in RNAs from the control (C) and patients B5 and 1, and at extremely low levels in patient A4. The amount of RNA loaded in each lane was evaluated by glyceraldehyde 3-phosphate dehydrogenase (GAPDH) hybridization (bottom). Density tracing analysis of the TGM1 signal to the GAPDH signal in patients B5 and 1 did not show any significant diminution in comparison to the control. Results shown for patient B5 correspond to keratinocytes from affected skin. Similar results were obtained with keratinocytes from unaffected skin from patient B5.
Northern Blot Analysis
Northern blot analysis from cultured keratinocytes was performed for patients A4, B5, 1 and a control. Keratinocytes were obtained from affected and unaffected skin from patient B5 and showed similar results. Patient A4 displayed a profound decrease in TGM1 transcript level when compared with the control (fig. 5b). In contrast, patients B5 (affected as well as unaffected skin) and patient 1 demonstrated TGM1 mRNA of normal size (2.8 kb) and comparable amounts with the age-matched control (fig. 5b). These results were obtained after standardization by GAPDH hybridization of the quantity of RNA present in each lane.
Discussion
We have investigated the involvement of TGK in 8 patients from 7 unrelated families with LI. We have described 4 patients who are homozygous for point mutations associated with TGK deficiency. Three of these mutations are novel and comprise a mutation affecting the binding site for Sp1 in the promoter region of TGK and two mutations predicting a single amino acid substitution. We have excluded linkage to the TGM1 locus in a further family, and have found no defect in the TGK gene in three other patients on the basis of TG activity assays and/or mutation screening. These results further support the involvement of TGK in some patients with LI, and provide evidence for different molecular mechanisms underlying TGK deficiency in LI.
To date, 21 mutations of the TGK gene have been reported in LI patients [14–20]. Of these mutations, 6 predict PTCs (2 nonsense mutations, 3 small frameshift deletions or insertions, and a splice acceptor site mutation resulting in intron retention). The other 15 mutations result in amino acid substitutions, a majority of which are localized in the β-sandwich or the core domain of the molecule. The consequences of these mutations on TGK transcript and protein activity have been reported in a limited number of cases [14]. In one, a homozygous 1-bp deletion was shown to result in mRNA instability leading to the absence of detectable TGK polypeptide, as previously described for frameshift mutations producing premature termination codons in other genes [30]. Three missense mutations resulted in the synthesis of detectable but non-functional TGK [14]. Finally, a splice acceptor site mutation gave rise to retention of intron 5 resulting in a PTC, with an absence of detectable TGK protein [14]. We have identified the same splice site mutation in patient 2, which was also recently reported in 3 further patients [18]. Interestingly, patients homozygous for this splice site mutation, including the 2 siblings reported by Huber et al. [14], presented either with classic LI or with erythrodermic LI, indicating that both phenotypes can be caused by the same TGK mutation.
The other 3 mutations that we report have not been previously described. These mutations are associated with lack of immunodetectable TGK and a profound reduction in TG activity. They are the only defects identified after screening all 15 exons of TGK, and were not found in any of the 50 controls studied. Therefore, it is unlikely that they represent silent polymorphisms. We hypothesize that the mutation of the Sp1 binding site in the promoter region of TGK impairs transcription of the gene and that the two missense mutations that we describe alter the structural integrity of the TGK polypeptide.
In patient A4, the mutation results in the modification of one of the two Sp1 sites (position −86 bp) in the promoter region of TGK [12]. This mutation is associated with a severe reduction of TGK transcripts, the absence of immunodetectable polypeptide and a profound decrease of TG activity, suggesting that TGK deficiency arises from a lack of mRNA template for protein synthesis. Sequence analysis did not reveal any nucleotide change at other putative regulatory elements within exon 1 (e.g. the other Sp1 binding site at position −61 bp, the KER1, CTF/NF1 and FP1 sequences at positions −266, −159 and −27 bp, respectively) (numbering as in Yamanashi et al. [12]). Similarly, sequence determination of all coding exons and splice site sequences of TGK failed to reveal any other nucleotide change. We therefore suggest that this mutation could affect promoter activity of the TGK gene by impairing binding of the Sp1 factor and its interaction with the RNA polymerase II and/or with other transcription factors. In favour of this interpretation, mutations of the Sp1 binding motif in the closely related TGM3 gene which shares common regulatory elements with TGK, have been shown to impair the binding of Sp1 on DNA and to abolish transcription of the TGM3 gene [31]. The relevance of these results to the TGK gene is unknown, and although other sites such as AP2-like sites located more upstream from the initiation codon have been shown to play an important role in the control of the expression of the TGK gene in vitro [32], the functional importance of Sp1 binding sites in expression of the gene has not been investigated. This first description of a naturally occurring mutation provides the opportunity for undertaking functional studies of this mutant and for a better understanding of the role of Sp1 in transcriptional regulation of the TGK gene.
In contrast with the mutation of the Sp1 site, the two novel missense mutations that we describe are associated with normal amounts of TGK mRNA, which is in agreement with the observation that missense mutations do not usually alter mRNA stability. However, both missense mutations led to the absence of immunodetectable TGK polypeptide, suggesting that they induce structural changes leading to instability of the mutated polypeptide. Alternatively, these defects may alter conformational epitopes of TGK. Gly143Glu and Val382Met are non-conservative substitutions occurring in two highly evolutionary conserved regions of TGK (table 3). The Gly143Glu mutation identified in patient 1 is located within the β-sandwich domain of the polypeptide within an ArgArg-GlyGln sequence, conserved among human TGs and between species [15]. According to the structural model common to TGs, this motif is part of a β-turn/β-strand structure [13, 15]. Replacement of glycine 143 by a glutamic acid residue introduces a bulky and negatively charged side chain capable of establishing ionic interactions with neighbouring amino acid residues. The ArgArg-GlyGln motif is located in a region of the molecule which has been shown by deletion mapping to be essential for normal TG activity [33]. Thus, it is possible that the alteration of amino acid size and chemical properties in this region could interfere with protein folding and/or lead to a destabilized molecule. It is also of interest that a mutation changing the same glycine residue 143 to an arginine has recently been reported in another patient with LI [18], and that this mutation is neighbouring arginines 141 and 142 which have recently been identified as mutational hotspots in LI [14, 19]. These results raise the possibility that glycine 143 may belong to a region of the TGK polypeptide important for its structure and function.
The Val382Met mutation identified in patient B5 occurs in exon 7 in the core domain of the TGK. This substitution replaces a hydrophobic valine residue by a slightly larger hydrophobic methionine residue within an evolutionary conserved region located four amino acids downstream of the consensus sequence Tyr-Gly-Gln-Cys-Trp encoding the active site of TGK. This mutation leads to very low or undetectable protein levels, which suggests that despite the less drastic change in the nature of the amino acid substitution, it is also predicted to alter a motif of the molecule important for structural integrity of the polypeptide. Interestingly, patient B5 is affected with a particular form of ichthyosis involving the neck, the scalp and the trunk, but remarkably sparing the face and the four limbs (fig. 2). Similar cases have been observed by others [Prof. Marc Larrègue, pers. commun.], and despite the absence of consensus for the classification of LI, the clinical aspect of the scales and the absence of redness of the skin is more suggestive of LI than congenital ichthyosiform erythroderma. Moreover, the demonstration in patient B5 of a defect in the TGK gene associated with TGK deficiency further supports the possibility that this patient is affected with a particular form of LI. These results further illustrate the phenotypic variability of LI and provide the first evidence for the involvement of TGK in this rare form of the disease. It is noteworthy that the presence of the Val382Met mutation was confirmed in cDNA from keratinocytes of affected as well as from unaffected skin of the patient, thus demonstrating that the defect is expressed in non-affected skin as confirmed by protein analysis. This suggests that other mechanisms compensate for TGK deficiency in unaffected skin, and raises the possibility that the regulation of the formation of the cornified envelope could differ between these different areas of the skin.
TGK was excluded as the disease gene in the other 4 patients studied. In the case of siblings C5 and C6, haplotype analysis using the (CA)n microsatellite repeat within the TGK gene was compatible with linkage, but the involvement of TGK could be excluded on the basis of TG activity assays and by sequencing of the 15 TGK exons. In family D, haplotype analysis excluded linkage to the TGM1 locus and sequencing of the shift in exon 7 identified no causative mutation, only a polymorphic C-to-A change which was also detected in normal controls. In patient 3, sequence analysis of the TGK gene revealed no change in comparison with the control, making TGK involvement in the disease unlikely. Interestingly, patients C5 and C6 were affected with classical LI, whereas patients D5 and 3 presented moderate LI with finer scaling and variable erythema. This suggests that both clinical presentations may be due to defects in genes different from TGK. Linkage studies, together with mutation and enzymatic analysis of additional patients, are required to determine to what extent TGK is involved in each phenotype.
We also tested patients C5, C6, D5 and 3 for linkage to the chromosomal region 2q33–35 where a second locus has been reported [22]. Linkage to this region of chromosome 2 could be excluded in patient D5 who shared the same genotype with her unaffected brother, and by homozygosity mapping in patients C5, C6 and 3 (data not shown). These results indicate that at least a third locus should be involved in these LI patients. Possible candidate loci include the TGM2 and TGM3 genes which encode other epidermally expressed TGs [6]. Both localize to chromosome 20q11.2, a region for which linkage was recently excluded by Bale et al. [34] in two families with a form of congenital recessive ichthyosis distinct from classic LI.
Finally, due to genetic heterogeneity of the disease, the investigation of TG activity in patients with LI will help to distinguish between LI due to TGK deficiency from forms of the disease due to defects in so far unidentified genes. The delineation of TGK mutations will help to identify regions of the molecule wich may be important for the normal expression, the stability, the conformation and the function of the TGK polypeptide. Overall, knowledge of TGK mutations will improve genetic counselling in families at risk of recurrence of LI and provides the possibility of DNA-based prenatal diagnosis for this severe skin disorder.
References
Williams ML, Elias PM: Genetically transmitted, generalized, disorders of cornification; in Alper JC (ed): Dermatologic Clinics. Philadelphia, Saunders, 1987, vol 5, pp 155–178.
Traupe H: The lamellar ichthyoses; in Traupe H (ed): The Ichthyoses: A Guide to Clinical Diagnosis, Genetic Counseling, and Therapy. Berlin, Springer-Verlag, 1989, pp 111–134.
Reichert U, Michel S, Schmidt R: The cornified envelope: A key structure of terminally differentiating keratinocytes; in Darmon M, Blumenberg M (eds): Molecular biology of the skin. San Diego, Academic Press, 1993, pp 107–150.
Rice RH, Green H: Relation of protein synthesis and transglutaminase activity to formation of the cross-linked envelope during terminal differentiation of the cultured human epidermal keratinocyte. J Cell Biol 1978;76:705–711.
Thacher SM, Rice RH: Keratinocyte-specific transglutaminase of cultured human epidermal cells: Relation to cross-linked envelope formation and terminal differentiation. Cell 1985;40: 685–695.
Polakowska RR, Goldsmith LA: The cell envelope and transglutaminases; in Goldsmith LA (ed): Physiology, biochemistry, and molecular biology of the skin. New York, Oxford University Press, 1991, vol 1, pp 168–201.
Steven AC, Steinert PM: Protein composition of the cornified cell envelope of epidermal keratinocytes. J Cell Sci 1994;107:693–700.
Hohl D, Huber M, Frenk E: Analysis of the cornified cell envelope in lamellar ichthyosis. Arch Dermatol 1993;129:618–624.
Lavrijsen S, Maruyama T: Absent transglutaminase TGK expression in 2 out of 3 patients with lamellar ichthyosis. Arch Dermatol 1995; 434:363–364.
Russell LJ, DiGiovanna JJ, Hashem N, Compton JG, Bale SJ: Linkage of autosomal recessive lamellar ichthyosis to chromosome 14q. Am J Hum Genet 1994;55:1146–1152.
Kim IG, McBride OW, Wang M, Kim SY, Idler WW, Steinert PM: Structure and organization of the human transglutaminase 1 gene. J Biol Chem 1992;7710–7717.
Yamanishi K, Inazawa J, Liew F-W, Nonomura K, Ariyama T, Yasuno H, Abe T, Doi H, Hirano J, Fukushima S: Structure of the gene for transglutaminase 1. J Biol Chem 1992;267: 17858–17863.
Yee VC, Pedersen LC, Le Trong I, Bishop PD, Stenkamp RE, Teller DC: Three dimensional structure of a transglutaminase: Human blood coagulation factor XIII. Proc Natl Acad Sci USA 1994;91:7296–7300.
Huber M, Rettler I, Bernasconi K, Frenk E, Lavrijsen SPM, Ponec M, Bon A, Lautenschlager S, Schorderet DF, Hohl D: Mutations of keratinocyte transglutaminase in lamellar ichthyosis. Science 1995;267:525–528.
Russell LJ, DiGiovanna JJ, Rogers GR, Steinert PM, Hashem N, Compton JG, Bale SJ: Mutations in the gene for transglutaminase 1 in autosomal recessive lamellar ichthyosis. Nature Genet 1995;9:279–283.
Parmentier L, Blanchet-Bardon C, Nguyen S, Prud’homme J-F, Dubertret L, Weissenbach J: Autosomal recessive lamellar ichthyosis: identification of a new mutation in transglutaminase 1 and evidence for genetic heterogeneity. Hum Mol Genet 1995;4:1391–1395.
Bichakjian CK, Wu WW, Elder JT, Nair RP: Two new mutations in the transglutaminase 1 gene in a lamellar ichthyosis kindred (abstract). J Invest Dermatol 1996;106:905.
Hennies H-C, Mackova A, Ehrig T, Küster W, Reis A: Genotype/phenotype correlation in autosomal recessive lamellar ichthyosis (LI) caused by TGM1 gene mutations and evidence for genetic heterogeneity of LI (abstract). Eur J Hum Genet 1996;4 (suppl 1):S4.002.
Laiho E, Igniatius J, Mikkola H, Niemi K-M, Saarialho-Kere U, Kere J, Palotie A: A mutational hotspot in the transglutaminase 1 gene revealed by the study of an isolated population (abstract). Am J Hum Genet 1996(suppl 59): A267.
Russell LJ, Whyte YM, DiGiovanna JJ, Hashem N, Bale SJ, Compton JG: Mutation screening of the transglutaminase 1 gene in patients with lamellar ichthyosis (LI) and other congenital recessive ichthyosis using dideoxy fingerprinting (abstract). J Invest Dermatol 1996;106:843.
Huber M, Rettler I, Bernasconi K, Wyss M, Hohl D: Lamellar ichthyosis is genetically heterogeneous. Cases with normal keratinocyte transglutaminase. J Invest Dermatol 1995; 105: 653–654.
Parmentier L, Lakhdar H, Blanchet-Bardon C, Marchand S, Dubertret L, Weissenbach J: Mapping of a second locus for lamellar ichthyosis to chromosome 2q33–35. Hum Mol Genet 1996;5:555–559.
John SWM, Weitzner G, Rozen R, Scriver CR: A rapid procedure for extracting genomic DNA from leukocytes. Nucleic Acids Res 1991; 19: 408.
Church GM, Gilbert W: Genomic sequencing. Proc Natl Acad Sci USA 1984;81:1991–1995.
Ganguly A, Rock MJ, Prockop DJ: Conformation-sensitive gel electrophoresis for rapid detection of single-base differences in double-stranded PCR products and DNA fragments: Evidence for solvent-induced bends in DNA heteroduplexes. Proc Natl Acad Sci USA 1993; 90:1035–1039.
Rheinwald JG, Green H: Serial cultivation of strains of human epidermal keratinocytes: The formation of keratinizing colonies from single cells. Cell 1975;6:331–334.
Thacher SM: Purification of keratinocyte transglutaminase and its expression during squamous differentiation. J Invest Dermatol 1989;89:578–584.
Lichti U, Ben T, Yuspa SH: Retinoic acid-induced transglutaminase in mouse epidermal cells is distinct from epidermal transglutaminase. J Biol Chem 1985;260:1422–1426.
Chomczynski P, Sacchi N: Single step method of RNA isolation of acid guanidium thiocyanate-phenol-chloroform extraction. Anal Biochem 1987;162:156–159.
Maquat LE: When cells stop making sense: Effect of non-sense codons on RNA metabolism in vertebrate cells. RNA 1995;1:453–465.
Lee J-H, Jang S-I, Yang J-M, Markova NG, Steinert PM: The proximal promoter of the human transglutaminase 3 gene. Stratified squamous epithelial-specific expression in cultured cells is mediated by binding of Sp1 and ets transcription factors to a proximal promoter element. J Biol Chem 1996;271:4561–4568.
Mariniello L, Qin Q, Jessen BA, Rice RH: Keratinocyte transglutaminase promoter analysis. Identification of a functional response element. J Biol Chem 1995;270:31358–31363.
Kim SY, Kim IG, Chung SI, Steinert PM: The structure of the transglutaminase 1 enzyme. Deletion cloning reveals domains that regulate its specific activity and substrate specificity. J Biol Chem 1994;269:27979–27986.
Bale JS, Russell LJ, Lee ML, Compton JG, DiGiovanna JJ: Congenital recessive ichthyosis unlinked to loci for epidermal transglutaminases. J Invest Dermatol 1996;107:808–811.
Acknowledgements
We are grateful to the patients and their families for their collaboration. We would like to acknowledge Richard Wade-Martins for helpful discussion. This work was supported by grants from the Well-come Trust, the Swiss National Science Foundation, the Institut National de la Santé et de la Recherche Médicale (INSERM) and the Association pour la Recherche contre le Cancer (ARC). E.P. is supported by a fellowship of Fondation France Telecom. A. H. held an EEC research fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petit, E., Huber, M., Rochat, A. et al. Three Novel Point Mutations in the Keratinocyte Transglutaminase (TGK) Gene in Lamellar Ichthyosis: Significance for Mutant Transcript Level, TGK Immunodetection and Activity. Eur J Hum Genet 5, 218–228 (1997). https://doi.org/10.1007/BF03405921
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03405921