Abstract
OBJECTIVE:
To compare growth and neurodevelopment in surviving very low birth weight (VLBW) infants with an intestinal perforation (IP) caused by necrotizing enterocolitis (NEC) versus spontaneous intestinal perforation (SIP).
STUDY DESIGN:
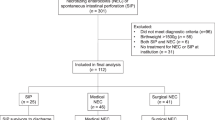
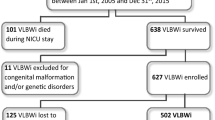
Retrospective, observational cohort study. Infants born between January 1996 and December 1999 with birth weight <1500?g and a diagnosis of intestinal perforation were identified and data extracted from NICU, surgical and hospital databases.
RESULTS:
IP was identified in 62 of 1357 VLBW infants (5%); 39 infants (63%) had surgical NEC and 23 (37%) had SIP. Among survivors, 21/28 with surgical NEC (75%) and 13/18 with SIP (72%) returned for follow-up. At 1-year adjusted age, there were no differences in growth parameters but the Mental Developmental Index (MDI) and Psychomotor Developmental Index (PDI) were lower in survivors with NEC versus SIP (mean difference in MDI=15; 95% confidence limits=3, 28; p=0.02; mean difference in PDI=14; 95% confidence limits=0.4, 28; p=0.04).
CONCLUSIONS:
Intestinal perforation caused by NEC, as compared to SIP, is associated with worse neurodevelopmental outcome at 1 year.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kliegmann RM, Faranoff AA . Neonatal necrotizing enterocolitis: a nine-year experience, part 1/2. Am J Dis Child 1981;135:603–611.
Aschner JL, Deluga KS, Metlay LA, Emmens RW, Hendricks-Munoz KD . Spontaneous focal perforation in very low birth weight infants. J Pediatr 1988;113:364–367.
Meyers CL, Payne NR, Roback SA . Spontaneous isolated intestinal perforation in neonates with birth weight <1,000?g, not associated with necrotizing enterocolitis. J Pediatr Surg 1991;26:714–717.
Adderson EE, Pappin A, Pavia AT . Spontaneous intestinal perforation in premature infants: a distinct clinical entity associated with systemic candidiasis. J Pediatr Surg 1998;33:1463–1467.
Buchheit JQ, Stewart DL . Clinical comparison of localized intestinal perforation and necrotizing enterocolitis in neonates. Pediatrics 1994;93:32–36.
Touloukian RJ . Gastric Ischemia: the primary factor in neonatal perforations. Clin Pediatr 1973;12:219–225.
Borzotta AP, Groff DB . Gastrointestinal perforation in infants. Am J Surg 1988;155:447–452.
Ladd AP, Rescorla FJ, West KW, Scherer III LR, Engum SA, Grosfeld JL . Long-term follow-up after resection for necrotizing enterocolitis: factors affecting outcome. J Pediatr Surg 1998;33:967–972.
Walsh MC, Kliegman RM, Hack M . Severity of necrotizing enterocolitis: influence on outcome at 2 years of age. Pediatrics 1989;84:808–814.
Vohr BR, Wright LL, Dusick AM, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Developmental Neonatal Research Network, 1993–1994. Pediatrics 2000;105:1216–1226.
Sonntag J, Grimmer I, Scholz T, Metze B, Wit J, Obladen M . Growth and neurodevelopmental outcome of very low birth weight infants with necrotizing enterocolitis. Acta Paediatr 2000;89:528–532.
Salhab WA, Perlman JM, Silver L, Broyles RS . Necrotizing enterocolitis and neurodevelopmental outcome in extremely low birth weight infants <1000?g. J Perinatol 2004;24:534–540.
Bell MJ . Perforation of the gastrointestinal tract and peritonitis in the neonate. Surg Gynecol Obstet 1985;160:20–26.
Hamill PVV, Drizd TA, Johnson CL, Reed RB, Roche AF, Moore WM . Physical growth: National Center for Health Statistics percentiles. Am J Clin Nutr 1979;32:607–629.
Stark AR, Carlo WA, Tyson JE, et al. Adverse effects of early dexamethasone in extremely low birth weight infants. National Institute of Child Health and Human Development Neonatal Research Network. N Engl J Med 2001;344:95–101.
Gordon PV, Young ML, Marshall DD . Focal small bowel perforation: an adverse effect of early postnatal dexamethasone therapy in extremely low birth weight infants. J Perinatol 2001;21:156–160.
Halliday HL, Ehrenkranz RA . Early postnatal (<96 hours) corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev 2000;2:CD001146 Review. Update in: Cochrane Database Syst Rev. 2001; 1: CD001146.
Watterberg KL, Gerdes JS, Cole CH, et al. Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial. Pediatrics 2004;114:1649–1657.
Kothadia JM, O'Shea TM, Roberts D, Auringer ST, Weaver III RG, Dillard RG . Randomized placebo-controlled trial of a 42-day tapering course of dexamethasone to reduce the duration of ventilator dependency in very low birth weight infants. Pediatrics 1999;104:22–27.
Hack M, Breslau N, Weissman B, Aram D, Klein N, Borawski E . Effect of very low birth weight and subnormal head size on cognitive abilities at school age. N Engl J Med 1991;325:231–237.
Acknowledgements
We thank Nancy Peters for her assistance in identifying study subjects, and Barbara Jackson, Robert Dillard, Kurt Klinepeter and Donald Goldstein for performing follow-up assessments on the study subjects. This study was funded in part by the North Carolina Department of Health and Human Services.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Adesanya, O., O'Shea, T., Turner, C. et al. Intestinal Perforation in Very Low Birth Weight Infants: Growth and Neurodevelopment at 1 Year of Age. J Perinatol 25, 583–589 (2005). https://doi.org/10.1038/sj.jp.7211360
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211360
This article is cited by
-
Neurodevelopmental outcome of very preterm infants with gastrointestinal tract perforations does not differ compared to controls
Wiener klinische Wochenschrift (2021)
-
Preterm birth and sustained inflammation: consequences for the neonate
Seminars in Immunopathology (2020)
-
Management of neonatal spontaneous intestinal perforation by peritoneal needle aspiration
Journal of Perinatology (2018)
-
Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis
Journal of Perinatology (2014)
-
Hospital and neurodevelopmental outcomes of extremely low-birth-weight infants with necrotizing enterocolitis and spontaneous intestinal perforation
Journal of Perinatology (2012)