Abstract
BACKGROUND: Inhaled nitric oxide (iNO) is a potent and selective pulmonary vasodilator that decreases pulmonary resistance, and improves ventilation-perfusion matching, thereby improving oxygenation and reducing the need for more invasive therapies. Despite the efficacy of iNO at reducing the use of extracorporeal membrane oxygenation, significant concern remains over the potential toxicity from oxidative derivatives and methemoglobinemia. At present, there is no universal agreement on the lowest effective starting dose. Reported initial doses in the neonatal literature have ranged from 1 to 80 ppm.
PURPOSE: To determine if the initial dose of iNO altered the incidence of adverse outcome.
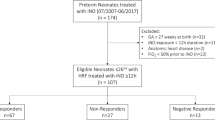
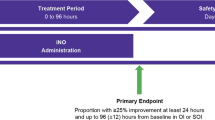
METHODS: A cohort of neonates who received iNO for treatment of hypoxic respiratory failure and were entered into the Duke Neonatal Nitric Oxide Registry were evaluated. Neonates with congenital anomalies were excluded. This registry collects data from 36 centers that voluntarily report their experiences with iNO. From this database, the starting dose was recorded and the clinical course was followed. Adverse outcomes were prospectively defined and monitored in the database and included: methemoglobinemia, chronic lung disease, treatment with extracorporeal membrane oxygenation, or death.
RESULTS: Data on 476 patients were analyzed. Based on starting doses, records were sorted into three groups: a low-dose group (LDG; <18 ppm, n=57), a mid-dose group (MDG; 18 to 22 ppm, n=320), and a high-dose group (HDG; >22 ppm, n=99). ANOVA showed no statistically significant differences among the groups except for PaO2/FiO2 (p<0.05). Neonates in the high starting dose group were more often classified as treatment failures (21% in the LDG, 27% in the MDG, and 38% in the HDG, p=0.04) and treated with extracorporeal membrane oxygenation (19% in the LDG, 23% in the MDG, and 34% in the HDG, p=0.05) compared to the lower dose groups. In addition, survival without the need for oxygen at 30 days or at discharge was higher in the lower dose groups (93% in the LDG, 84% in the MDG, and 76% in the HDG, p=0.03). Logistic regression, however, showed that the starting dose of iNO did not significantly influence these outcomes when corrected for the degree of hypoxemia (PaO2/FiO2) at the start of therapy (p>0.1). High initial doses of iNO (>22 ppm) were associated with higher levels of methemoglobin (p< 0.05). There were no differences in mortality or length of hospital stay between the groups.
CONCLUSIONS: There is significant variation in the starting dose of iNO between centers. Our retrospective study shows no evidence that higher doses improve outcome. A low concentration of iNO (<18 ppm) should be considered to minimize the potential toxicity of methemoglobin. Furthermore, a well-designed, prospective trial should be undertaken to further define the optimal starting dose.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Kinsella JP, Neish SR, Shaffer E, Abman SH . Low-dose inhalation nitric oxide in persistent pulmonary hypertension of the newborn. Lancet 1992;340:819–820.
Roberts JD, Polaner DM, Lang P, Zapol WM . Inhaled nitric oxide in persistent pulmonary hypertension of the newborn. Lancet 1992;340:818–819.
Clark RH, Kueser TJ, Walker MW, et al. Low-dose nitric oxide therapy for persistent pulmonary hypertension of the newborn. Clinical Inhaled Nitric Oxide Research Group. N Engl J Med 2000;342:469–474.
Cornfield DN, Maynard RC, deRegnier RA, Guiang III SF, Barbato JE, Milla CE . Randomized, controlled trial of low-dose inhaled nitric oxide in the treatment of term and near-term infants with respiratory failure and pulmonary hypertension. Pediatrics 1999;104:1089–1094.
Davidson D, Barefield ES, Kattwinkel J, et al. Inhaled nitric oxide for the early treatment of persistent pulmonary hypertension of the term newborn: a randomized, double-masked, placebo-controlled, dose-response, multicenter study. The I-NO/PPHN Study Group. Pediatrics 1998;101:325–334.
Finer NN, Sun JW, Rich W, Knodel E, Barrington KJ . Randomized, prospective study of low-dose versus high-dose inhaled nitric oxide in the neonate with hypoxic respiratory failure. Pediatrics 2001;108:949–955.
Wessel DL, Adatia I, Van Marter LJ, et al. Improved oxygenation in a randomized trial of inhaled nitric oxide for persistent pulmonary hypertension of the newborn. Pediatrics 1997;100:E7.
Wood KS, McCaffrey MJ, Donovan JC, Stiles AD, Bose CL . Effect of initial nitric oxide concentration on outcome in infants with persistent pulmonary hypertension of the newborn. Biol Neonate 1999;75:215–224.
Finer NN, Barrington KJ . Nitric oxide for respiratory failure in infants born at or near term. Cochrane Database Syst Rev 2001. CD000399.
Fortenberry JD, Owens ML, Brown LA . S-nitrosoglutathione enhances neutrophil DNA fragmentation and cell death. Am J Physiol 1999;276:L435–L442.
Fortenberry JD, Owens ML, Brown MR, Atkinson D, Brown LA . Exogenous nitric oxide enhances neutrophil cell death and DNA fragmentation. Am J Respir Cell Mol Biol 1998;18:421–428.
Gutierrez HH, Nieves B, Chumley P, Rivera A, Freeman BA . Nitric oxide regulation of superoxide-dependent lung injury: oxidant-protective actions of endogenously produced and exogenously administered nitric oxide. Free Radic Biol Med 1996;21:43–52.
Kinsella JP, Walsh WF, Bose CL, et al. Inhaled nitric oxide in premature neonates with severe hypoxaemic respiratory failure: a randomised controlled trial. Lancet 1999;354:1061–1065.
Acknowledgements
We acknowledge Dr. Robert B. Cotton for his careful review of this manuscript.
Author information
Authors and Affiliations
Additional information
The Duke Neonatal Nitric Oxide Registry is funded by a grant from INO Therapeutics.
Rights and permissions
About this article
Cite this article
Guthrie, S., Walsh, W., Auten, K. et al. Initial Dosing of Inhaled Nitric Oxide in Infants with Hypoxic Respiratory Failure. J Perinatol 24, 290–294 (2004). https://doi.org/10.1038/sj.jp.7211087
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211087
This article is cited by
-
Rapid Formation of Methemoglobin via Nitric Oxide Delivery for Potential Use as an MRI Contrast Agent
Annals of Biomedical Engineering (2023)
-
Methemoglobin to cumulative nitric oxide ratio and response to inhaled nitric oxide in PPHN
Journal of Perinatology (2009)
-
Role of iNO in the modulation of pulmonary vascular resistance
Journal of Perinatology (2008)
-
Hypoxic respiratory failure: etiology and outcomes at one referral center 2000 through 2005
Journal of Perinatology (2007)
-
Emerging trends in acquired neonatal intestinal disease: is it time to abandon Bell's criteria?
Journal of Perinatology (2007)