Abstract
OBJECTIVE: Critically ill neonates frequently require multiple small volume red blood cell (RBC) transfusions. RBC units assigned to individual infants, used sequentially in small aliquots until the original expiration date, can substantially reduce donor exposures. In 1993, adenine–saline solution (AS-3) was introduced by the Canadian Red Cross as the red cell storage medium to replace citrate–phosphate–dextrose–adenine anticoagulant–preservative solution (CPDA-1). We surveyed the safety and efficacy of using AS-3 split packs, stored up to 35 days, for premature infants.
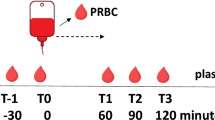
STUDY DESIGN: Units of packed cells were aseptically welded to three satellite bags using a sterile connecting device. When blood was requested for a small volume transfusion, the first satellite bag was used and the others were set aside for the same baby, for use up until their expiration date of 35 days.
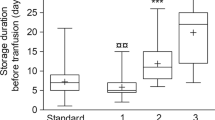
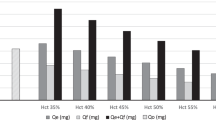
RESULTS: Over a 1-year period, 56 infants received a total of 263 AS-3 transfusions from 97 donors, with a mean of 4.7 transfusions and 1.7 donor exposures per infant. Following a 7-ml/kg RBC transfusion, mean rise in hematocrit (hct) was 0.04, regardless of the age of the unit, mean change in serum potassium was −0.16 mmol/l and mean change in total bilirubin was +1.86 μmol/l. The posttransfusion hct was not reduced with the use of the older red cell packs.
CONCLUSION: Designated AS-3–preserved split RBC packs effectively limit donor exposures, can safely be used for neonatal small volume transfusions, and give a constant transfusion effect after up to 35 days of storage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Levy GJ, Strauss RG, Hume H, et al National survey of neonatal transfusion practices: I. Red blood cell therapy Pediatrics 1993 91 523–9
Luban NLC, Strauss RG, Hume HA Commentary on the safety of red cells preserved in extended-storage media for neonatal transfusions Transfusion 1991 31 229–35
Cook S, Gunter J, Wissel M Effective use of a strategy using assigned red cell units to limit donor exposure for neonatal patients Transfusion 1993 33 379–83
Wood A, Wilson N, Skacel P, et al Reducing donor exposure in preterm infants requiring multiple blood transfusions Arch Dis Child Fetal Neonat Ed 1995 72 F29–33
Liu EA, Mannino FL, Lane TA Prospective, randomized trial of the safety and efficacy of a limited donor exposure transfusion program for premature neonates J Pediatr 1994 125 92–6
Strauss RG, Burmeister LF, Johnson K, et al AS-1 red cells for neonatal transfusions: a randomized trial assessing donor exposure and safety Transfusion 1996 36 873–8
Wang-Rodriguez J, Mannino FL, Liu E, Lane TA A novel strategy to limit blood donor exposure and blood waste in multiply transfused premature infants Transfusion 1996 36 64–70
Patten E, Robbins M, Vincent J, et al Use of red cells older than five days for neonatal transfusion J Perinatol 1991 11 37–40
Strauss RG, Burmeister L, James T, et al A randomized trial of fresh versus stored RBCs for neonatal transfusions Transfusion 1994 34 (suppl) 65S (Abstract)
Eshleman JR, Akinbi H, Pleasure J, et al Prospective doubleblind study of small volume neonatal transfusion with red blood cells up to 35 days old Transfusion 1994 34 (suppl) 32S (Abstract)
Lee DA, Slagle TA, Jackson TM, Evans CS Reducing blood donor exposures in low birth weight infants by the use of older, unwashed packed red blood cells J Pediatr 1995 126 280–6
Strauss RG, Burmeister LF, Johnson K, et al Feasibility and safety of AS-3 red blood cells for neonatal transfusions J Pediatr 2000 136 215–9
Donowitz LG, Turner RB, Searcy MA, et al The high rate of blood donor exposure for critically ill neonates Infect Control Hosp Epidemiol 1989 10 509–10
Strauss RG Red blood cell transfusion practices in the neonate Clin Perinatol 1995 22 641–55
Strauss RG, Sacher RA, Blazina JF, et al Commentary on small volume red cell transfusions for neonatal patients Transfusion 1990 30 565–70
Holman P, Blajchman MA, Heddle N Noninfectious adverse effects of blood transfusion in the neonate Transfus Med Rev 1995 9 277–87
Goodstein MH, Locke RG, Wlodarczyk D, et al Comparison of two preservation solutions for erythrocyte transfusions in newborn infants J Pediatr 1993 123 783–8
Bifano EM, Curran TR Minimizing donor blood exposure in the neonatal intensive care unit. Current trends and future prospects Clin Perinatol 1995 22 557–669
Acknowledgements
The authors thank Robert Usher, Director of the Royal Victoria Hospital Neonatal Intensive Care Unit.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mangel, J., Goldman, M., Garcia, C. et al. Reduction of Donor Exposures in Premature Infants by the Use of Designated Adenine–Saline Preserved Split Red Blood Cell Packs. J Perinatol 21, 363–367 (2001). https://doi.org/10.1038/sj.jp.7210545
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7210545
This article is cited by
-
A cost-analysis study of using adult red cell packs and Pedi-Packs in newborn intensive care units in Southern Iran
Cost Effectiveness and Resource Allocation (2021)
-
Effect of red blood cell storage time on markers of hemolysis and inflammation in transfused very low birth weight infants
Pediatric Research (2017)
-
Health Care-Associated Infections in Children After Cardiac Surgery
Pediatric Cardiology (2014)