Abstract
Purpose
To study the prevalence and associations of dry eye symptoms in adult Chinese.
Methods
The Beijing Eye Study is a population-based study in northern China, which included 4439 of 5324 subjects invited to participate with an age of 40+ years (response rate: 83.4%). For the present study, a random sample was taken consisting of 1957(44.1%) subjects (1112 women; 56.9%). Dry eye symptoms were evaluated with (1) an interviewer-assisted questionnaire; (2) measurement of the tear-film break-up time; (3) assessment of the fluorescein staining of the cornea; (4) slit-lamp-based examination of a meibomian gland dysfunction; and (5) Schirmer's test.
Results
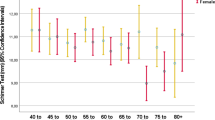
Symptoms of a dry eye felt ‘often’ or ‘at all times’ were present in 411 subjects (21.0%). In a multivariate analysis, dry eye symptoms were significantly associated with age (P<0.001), female gender (P<0.001; odds ratio (OR): 1.56; 95% confidence intervals (CI): 1.23, 1.98), urban region (P<0.001;OR: 1.89; 95% CI: 1.46, 2.48), low degree of nuclear cataract (P=0.02), and undercorrection of refractive error (P=0.005; OR: 1.42; 95% CI: 1.11, 1.82). All tests for dry eye did not vary significantly between the dry eye group and the normal group.
Conclusions
The dry eye symptoms as evaluated subjectively in a questionnaire occurred in about 21% of the adult population in China, with associations to age, female gender, urban region, and undercorrection of a refractive error. Measurement of the tear-film break-up time, assessment of the corneal fluorescein staining, slit-lamp-based examination of a meibomian gland dysfunction, and Schirmer's test were not significantly associated with dry eye symptoms.
Similar content being viewed by others
Introduction
Dry eye symptoms belong to the most frequently encountered ocular problems that patients complain about in the daily practice of ophthalmologists.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 Although these symptoms rarely lead to severe problems threatening vision, they may be one of the most common symptoms decreasing the quality of vision. In view of their importance for daily life of patients and ophthalmologists, in practice it was the purpose of the present study to examine the prevalence of dry symptoms and their associations with ocular and general parameters in a population-based study in mainland China. An additional goal of the study was to evaluate which commonly used test of the ocular surface was most suitable to assess a dry eye symptom as reported by the subjects.
Methods
The Beijing Eye Study is a population-based study in northern China performed in 2001. It was carried out in four communities in the urban districts of Xicheng and Haidian, which were in the centre of Beijing, and in three communities in the village area of Yufa of the Daxing district, south of Beijing. The rural communities, the inhabitants of which mainly lived from farming, were located about 50 km from central Beijing and were easily accessible by car in about 1 h via an express autobahn. The mean family income was significantly higher in the urban region (1688±4134 RMB) than in the rural region (393±360 RMB). All people living in the seven communities were officially registered by name, gender, and age at the local mayor's office. Using this register as the sampling frame, all subjects living in the seven communities and fulfilling the inclusion criterion of an age of 40+ years were eligible for the study. Because of the registration list at the mayor's office, the boundaries of the communities and the size of the population of each of the communities were known before the start of the study. Home visits were performed according to the registration list, and the eligibility criterion for the study, an age of 40+ years, was confirmed by door-to-door enrolment. The door-to-door visitation included all houses in the communities, and the registration list of the inhabitants served to have an overview of who is residing in each of the houses. The eligible subjects were visited up to three times if they did not participate after the first visit in the Beijing Eye Study. The study has been described in detail recently.15, 16 The Medical Ethics Committee of the Beijing Tongren Hospital had approved the study protocol and all participants had given informed consent, according to the Declaration of Helsinki.
At the time of the survey in 2001, there were 5324 individuals aged 40+ years residing in the seven communities. In total, 4439 individuals (2505 women) participated in the eye examination, corresponding to an overall response rate of 83.4%. The study was divided into the rural part (1918 (43.8%) subjects; 3814 eyes) and the urban part (2460 (56.2%) subjects; 4910 eyes). Mean age was 56.2±10.6 years (range: 40–101 years). A detailed ophthalmic examination was carried out including measurement of uncorrected and best-corrected visual acuity, noncontact tonometry (CT-60 computerized tonometer, Topcon Ltd, Japan), frequency doubling perimetry using the screening program C-20-1 (Zeiss-Humphrey, Dublin, CA, USA), slit-lamp examination of the anterior segment, ophthalmoscopy, digital photography of the lens (Neitz CT-R camera; Neitz Instruments Co, Tokyo, Japan), and photography (45°) of the optic disc and macula (fundus camera, type CR6-45NM, Canon Inc. USA) after medical mydriasis. Past history of eye diseases, eye trauma, diabetes mellitus, hypertension, any ophthalmologic care that the participant received, professions, educational level of the participants, habit of smoking, and alcohol intake were recorded.
In addition, in a random sample of study participants, dry eye symptoms were evaluated with (1) an interviewer-assisted questionnaire (Table 1), (2) measurement of the tear-film break-up time, (3) assessment of fluorescein staining of the cornea, (4) examination of a meibomian gland dysfunction, and (5) Schirmer's test. For each study participant, both eyes were tested, and the data of the worse eyes were taken for statistical analysis. The tear-film break-up time test was performed before the other dry eye tests to avoid any interference between the tests. The tear-film break-up test was repeated three times for each eye, and the average time was recorded. Fluorescein staining of the cornea was observed through a slit lamp with a cobalt blue filter and was graded as ‘0’ for ‘no staining’, as ‘1’ for ‘mild staining with a few disseminated stains, and limited to less than one-third of the cornea’, as ‘2’ for ‘moderate staining with a severity between grades 1 and 3’, or as ‘3’ for ‘severe staining with confluent stains, and occupying half or more of the cornea’. The condition of the meibomian glands was determined by examining the lid margin with a slit lamp. As there has not been any generally accepted grading system for meibomian gland dysfunction, we defined meibomian gland dysfunction as the presence of a plugging of the meibomian gland orifices or as telangiectasias at the lid margin. The presence of lid margin telangiectasia was recorded, and the meibomian gland orifices were graded using a scale of ‘0’ for ‘no obstruction’, grade 1 for ‘plugged with translucent serous secretion when the lid margin was compressed’, grade 2 as ‘plugged with viscous or waxy white secretion when the lid margin was compressed’, and as grade 3 for ‘plugged with no secretion when the lid margin was compressed’. The Schirmer's test was performed at the end of the examination, so that ocular irritation by the test strip would not interfere with the other examinations. One minute after instillation of a drop of 0.5% proparacaine, any visible fluid in the inferior fornix or lid margin was gently dried with a cotton swab. A precalibrated filter strip was then placed into the temporal inferior fornix and left in place for 5 min. The patient was allowed to either blink normally or to close the eyes. After 5 min, the strip was removed, and the amount of wetting (in millimetres) was recorded from the precalibrated strip.
For the diagnosis of an objectively diagnosed dry eye several definitions were used. Definition 1 was made if one of the following conditions was fulfilled: a tear-film break-up time ⩽10 s; a Schirmer test score ⩽5 mm; a fluorescein score ⩾1; telangiectasia at the lid margin; or if plugging of the gland orifices was present. Definition 2 was made if all parameters mentioned above were positive, that is, a tear-film break-up time ⩽10 s, a Schirmer test score ⩽5 mm, a fluorescein score ⩾1 telangiectasia at the lid margin, and plugging of the gland orifices. Definition 3 was made if the tear-film break-up time ⩽4 s or a Schirmer test score ⩽4 mm, or a fluorescein score ⩾2. Telangiectasia at the lid margin and plugging of the gland orifices were not considered for this definition. Definition 4 was made if the tear-film break-up time ⩽4 s and a Schirmer test score ⩽4 mm and a fluorescein score ⩾2. Definition 5 was made if the tear-film break-up time ⩽4 s or a Schirmer test score ⩽4 mm, without taking the fluorescein score into account, and the appearance of the lid margin and the meibomian glands. Definition 6 was made if the tear-film break-up time ⩽4 s and a Schirmer test score ⩽4 mm, again without taking the fluorescein score into account, and the appearance of the lid margin and the meibomian glands.
Statistical analysis was performed using a commercially available statistical software package (SPSS for Windows, version 15.0, SPSS, Chicago, IL, USA). χ2 tests were used to compare the proportions. Logistic regression was used to investigate the associations of the binary dependent variable ‘presence of dry eye’ with the continuous or categorical independent variables, such as age and gender. Confidence intervals were presented. The statistical analysis was performed on the basis of subjects and not of eyes. All P-values were two-sided and were considered statistically significant when the values were less than 0.05.
Results
Of the 4439 subjects participating in the Beijing Eye Study 2001, a random sample of 1957 (44. 1%) subjects (1112 (56.8%) women) was drawn to assess dry eye symptoms and their associations. The mean age was 56.5±9.3 years (median: 57 years; range: 40–84 years), and the mean refractive error was −0.34±2.29 D. The study group did not vary significantly from the total study population of the Beijing Eye Survey in age (56.5±9.3 years vs 56.0±10.7 years; P=0.14), gender (P=0.64), refractive error (P=0.59), rural vs urban region (P=0.06), family income (P=0.97), intraocular pressure (P=0.25), prevalence of glaucoma (P=0.10), and prevalence of age-related maculopathy (P=0.39).
Of the study population, 1546 (79.0%) subjects were asymptomatic defined as no symptoms of a dry eye at all or symptoms of dry eye felt only rarely or sometimes. Subjective symptoms of a dry eye felt often or at all times were present in 411 subjects (21.0%). In a univariate analysis, the symptomatic subjects compared with the asymptomatic subjects came significantly more often from the urban region, and more often were female than male subjects. Additionally, dry eye symptoms were associated with corneal astigmatism, low best-corrected visual acuity, undercorrection of refractive errors, degree of nuclear cataract, presence of diabetes mellitus, present or former smoker, and family income (Table 2). It was not associated with refractive error calculated as the mean spherical equivalent, degree of cortical cataract and subcapsular cataract, intraocular pressure, drinking of alcohol, the presence of glaucoma, age-related maculopathy, and arterial hypertension.
Performing a multivariate analysis, with subjectively dry eye as dependent variable, and age, gender, rural vs urban region, corneal astigmatism, best-corrected visual acuity, undercorrection, degree of nuclear cataract, presence of diabetes mellitus, present or former smoker, and family income as independent parameters showed that a dry eye was still significantly associated with age, female gender, urban region, low degree of nuclear cataract, and undercorrection of refractive error (Table 3).
The results of all performed tests, that is, the measurement of the tear-film break-up time, the assessment of the fluorescein staining of the cornea, the slit-lamp-based examination of a meibomian gland dysfunction, and Schirmer's test did not vary significantly between the subjectively dry eye group and the normal group (Table 2).
The prevalence of a subjectively diagnosed dry eye based on the symptoms as described the subjects was not significantly associated with the objective diagnosis of a dry eye based on the tests of ocular surface stability, tear production, and lid margin appearance; and using definitions 1, 2, 3, 4, 5, and 6 the prevalence of dry eye was 98.5±0.3% (mean±standard error), 6.1±0.5%, 97.6±3.3%, 1.5±0.3%, 36.9±1.1%, and 4.1±0.4%, respectively. The subjective diagnosis of dry eye by the study participants was not significantly associated with the objective diagnosis of dry eye using definition 1 (P=0.66), using definition 2 (P=0.26), using definition 3 (P=0.48), using definition 4 (P=0.83), using definition 5 (P=0.29), and using definition 6 (P=0.28).
Discussion
Dry eye represents a multifactorial, heterogeneous disorder of the preocular tear film, which can result in multiple ocular surface disease. The tear film and ocular surface form a complex and stable system that can lose its equilibrium through numerous disturbing factors.17 Reduction in quality of life is inevitable when symptoms of dry eye occur. These symptoms range from mild transient irritation to persistent dryness, burning, itchiness, redness, pain, ocular fatigue, and visual disturbance. In the United States alone, approximately 7–10 million Americans require artificial tear preparations, with consumers spending over $100 million per year.18 Reported prevalence of dry eye is diverse, with questionnaire-based surveys documenting rates ranging from 14.4 to 33% of the population sampled.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 19, 20, 21 Studies that also involve tests of tear function including Schirmer's test, tear break-up time, fluorescein staining, or rose Bengal staining for determination of dry eye have found generally lower prevalence rates.3, 21 Limitations in comparisons of studies in different populations include different age distribution of the population, definitions of dry eye, or methodology. Most studies of dry eye have been confined to developed nations and older populations, with resultant lack of ethnic diversity. Therefore, we aimed to report the prevalence of dry eye symptoms in mainland China and to identify the possible associated risk factors.
Dry eye symptoms were rather common in the present population-based sample of Chinese with an age of 40+ years and living in Greater Beijing. Of 1957 participants, 411 (21%) reported having a dry eye symptom. In a multivariate analysis, the dry eye symptoms were significantly associated with age, female gender, urban region, and undercorrection of refractive error (Table 3). The prevalence figures of dry eye symptoms as found in the present study are mostly in agreement with findings from other investigations on other ethnic groups. These figures range from 14 to 34%.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 19, 20, 21
The published data regarding the relation between dry eye and gender are partially inconsistent.22, 23 The study performed in Australia by McCarty et al3 indicated that women were more likely to report symptoms of dry eye (odds ratio: 1.85). The study performed in North America by Moss et al6 indicated that the age-adjusted prevalence in men was 11.4%, which was significantly lower than the 16.7% prevalence in women (P<0.001). The studies by both Bjerrum et al24 and Schein et al2 indicated no gender difference in the prevalence of dry eye. In clinical experience, menopausal and postmenopausal women both tend to have dry eye complaints. Lamberts et al25 demonstrated that the tear production decreased significantly in women aged 50–59 years. McCarty et al3 reported that women were significantly more likely to be diagnosed with dry eye by rose Bengal assessment in the 50- to 59-year and 60- to 69-year age groups, but not in the 40- to 49-year age group.
However, a poor correlation between dry eye symptoms and dry eye tests has been demonstrated in population-based studies by Schein and co-workers1 in the United States and McCarty et al3 in Australia. The heterogeneity of dry eye and the reporting bias of the participants are potential explanations suggested by the authors.1, 2, 3, 4, 5, 6, 7 Each dry eye test that is frequently performed in clinical practice seeks only to measure a specific disorder of dry eye. Consequently, a patient with normal Schirmer test results, which reflects normal aqueous tear secretion, may report dry eye symptoms resulting from meibomian gland disease. If the dry eye symptoms could also be categorized into subtypes (that is, symptoms of aqueous tear deficiency, symptoms of meibomian gland diseases, and symptoms of mucin anomalies), then more logical analyses of the correlations between symptoms and signs could be made.
Another explanation of the poor association between dry eye symptoms and signs is that the frequently used dry eye tests do not reliably reflect the tear-film conditions in the nonclinic-based general population and consequently have limited value as screening tests.
To clarify the correlation between dry eye symptoms and signs, analyses were performed on data gathered from the Shihpai Eye Study, a population-based survey of subjects ⩾65 years of age in Shihpai, Taipei, Taiwan.
Interestingly, the tests assessing the tear production and the condition of the corneal surface and meibomian glands in the lids were not significantly associated with the subjective assessment of a dry eye by the subjects themselves. It agrees with the results of previous studies. To cite an example, Schein et al2 observed no association between the presence of more frequent symptoms and a lower Schirmer result, regardless of whether the analysis was based on mean scores with a cut-off value of 5 or a cut-off value of 7. One of the major reasons for the low sensitivity and specificity of Schirmer's test to detect a dry eye syndrome may be the heterogeneity of the dry eye syndrome itself.
An interesting finding in the present investigation was dry eye syndrome was more commonly reported in the urban region than in the rural region. Future studies may address whether it may be because of air pollution in the city of Beijing compared with its surroundings. In addition, undercorrection of an existing refractive error was another significant factor associated with dry eye symptoms, a finding that has not been usually found in the preceding studies. It may imply for daily practice that, for patients with dry symptoms, an undercorrected refractive error should be ruled out.
In conclusion, the dry eye symptoms as evaluated subjectively in a questionnaire occurred in about 21% of the adult population in the Greater Beijing area, with associations to age, female gender, urban region, and undercorrection of a refractive error. Measurement of the tear-film break-up time, assessment of the corneal fluorescein staining, slit-lamp based examination of a meibomian gland dysfunction, and Schirmer's test were not significantly associated with dry eye symptoms.
References
Bandeen-Roche K, Munoz B, Tielsch JM, West SK, Schein OD . Self-reported assessment of dry eye in a population-based setting. Invest Ophthalmol Vis Sci 1997; 38: 2469–2475.
Schein OD, Munoz B, Tielsch JM, Bandeen-Roche K, West S . Prevalence of dry eye among the elderly. Am J Ophthalmol 1997; 124: 723–728.
McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR . The epidemiology of dry eye in Melbourne, Australia. Ophthalmology 1998; 105: 1114–1119.
Shimmura S, Shimazaki J, Tsubota K . Results of a population-based questionnaire on the symptoms and lifestyles associated with dry eye. Cornea 1999; 8: 408–411.
Schein OD, Hochberg MC, Munoz B, Tielsch JM, Bandeen-Roche K, provost T et al. Dry eye and dry mouth in the elderly: a population-based assessment. Arch Intern Med 1999; 159: 1359–1363.
Moss SE, Klein R, Klein BE . Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol 2000; 118: 1264–1268.
Lee AJ, Lee J, Saw SM, Gazzard G, Koh D, Widjaja D et al. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Br J Ophthalmol 2002; 86: 1347–1351.
Lin PY, Tsai SY, Cheng CY, Liu JH, Chou P, Hsu WM . Prevalence of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology 2003; 110: 1096–1101.
Chia EM, Mitchell P, Rochtchina E, Lee AJ, Maroun R, Wang JJ . Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Experiment Ophthalmol 2003; 31: 229–232.
Moss SE, Klein R, Klein BE . Incidence of dry eye in an older population. Arch Ophthalmol 2004; 122: 369–373.
Lin PY, Cheng CY, Hsu WM, Tsai SY, Lin MW, Liu JH et al. Association between symptoms and signs of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Invest Ophthalmol Vis Sci 2005; 46: 1593–1598.
Kaiserman I, Kaiserman N, Nakar S, Vinker S . Dry eye in diabetic patients. Am J Ophthalmol 2005; 139: 498–503.
Uchino M, Dogru M, Yagi Y, Goto E, Tomita M, Kon T et al. The features of dry eye disease in a Japanese elderly population. Optom Vis Sci 2006; 83: 797–802.
Sahai A, Malik P . Dry eye: prevalence and attributable risk factors in a hospital-based population. Indian J Ophthalmol 2005; 53: 87–91.
Xu L, Wang Y, Wang S, Wang Y, Jonas JB . High myopia and glaucoma susceptibility. The Beijing Eye Study. Ophthalmology 2007; 114: 216–220.
Xu L, Li Y, Wang S, Wang Y, Wang Y, Jonas JB . Characteristics of highly myopic eyes. The Beijing Eye Study. Ophthalmology 2007; 114: 121–126.
Brewitt H, Sistani F . Dry eye disease: the scale of the problem. Surv Ophthalmol 2001; 45 (Supp 2): S199–S202.
Lemp MA . Epidemiology and classification of dry eyes. In: Sullivan DA, et al (eds). Lacrimal gland, tear film and dry eye syndromes 2. Plenum Press New York, 1998, pp 791–803.
Caffrey BE, Richter D, Simpson T, Fonn D, Doughty M, Gordon K . The Canadian dry eye epidemiology study. In: Sullivan DA, Dartt DA, Meneray MA (eds). Lacrimal gland, tear film and dry eye syndromes 2. Plenum Press: New York, 1998, pp 805–806.
Shimmura S, Shimazaki J, Tsubota K . Results of a population-based questionnaire on the symptoms and lifestyles associated with dry eyes. Cornea 1999; 4: 408–411.
Hikichi T, Yoshida A, Fukui Y, Hamano T, Ri M, Araki K et al. Prevalence of dry eye in Japanese eye centers. Graefes Arch Clin Exp Ophthalmol 1995; 233: 555–558.
Chalmers RL, Begley CG, Edrington T, Caffery B, Nelson D, Snyder C et al. The agreement between self-assessment and clinician assessment of dry eye severity. Cornea 2005; 24: 804–810.
Hay EM, Thomas E, Pal B, Hajeer A, Chambers H, Silman AJ . Weak association between subjective symptoms or and objective testing for dry eyes and dry mouth: results from a population based study. Ann Rheum Dis 1998; 57: 20–24.
Bjerrum KB . Keratoconjunctivitis sicca and primary Sjogren's syndrome in a Danish population aged 30–60 years. Acta Ophthalmol 1997; 75: 281–286.
Lamberts DW, Foster CS, Perry HD . Schirmer test after topical anesthesia and the tear meniscus height in normal eyes. Arch Ophthalmol 1979; 97: 1082–1085.
Acknowledgements
This study was supported by the Beijing Natural Science Foundation.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jie, Y., Xu, L., Wu, Y. et al. Prevalence of dry eye among adult Chinese in the Beijing Eye Study. Eye 23, 688–693 (2009). https://doi.org/10.1038/sj.eye.6703101
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703101
Keywords
This article is cited by
-
Comparison of deep learning-assisted blinking analysis system and Lipiview interferometer in dry eye patients: a cross-sectional study
Eye and Vision (2024)
-
Higher incidence of meibomian gland dysfunction in postmenopausal women with primary acquired nasolacrimal duct obstruction
International Ophthalmology (2024)
-
Differential characteristics among asymptomatic and symptomatic meibomian gland dysfunction and those with dry eye
BMC Ophthalmology (2023)
-
Impacts of air pollution and meteorological conditions on dry eye disease among residents in a northeastern Chinese metropolis: a six-year crossover study in a cold region
Light: Science & Applications (2023)
-
Development and validation of a multiplex electrochemiluminescence immunoassay to evaluate dry eye disease in rat tear fluids
Scientific Reports (2023)