Abstract
Purpose
To verify whether scanning laser polarimeter with the new variable corneal compensation algorithm (GDx VCC) and scanning laser ophthalmoscopy (Heidelberg Retina Tomograph (HRT)) allow measuring retinal ganglion cell loss in patients with multiple sclerosis (MS).
Patients and methods
We enrolled 23 MS patients with a history of previous demyelinating monocular optic neuritis. Examination included visual evoked potentials (VEPs), scanning laser ophthalmoscopy, and scanning laser polarimeter. HRT was performed to assess optic nerve head (ONH) shape, while GDx VCC was used to evaluate the retinal nerve fibre layer thickness (RNFLt) around the ONH. Statistical analysis was performed comparing results obtained for each eye with the available normative database and with the unaffected fellow eye.
Results
When the affected eye group was compared to the fellow-eye group, a significant (P<0.05) difference was found for few GDx VCC parameters. In contrast, no significant correlation was observed between clinical assessment and imaging techniques when the normal database of HRT and GDx VCC was used. A significant association was observed between VEP latency and some GDx VCC parameters.
Conclusions
Our results suggested that scanning laser polarimetry could detect loss of ganglion cells following demyelinating optic neuritis, but further studies are needed.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is a chronic neurological disease characterized by an autoimmune attack to the myelin sheath leading to tissue damage, often involving the prechiasmatic visual pathways. Demyelination of the optic nerve leads frequently to ganglion cell loss and subsequent nerve atrophy.1
In the last years, many new instruments have been introduced to quantify retinal ganglion cells.2 In particular, in glaucoma disease, loss of ganglion cells is characterized by reduction of the retinal nerve fibre layer (RNFL) outside the optic nerve head (ONH) and by the enlargement of the optic cup.3, 4, 5, 6
By using a polarimeter such as the Nerve Fiber Analyzer GDx VCC (with the new variable corneal compensation algorithm) (Carl Zeiss Meditec Inc., Dublin, CA, USA), some authors have shown that RNFL decreases upon glaucomatous damage.7, 8, 9 In particular, scanning laser polarimetry, which has been shown to allow early detection of glaucoma, assesses the thickness of RNFL by measuring the phase shift or retardation occurring when polarized light passes through a birefringent structure such as RNFL. The total retardation observed is proportional to the thickness of RNFL.7, 8, 9 Others observed that confocal scanning laser ophthalmoscopy such as Heidelberg Retina Tomograph (HRT; Heidelberg Engineering, Heidelberg, Germany; software version 2.01) is able to detect an early glaucomatous change of the ONH, analysing the three-dimensional shape of the optic disc.10, 11
The aim of this study was to detect retinal ganglion cell loss in MS patients with a history of optic neuritis (ON) and to assess difference between ON affected and unaffected eyes by using HRT and GDx VCC.
Patients and methods
In this prospective cross-sectional study, we enrolled 23 MS patients upon informed consent. The research followed the tenets of the Declaration of Helsinki.
Patients were included if they had definite MS according to McDonalds12 criteria, a documented history of recent unilateral ON, and a clinical relative afferent pupillary defect was present in the eye with the ON history. ONH had to be ophthalmoscopically normal in the ON unaffected eyes. Best-corrected visual acuity was better than 20/50 in the ON-affected eyes and 20/20 in the unaffected eyes.
Exclusion criteria included visual acuity below 20/50 in both eyes, a history of ON in both eyes, and/or any other clinically relevant eye abnormality or the presence of any other optic neuropathy. Eighteen patients had a relapsing–remitting (RR) subtype of MS, while the remaining five had a secondary progressive subtype. All patients with RR subtype of MS were relapse free at the time of the investigation. No patient was taking steroids.
Each patient was subjected to visual evoked potential (VEP) recording, assessment of ONH by HRT and RNFL by GDx VCC. The electrophysiological data were interpreted without knowledge of the HRT and GDx findings, and vice versa.
Retinal nerve analyzer—GDx VCC
RNFL of each eye was analysed by GDx VCC software version 5.3.1, a confocal scanning laser polarimeter using a 780 nm polarized light source. The image analyzer allows ignoring retinal vessels when assessing RNFL.13, 14 Such technique is highly reproducible and has been fully described elsewhere.7, 8, 13, 14, 15, 16, 17, 18, 19
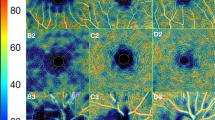
Briefly, a complete scan consisted of 128 pixels × 256 pixels. The field of view used by the system was 40 × 20°. Only good quality images determined by automatic software image quality assessment (better than 8) were selected for analysis. Upon data acquisition, a computer algorithm calculated the amount of retardation at each measured retinal position. A retardation map described the change in the state of polarization (retardation) at each location within the field of view. Each pixel represented the amount of retardation at a particular location. The GDx VCC compensates for corneal birefringence using a variable cornea compensator that allows compensation for each specific cornea individually.
The following GDx VCC parameters were considered: TSNIT average (mean average of the 360° RNFLT (TSNITAV)), superior average (SUPAV), inferior average (INFAV), TSNIT standard deviation (TSNITSD), nerve fibre indicator (NFI), symmetry (SYMM), superior ratio (SUPRAT), inferior ratio (INFRAT), superior/nasal ratio (SUPNAS), maximum modulation (MAXMOD), inferior modulation (INFMOD), ellipse modulation (ELLIPS), normalized superior area (NORSUPAR), and normalized inferior area (NORINFAR).
HRT
ONH was morphometrically evaluated by HRT. Details of this technique were previously published.20, 21, 22, 23, 24, 25 HRT is a confocal scanning diode laser with a wavelength of 670 nm. A series of 32 confocal images are obtained at consecutive focal planes, each 256 pixels × 256 pixels in size that the computer converts into a single topographic image. The depth of each topographic image series ranges between 0.5 and 4.0 mm in 0.5-mm increments, depending on individual differences in the optic disc morphology. For each eye, three 10° confocal scanning laser tomographic images were obtained. HRT mean standard deviation was 28.0±17.6 μm. Reproducibility and reliability of this technique have already been described in detail elsewhere.20, 21, 22, 23, 24, 25
We measured the following parameters: disc area (DA), rim area (RA), cup area (CA), cup/disc ratio (CD), cup volume (CV), rim volume (RV), mean cup depth (MEANC), maximum cup depth (MAXC), cup shape measure (CSM), high variation contour (HVC), mean retinal nerve fibre layer thickness (mRNFLt), retinal nerve fibre layer cross-section area (RNFLcsa), classification (class) and reference plane height (RH).
Visual evoked potential
For VEP recording, the eyes of MS patients were partitioned into two groups, depending on the presence (23 eyes) or absence (23 eyes) of history/signs of ON. The stimuli consisted of checkerboard patterns with a rectangular luminance profile presented in a counterphase mode, with a repetition frequency of 1 Hz (transient pattern VEPs). Two different fundamental spatial frequencies (SFs) of 1 and 4 cycles per degree (c.p.d.) were used. Stimuli were generated by a digital display generator driven by an IBM-compatible PC, and displayed on a monitor subtending 14° from 1 m viewing distance. The screen mean luminance was 80 cd/m2. The contrast of the patterns was 70%. VEPs were differentially recorded between an occipital and midfrontal electrode using gold cup electrodes placed on the scalp along the midline sites at Oz and Fz (international 10–20 system). The ground electrode was placed in the middle of the forehead. The interelectrode impedances were kept below 5 kΩ. Patients were asked to put their chin on a chin-rest and to refrain from blinking during the experimental sessions. A small cross in the centre of the screen was used as a fixation point. Each eye was tested separately, while the other eye was covered by a translucent patch to maintain light adaptation. Patients were tested by two trials, consisting of three separate 30-s runs, for each SF. The responses of each run were acquired in 1000-ms epochs and stored for off-line analysis. The signals were amplified 10,000 times and bandpass filtered (1–100 Hz). The sampling rate was 254 Hz. We evaluated, for each SF (1 and 4 c.p.d.) and each eye, the peak latency of the major positive component (P100). Mean values and SDs of the electrophysiological data were computed. Limits of normal values were obtained by adding 2.5 SD to the mean latency and amplitude values of our laboratory.26, 27
Statistical analysis
Both eyes of each patient were included in the study. The ON eyes were compared to the normal database of the instruments and to the unaffected fellow eye. All the data were analysed by a descriptive analysis. Student's t-test and Pearson's r correlation coefficient were used to compare the two sets of data when the distribution of the data was normal. Mann–Whitney test and Spearman's correlation coefficient were utilized to compare the two sets of data when they did not follow a normal distribution. The statistical power of the study ranged between 76.2 and 94.2% with an alpha of 0.05 and a beta of 0.5. Bonferroni correction was applied to Student's t-test because otherwise we would have a significant chance of 40.1% of our finding. For the comparison between imaging techniques, the kappa test was used.
Results
The mean age of the subjects included was 40.52±11.3 years (mean±SD) (range, 25–64 years) and the mean refractive error was −1.3±2.6 dioptres. There were 9 men and 15 women. The mean duration of the last ON attack was 7.2±7.1 months. The mean expanded disability status scale (EDSS) clinical score12 was 2.3±1.5 (range, 0–6). The first documented ON happened 6.2±5.9 years ago, and the diagnosis was carried out 9.7±7.1 years ago.
Reproducible transient VEPs were obtained from all the subjects, for both 1 and 4 c.p.d. stimulation patterns. Data (mean and SD) from the eyes of MS patients for each SF are shown in Table 1. VEP abnormalities were much more frequent (76% for 1 c.p.d. and 81% for 4 c.p.d. stimuli) in the eyes of patients with a history of ON than in those without a history of ON (44% for 1 c.p.d. and 55.5% for 4 c.p.d.). In the first group, 14 eyes out of 21 showed a delayed P100 to both SF, three eyes had a normal response to 1 c.p.d. stimulation, but a prolonged P100 to 4 c.p.d., and two eyes showed the opposite behaviour. In the second group, the most common abnormality was again a delayed P100 to both SF (11 eyes out of 27). Four eyes had normal responses to 1 c.p.d. stimulation but abnormal responses to 4 c.p.d., and only one eye showed a normal P100 latency to 4 c.p.d., in presence of a delayed 1 c.p.d. response. The combined use of P100 latency values for 1 and 4 c.p.d. stimuli allowed us to detect VEP abnormalities in 87% of the patients.
When the standard HRT and GDx VCC parameters were used to detect ON changes by using the normal database of the devices, HRT was able to detect ONH changes due to MS in 8 eyes of 23 patients, among these patients 3 had an ON and 5 not. GDx VCC was able to detect RNFL changes in 17 eyes of 23 patients, among these patients 8 had an ON and 9 not. Poor agreement among GDx VCC, HRT, and the history of ON was found. In particular, kappa was 0.155 (SE=0.22) between HRT and the history of ON, 0.195 (SE=0.209) between GDx VCC, and the history of ON and 0.201 (SE=0.208) between HRT and the GDx VCC.
When the HRT data obtained from the ON eyes were compared to the unaffected fellow eyes, a significant (P<0.05) reduction was found for mean RNFLt of HRT in the ON-affected eyes (Table 2), but when Bonferroni correction was applied, that difference was not significant anymore. Significant (P<0.05) changes were found for some GDx VCC parameters (TSNIT average and SD, superior and inferior average, nerve fibre indicator, superior and inferior max, normalized superior area, and normalized inferior area) (Table 3), but when Bonferroni correction was applied, only for two parameters (superior average and normalized superior area) the difference was significant. However, all the GDx VCC changes found showed a reduction of RNFL thickness in the ON-affected eyes.
We also analysed the eventual correlation between VEP and structure parameters and we found that when VEP increased, there was an RNFL reduction. In particular, the latency of P100 at 4 c.p.d. was significantly correlated with the HRT classification (r=−0.31; P=0.04). Some correlation was also found between GDx VCC parameters and VEP, P100 latency at 1 c.p.d. was significantly correlated with inferior average (r=−0.42; P=0.004) and TSNIT (r=−0.36; P=0.016) and NFI (r=0.28; P=0.05), while P100 latency at 4 c.p.d. was significantly correlated with superior/nasal ratio (r=0.32; P=0.03) and inferior average (r=−0.41, P=0.006).
No correlation was found between ON history and VEP and structural changes.
Discussion
The clinical application of HRT and GDx VCC has been clearly demonstrated in glaucoma, where RNFLt has been shown to correlate with visual field loss and could potentially be used as an indicator of early glaucomatous changes.10, 11, 18, 19
Hoyt et al28 first observed qualitative changes in RNFL of patients affected by glaucoma, later in 1974, Frisen and Hoyt noted that RNFL of MS patients was different from healthy subjects.29 In MS patients, RNFL abnormalities have been found in up to 80% of the cases by inspection of red-free retinal photographs.30, 31 Also, optic disc pallor detected by direct ophthalmoscopy or by slides has been described in up to 71% of eyes previously affected by ON.31, 32 However, clinical assessment using these techniques is somewhat subjective, prone to interobserver variability, and does not produce quantitative data.
A descriptive post-mortem studies of MS patients and in vivo magnetic resonance imaging studies found the presence of RNFL atrophy in association with optic nerve atrophy, although neither was measured quantitatively.33, 34, 35, 36
In a previous study, Parisi et al37 tried to measure the ONH changes in ON by means of Optical Coherence Tomography (OCT). The authors assessed axonal loss in RNFL after a single clinical episode of unilateral ON. In particular, 14 MS patients previously affected by ON demonstrated a significant reduction in RNFLt. A 46% reduction of total RNFL thickness in affected eyes compared with control eyes was observed, as well as a 28% reduction compared with the unaffected fellow eyes. RNFLt of the unaffected fellow eye was reduced by 26% relative to control eyes.37 Using OCT, Trip et al38 also showed a significant reduction of RNFLt in the affected eyes of MS patient compared with both controls and fellow eyes. Specifically, the authors found less reduction compared with control eyes but a similar reduction compared with unaffected fellow eyes. These results were obtained using the Stratus OCT Model 3000 and the minor level of reduction compared to control subjects could be due to the better accuracy of the Stratus OCT or to the differences in RNFLt in the control subjects. A nonsignificant reduction in unaffected eyes compared to control eyes was found in this study, which again was of lower magnitude than the findings of Parisi et al.37 In a recent study using HRT, Trip et al39 detected relevant changes in the amount of ganglion cells. In particular, they found significant difference between the ON eyes and the unaffected fellow eyes for RV and mRNFLt.
In this study, even if many parameters have been considered, among the HRT parameters, mRNFLt, which is able to assess RNFL height all around the ONH, was able to distinguish ON affected from unaffected eyes, while among the GDx VCC parameters the significant ones were those that more directly analysed RNFL thickness. These data suggested that both systems should be used to assess RNFL even if by using different methodology.
In addition, HRT and GDx VCC are two different confocal scanning techniques tailored to distinguish normal from glaucomatous eyes and were introduced to detect ganglion cell loss in glaucomatous disease. Both systems had difficulties to detect ON changes, probably because they used clinical formulae for glaucoma.40, 41 Indeed when we used the classification methods (the HRT FSM classification and the GDx VCC NFI), both systems had a bad performance, probably because these methods have been introduced for glaucoma and not MS clinic.
The poor agreement between VEP and devices could also be due to the presence of some subclinic demyelination, as VEP showed in Table 1. Indeed when there is a suspicion of ON in one eye, VEP is suggested to assess that optic nerve.27
These data could be explained by the presence of some patients with subclinical ON among the unaffected eyes. However, the presence of a relative afferent pupillary defect suggested the difference of the working fibres between the two eyes.
However, all the HRT parameters were not able to detect ONH changes due to MS, likely because MS patients can suffer from loss of ganglion cells but without creating a deep cup; astroglia cells can indeed occupy the damaged space. The HRT cup shape measure, which is the most sensitive parameter to distinguish normal from glaucomatous ONHs, did not show any difference between controls and both ON and unaffected eyes of MS patients. CSM indicated that the measurement was normal in both groups. Even when the HRT classification was used, the system did not show good diagnostic capacity.
The GDx VCC is a different technique, able to detect ganglion cell loss, because of change in the retardation time. The polarized light needs time to cross the microtubule of the ganglion cell and, when these cells die, the retardation time changes. The nerve fibre indicator did not have good diagnostic capacity as in glaucoma clinics and we found a poor agreement between techniques. However, few GDx parameters showed a good capacity to distinguish ON eyes and those without a history of ON. Thus, GDx VCC could be able to detect small differences also between the two eyes, one with a large amount of ganglion cell loss post-ON and the other one with some subclinical involvement of the optic disc, but with a smaller loss of ganglion cells.
Our study, using both HRT and GDx VCC, indicated that these imaging technologies could detect a different degree of RNFL loss between the eyes with ON and the unaffected fellow eyes, although they did not distinguish ON eyes from healthy control eyes, probably because of the parameters considered.
From these data, it was possible to presume that ON eyes compared to the unaffected fellow eyes could show some difference in ganglion cell loss, as well as VEP, suggested by the presence of significant correlation between VEP and structure parameters.
In MS population, scanning laser ophthalmoscopes, which is able to analyse the ONH three-dimensional shape and in particular the change of volume, were not able to detect change. On the other hand, GDx VCC, which assesses RNFL thickness by using the birefringency property of ganglion cell microtubule, was probably able to detect the loss of cell because of the loss of microtubuli.
Clinical assessment of RNFL is still too subjective, these non-invasive techniques that could specifically measure loss of optic nerve axons would help to clarify whether the magnetic resonance imaging measures of atrophy do reflect axonal loss. These new methods to quantify the loss of RNFL could be very useful in clinics, but further studies need to be carried out towards this direction.
References
Gartner S . Optic neuropathy in multiple sclerosis. Arch Ophthalmol 1953; 50: 718–726.
Iester M, Garway-Heath DF, Lemij H . Optic Nerve Head and Retinal Nerve Fiber Analysis. Dogma: Savona, 2005.
Airaksinen PJ, Drance SM, Douglas GR, Mawson DK . Diffuse and localized nerve fiber loss in glaucoma. Am J Ophthalmol 1984; 98: 566–571.
Airaksinen PJ, Drance SM, Douglas GR, Schulzer M, Wijsman K . Visual field and retinal nerve fiber layer comparisons in glaucoma. Arch Ophthalmol 1985; 103: 205–207.
Caprioli J, Miller JM . Measurements of retinal nerve fiber layer surface height in glaucoma. Ophthalmology 1989; 96: 633–641.
Iester M, Courtright P, Mikelberg FS . Retinal nerve fiber layer height in high-tension glaucoma and healthy eyes. J Glaucoma 1998; 7: 1–7.
Weinreb RN, Dreher AW, Coleman A, Quigley H, Shaw B, Reiter K . Histopathologic validation of four-ellipsometry measurements of retinal nerve fiber layer thickness. Arch Ophthalmol 1990; 108: 557–560.
Zhou Q, Weinreb RN . Individualized compensation for anterior segment birefringence during scanning laser polarimetry. Invest Ophthalmol Vis Sci 2002; 43: 2221–2228.
Tannenbaum DP, Hoffman D, Lemij HG, Garway-Heath DF, Greenfield DS, Caprioli J . Variable corneal compensation improves discrimination between normal and glaucomatous eyes with scanning laser polarimeter. Ophthalmology 2004; 111: 259–264.
Kamal DS, Viswanthan AC, Garway-Heath DF, Hitchings RA, Poinoosawmy D, Bunce C . Detection of optic disc change with the HRT before confirmed visual field change in ocular hypertensives converting to early glaucoma. Br J Ophthalmol 1999; 83: 290–294.
Chauhan BC, McCormick TA, Nicolela MT, LeBlanc RP . Optic disc and visual field changes in a prospective longitudinal study of patients with glaucoma. Arch Ophthalmol 2001; 119: 1492–1499.
McDonald WI, Composton A, Edan G, Goodkin D, Hartung HP, Lublin FD et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the Diagnosis of Multiple Sclerosis. Ann Neurol 2001; 50: 121–127.
Waldock A, Potts MJ, Sparrow JM, Karwatowski WSS . Clinical evaluation of scanning laser polarimetry: I intraoperator reproducibility and design of a blood vessel removal algorithm. Br J Ophthalmol 1998; 82: 252–259.
Waldock A, Potts MJ, Sparrow JM, Karwatowski WSS . Clinical evaluation of scanning laser polarimetry: II polar profile shape analysis. Br J Ophthalmol 1998; 82: 260–266.
Zangwill L, Berry CA, Garden VS, Weinreb RN . Reproducibility of retardation measurements with the Nerve Fiber Analyzer II. J Glaucoma 1997; 6:384–389.
Hoh ST, Ishikawa H, Greenfield DS, Liebmann JM, Chew SJ, Ritch R . Peripapillary nerve fiber layer thickness measurement reproducibility using scanning laser polarimetry. J Glaucoma 1998; 7: 12–15.
Weinreb RN, Shakiba S, Sample PA, Shahrokni S, Van Horn S, Garden VS et al. Association between quantitative nerve fiber layer of normal and glaucomatous eyes. Am J Ophthalmol 1995; 120: 732–738.
Weinreb RN, Shakiba S, Zangwill L . Scanning laser polarimetry to measure the nerve fiber layer of normal and glaucomatous eyes. Am J Ophthalmol 1995; 119: 627–636.
Tjon-Fo-Sang MJ, Lemij HG . The sensitivity and specificity of nerve fiber layer measurements in glaucoma as determined with scanning laser polarimetry. Am J Ophthalmol 1997; 123: 62–69.
Dreher AW, Tso PC, Weinreb RN . Reproducibility of topographic measurements of the normal and glaucomatous nerve head with the laser tomographic scanner. Am J Ophthalmol 1991; 111: 221–229.
Kruse FE, Burk RO, Völcker HE, Zinser G, Harbarth U . Reproducibility of topographic measurements of the optic nerve head with laser tomographic scanning. Ophthalmology 1989; 96: 1320–1324.
Cioffi GA, Robin AL, Eastman RD et al. Confocal laser scanning ophthalmoscope: reproducibility of optic nerve head topographic measurements with the confocal scanning laser ophthalmoscope. Ophthalmology 1993; 100: 57–62.
Weinreb RN, Lusky M, Bartsch DU, Morsman D . Effect of repetitive imaging on topographic measurements of the optic nerve head. Arch Ophthalmol 1993; 111: 636–638.
Mikelberg FS, Wijsman K, Schulzer M . Reproducibility of topographic parameters obtained with the Heidelberg Retina Tomograph. J Glaucoma 1993; 2: 101–103.
Chauhan BC, LeBlanc RP, McCormick TA, Rogers JB . Test–retest variability of topographic measurements with confocal scanning laser tomography in patients with glaucoma and control subjects. Am J Ophthalmol 1994; 118: 9–15.
Bandini F, Beronio A, Ghiglione E, Solaro C, Parodi RC, Mazzella L . The diagnostic value of vestibular evoked myogenic potentials in multiple sclerosis. J Neurol 2004; 251: 617–621.
American Clinical Neurophysiology Society. Guidelines 9A: guidelines on evoked potentials. 2006; 1–13.
Hoyt WF, Schlicke B, Eckelhoff RJ . Funduscopic appearance of a nerve fibre bundle defect. Br J Ophthalmol 1972; 56: 577–583.
Frisen L, Hoyt WF . Insidious atrophy of retinal nerve fibers in multiple sclerosis. Funduscopic identification in patients with and without visual complaints. Arch Ophthalmol 1974; 92: 91–97.
MacFadyen DJ, Drance SM, Douglas GR, Airaksinen PJ, Mawson DK, Paty DW . The retinal nerve fiber layer, neuroretinal rim area, and visual evoked potentials in MS. Neurology 1988; 38: 1353–1358.
Elbol P, Work K . Retinal nerve fiber layer in multiple sclerosis. Acta Ophthalmol (Copenh) 1990; 68: 481–486.
Trobe JD, Glaser JS, Cassady JC . Optic atrophy. Differential diagnosis by fundus observation alone. Arch Ophthalmol 1980; 98: 1040–1045.
Kerrison JB, Flynn T, Green WR . Retinal pathologic changes in multiple sclerosis. Retina 1994; 14: 445–451.
Gartner S . Optic neuropathy in multiple sclerosis. Arch Ophthalmol 1953; 50: 718–726.
Hickman SJ, Brex PA, Brierley CM, Silver NC, Barker GJ, Scolding NJ et al. Detection of optic nerve atrophy following a single episode of unilateral optic neuritis by MRI using a fat-saturated short-echo fast FLAIR sequence. Neuroradiology 2001; 43: 123–128.
Inglese M, Ghezzi A, Bianchi S, Gerevini S, Sormani MP, Martinelli V et al. Irreversible disability and tissue loss in multiple sclerosis: a conventional and magnetization transfer magnetic resonance imaging study of the optic nerves. Arch Neurol 2002; 59: 250–255.
Parisi V, Manni G, Spadaio M, Colacino G, Restuccia R, Marchi S et al. Correlation between morphological and functional retinal impairment in multiple sclerosis patients. Invest Ophthalmol Vis Sci 1999; 40: 2520–2527.
Trip SA, Schlottmann PG, Jones SJ, Altmann DR, Garway-Heath DF, Thompson AJ et al. Retinal nerve fiber layer axonal loss and visual dysfunction in optic neuritis. Ann Neurol 2005; 58: 383–391.
Trip SA, Schlottmann PG, Jones SJ, Garway-Heath DF, Thompson AJ, Plant GT et al. Quantification of optic nerve head topography in optic neuritis: a pilot study. Br J Ophthalmol 2006; 90: 1128–1131.
Iester M, Jonas JB, Mardin CY, Budde WM . Discriminant analysis models for early detection of glaucomatous optic disc changes. Br J Ophthalmol 2000; 84: 464–468.
Reus NJ, Lemij H . Diagnostic accuracy of the GDx VCC for glaucoma. Ophthalmology 2004; 111: 1860–1865.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors have proprietary interest in the development or marketing of any product or instrument mentioned in this article.
Rights and permissions
About this article
Cite this article
Iester, M., Cioli, F., Uccelli, A. et al. Retinal nerve fibre layer measurements and optic nerve head analysis in multiple sclerosis patients. Eye 23, 407–412 (2009). https://doi.org/10.1038/sj.eye.6703013
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703013
Keywords
This article is cited by
-
Altered birefringence of peripapillary retinal nerve fiber layer in multiple sclerosis measured by polarization sensitive optical coherence tomography
Eye and Vision (2018)
-
Retinal nerve fiber layer thickness changes following optic neuritis caused by multiple sclerosis
Japanese Journal of Ophthalmology (2011)
-
Retinal nerve fiber layer thickness in subgroups of multiple sclerosis, measured by optical coherence tomography and scanning laser polarimetry
Journal of Neurology (2010)
-
Assessing structure and function of the afferent visual pathway in multiple sclerosis and associated optic neuritis
Journal of Neurology (2009)