Abstract
Aim
To report on the agreement of macular hole size as measured using optical coherence tomography (OCT), Topcon digital photography, and surgeon estimate on clinical examination.
Methods
Observational cohort series of patients who underwent macular hole surgery over an 18-month period. Patients had OCT scan and digital fundus photographs preoperatively. At operation the surgeon estimated the size of macular hole. The agreement between methods was assessed using the technique described by Bland and Altman.
Results
There was good repeatability of photographic and OCT assessment and no evidence of systematic bias between repeated macular hole measurement by digital photography (P=0.36) or by OCT (P=0.58). There was evidence of systematic bias between photographic and surgeon measurements (P<0.001), and between OCT and surgeon (P<0.001) with photographic and OCT assessment being greater. There was also evidence of bias between OCT and photographic measurements with photographic measurement tending to be greater than the OCT measurement for smaller holes and lower for larger holes (P=0.02).
Conclusions
OCT and Topcon digital photography have good repeatability for measurement of macular hole size. Both these methods measured larger hole sizes compared to surgeon estimate. Digital photography and OCT methods did not agree.
Similar content being viewed by others
Introduction
Macular hole size is a prognostic indicator for both visual outcome and anatomical success of surgery.1, 2, 3 Various imaging modalities have been used to measure the size of macular holes, including optical coherence tomography (OCT),1, 2, 3 digital photography, and the confocal scanning laser ophthalmoscope.4 This study was undertaken to assess the repeatability of OCT and digital photographic analyses and to determine the agreement between these two methods and clinical assessment.
Materials and methods
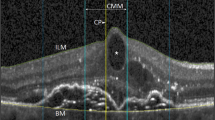
Patients were a cohort who underwent macular hole surgery over an 18-month period at Moorfields Eye Hospital. All patients underwent analysis by STRATUSOCT Model 3000 scanner (Zeiss Humphrey Instruments, Dublin, CA, USA) radial line OCT scan producing 6 × 6 mm scans, and digital fundus photographs taken with the Topcon TRC 50IA retinal camera (Topcon Corporation, Tokyo, Japan) the day prior to surgery. OCT scans were considered of good quality and used only if all six radial line images had a signal-to-noise ratio higher than 35 db, more than 95% of accepted A-scans and signal strength of 5 or more as recommended by the OCT scanner manufacturers.5 All six scans were examined by an ophthalmologist experienced in OCT interpretation. Macular hole size was measured using callipers in the ‘retinal thickness analysis’ mode (Figure 1), the scan with the largest distance between edges of the hole was taken to be the most accurate as this was more likely to represent the true diameter of the hole rather than an ‘off centre’ measurement. This is particularly relevant due the central scotoma and poor central fixation in many macular hole patients. From the chosen scan the shortest distance across the full-thickness defect was defined as the size of the hole as described in previous studies.2, 3
A photographic technician experienced in measuring images using Topcon IMAGEnet Digital Systems (Topcon, America Corporation, Paramus, NJ, USA) software system analysed one digital fundus photograph from each patient. If more than one photograph had been taken, the best image quality was assessed. Images were considered to be of good quality when the retinal nerve fibre layer was visualised. All images were 35° field size, two-dimensional (stereo images were not used), of 1024 pixels per inch resolution (ppi), and were viewed in colour mode. Both a horizontal and vertical diameter measurement was recorded for each photograph (Figure 2). The vertical and horizontal measurements were then averaged for each photograph resulting in a single diameter measurement per patient. The operating surgeon (of which there were four in total) was asked to estimate hole size in relation to the perceived size of the optic disc to the nearest 50 μm at operation using either the BIOM wide angle viewing system or the Machemer contact lens.
Assessment of agreement between the methods of measurement was performed using the Bland and Altman technique.6, 7 To assess repeatability, we performed repeat measurements of macular hole size by masked analysis of a second digital photograph and a second OCT for each patient. Repeat surgeon estimate was not performed as the surgeon could not be adequately masked to their previous estimate during surgery. All statistical analyses were conducted using STATA version 7 (College Station, TX, USA). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Results
Fifty patients were recruited of which three did not have digital photographs and 11 had no surgeon estimate of hole size. A further three patients did not have OCT scan. The median size of all macular holes measured by OCT was 512 μm and the range was 212–1073 μm. The median as measured by surgeon estimate was 400 μm (range 100–800) and the median as measured by digital photography was 578 (range 153.5–996).
Repeatability
There was no evidence of systematic bias between repeat macular hole measurement by digital photography (47 patients, P=0.36). or by OCT (47 patients, P=0.58). The 95% limits of agreement for photographic readings were from −36.99 to 32.31 and for OCT readings −121.66 to 112.22.
Comparison of assessments
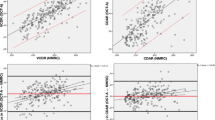
There was evidence of systematic bias between digital photography and surgeon macular hole measurements with photographic readings being almost always higher than the surgeon assessment (37 patients, mean difference (SE) 173.7 μm (29.00), P<0.001). Likewise, between OCT and surgeon (37 patients, mean difference (SE), 150.3 μm (29.57), P<0.001), OCT measurements were usually higher than surgeon estimate. The 95% limits of agreement for photographic and surgeon readings were from −179.0 to 526.4 μm and for OCT and surgeon readings −209.4 to 509.9 μm. Figure 3 illustrates that while photographic measurements tended to be higher than the corresponding OCT measurement for smaller holes the reverse was true for larger holes with the photographic measurement being lower than that of the OCT. Overall, there was evidence of systematic bias—with a mean (SE) difference of −61 μm (24.1) P=0.02. The 95% limits of agreement were wide ranging from −349.7 to 227.7 μm.
Agreement between OCT and Topcon digital photographic measurements. For smaller macular holes (to the left of the horizontal axis), there is a tendency for photographic measurements to be higher than the OCT measurements (observations tend to be above the horizontal line), whereas for larger holes the photographic measurements are lower than those of the OCT (observations are below this line).
Discussion
Accurate assessment of size of macular holes is important for both research studies and to guide clinical management, size of hole having been shown to affect anatomical and visual success.3, 8, 9 This study was undertaken to determine the extent of agreement between commonly used methods of macular hole size measurement (OCT, digital photography, and clinical examination) and the results show that while OCT and digital photography have good repeatability of results the two methods do not have a high level of agreement in their assessment of macular hole size. Since OCT and digital photography are intuitively less subjective than clinicians estimate, it might be expected that there would be closer agreement between these two methods than of either with surgeons estimate. OCT and digital photographic analysis are, however, not totally objective: in OCT the callipers must be placed by an observer, likewise the observer must choose where to start and end the measurement when using Topcon digital photography. Detailed study of individual pixels of digital images may allow more scientific and accurate measurement of hole size, however, would be both time consuming and impractical clinically. It is notable that the photographic measurement tended to result in larger hole size compared to OCT measurement for small macular holes, and conversely giving a smaller hole size compared to OCT for larger holes. It may be that patients with a larger macular hole and therefore larger central scotoma tracked the OCT scanning line, therefore resulting in a falsely elongated macular hole size measurement. Our results suggest that clinical examination underestimates macular hole size compared to OCT and digital photography. It is possible that clinical assessment may underestimate hole size because of reflected light from around the hole or due to glial tissue along the hole edges.10
The statistical assessment of agreement as described by Bland and Altman6, 7 was chosen as it is applied when direct measurement without adverse effects is difficult or impossible (in this instance direct measurement of the macular hole). As the true values remain unknown we are using indirect methods of measurement and these are assessed in pairs (ie, OCT, digital photography, and clinical examination). Bland and Altman6, 7 also stress the importance of repeatability in assessing agreement between methods, as a method with poor repeatability will never agree well with another method.6, 7 The ideal model for assessment of agreement as described would have involved the same observer taking the different measurements to avoid interobserver variability;6, 7 however, because of the skill and experience required by each of the three methods, the measurements in this study were performed by different individuals. Interobserver variability was also introduced by having different surgeons (total four) estimating the hole size at time of operation; however, we consider that this represents the ‘real-life’ situation encountered by vitreoretinal surgeons.
We performed repeatability tests for the OCT and digital photography, an essential step in assessment of agreement. It was not possible in the operative time frame for surgeons to repeat measurement by clinical examination while remaining masked to their previous result and we consequently do not have a repeatability analysis for this.
A number of variables were considered in planning measurement of hole size by each method. For example, the difficulty of fixation with a central scotoma may have prevented a true maximum diameter section through the hole being obtained with both the digital photographs and OCT. In an attempt to reduce this problem, the scans and photographs were either repeated until optimal fixation was obtained or for the OCT the external fixator light was used.
Refractive errors can affect magnification of absolute measurements, as surgeon estimate of macular hole size (although using two different viewing systems) was a relative measurement (relative to optic nerve size) this does not apply.11 No correction was made for different refractive errors in our methods of measurement (OCT or digital photography). Therefore, any bias introduced would have applied to all sets of measurements although possibly in unequal proportions. We limited surgeons to estimating hole size to the nearest 50 μm as we felt any smaller increment would be impractical in the clinical setting. We acknowledge, however, that limiting only this one method of measuring hole size could introduce bias. Using the Topcon photographic system, an infinite number of measurements can be taken and we concluded that averaging two was practical in a clinical setting. Furthermore, we selected the OCT scanning mode of ‘6 × 6 radial line’, providing six scans evenly spread at a 60° angle centred at the macula. This was considered a clinically practical compromise likely to incorporate the maximum hole diameter in one of the six scans. The ‘radial line’ scanning mode of the OCT while taking a few seconds longer than the ‘fast macula scan’ provides greater resolution of image (512 A-scans vs 128 A-scans),5 and was therefore chosen to determine more accurately the hole edges.
OCT and digital photography demonstrated good repeatability in the measurement of macular hole size although agreement was not found between the measurements obtained using OCT, photography, and clinical examination. Therefore, we would advise that caution should be exercised in comparing studies where two different methods of macular hole size measurement are used and in generalising the results when advising patients on their prognosis. To determine which indirect measurement modality is the most accurate, agreement would ideally be assessed against a direct measurement of hole size. Potentially, this could be performed using optical assessment at operation or on pathology specimens although both such approaches have inherent weaknesses because of optical aberrations and processing artefacts. In clinical practice, it is likely that either OCT or photography would be used to measure hole size and advise patients of their prognosis. As both methods are reliably repeatable they would appear to be equally valid (and better than clinical assessment) if individual units audit surgical results against hole size measurements. In addition, it may well be that there is no arbitrary cutoff hole size (eg, 400 μm) where the surgical prognosis significantly alters and that outcome varies directly with the continuum of hole size. The absolute measurement of the size of the macular hole in comparison to previous studies may therefore be only of secondary importance.
References
Ullrich S, Haritoglou C, Gass C, Schaumberger M, Ulbig MW, Kampik A . Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol 2002; 86: 390–393.
Ip MS, Baker BJ, Duker JS, Reichel E, Baumal CR, Gangnon R et al. Anatomical outcomes of surgery for idiopathic macular hole as determined by Optical Coherence Tomography. Arch Ophthalmol 2002; 120: 29–35.
Kang SW, Ahn K, Ham D-I . Types of macula hole closure and their clinical implications. Br J Ophthalmol 2003; 87: 1015–1019.
Kobayashi H, Kobayashi K . Correlation of quantitative three-dimensional measurements of macular hole size with visual acuity after vitrectomy. Graefes Arch Clin Exp Ophthalmol 1999; 4: 283–288.
Zeiss STRATUSOCT USER MANUAL P/N 55556 Rev A. 2004.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; i: 307–310.
Bland JM, Altman DG . Measuring agreement in method comparison studies. Stat Methods Med Res 1999; 8: 135–160.
Puliafito CA, Hee MR, Lin CP, Reichel E, Schuman JS, Duker JS et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology 1995; 102: 217–229.
Ryan EH, Gilbert HD . Results of surgical treatment of recent-onset full-thickness idiopathic macular holes. Arch Ophthalmol 1994; 112: 1545–1553.
Madreperla SA, Geiger GL, Funata M, de la Cruz Z, Green R . Clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade. Ophthalmology 1994; 101: 682–686.
Pach J, Pennell DO, Romano PE . Optic disc photogrammetry: magnification factors for eye position, centration and ametropias, refractive and axial; and their application in the diagnosis of optic nerve hypoplasia. Ann Ophthalmol 1989; 21: 454–462.
Acknowledgements
Grant information: Financial support provided by Pfizer, Tadworth, Surrey, grant no.: PARA-0505-084. The authors have no competing interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Benson, S., Schlottmann, P., Bunce, C. et al. Comparison of macular hole size measured by optical coherence tomography, digital photography, and clinical examination. Eye 22, 87–90 (2008). https://doi.org/10.1038/sj.eye.6702947
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702947
Keywords
This article is cited by
-
Assessment of OCT measurements as prognostic factors in myopic macular hole surgery without foveoschisis
Graefe's Archive for Clinical and Experimental Ophthalmology (2013)