Abstract
Purpose
To report our experience of using Aqualase technology for cataract extraction.
Methods
In total, 33 patients (20 females; mean age 71.4 years) underwent cataract surgery using Aqualase through a 3.2-mm corneal incision. Grade of nucleus, nuclear removal technique, and intraoperative complications were noted. Clinical parameters from postoperative visits were collected.
Results
Aqualase is capable of removing cataracts up to nuclear sclerosis 2+ (out of 4) with relative ease. Nuclei graded 2+ or greater were technically more difficult and conversion to ultrasound phacoemulsification was required in one case. Two posterior capsule ruptures occurred: one during nucleus removal (contact with the tip while aspirating without Aqualase) and one unrelated to Aqualase during aspiration of cortex. Of 25 patients seen on the first postoperative day, 22 had a clear cornea. A total of 96% patients without preoperative comorbidity achieved 6/9 or better postoperatively. One patient had transient postoperative uveitis.
Conclusions
Removal of softer cataracts with Aqualase has the theoretical advantage over phacoemulsification, by carrying less risk to the posterior capsule, since the handpiece has a smooth polymer tip that has no mechanical motion inside the eye. However, the tip should not be considered entirely capsule-friendly, as rupture is possible with the foot-pedal in position two (aspiration only). Although certain adjustments to the technique are required, the method is similar enough to phacoemulsification to ensure a brief learning curve. With increasingly firm cataracts, Aqualase becomes less effective and ultrasound phacoemulsification is still superior for such cases, in our experience.
Similar content being viewed by others
Introduction
With the development of small incision ultrasound phacoemulsification cataract surgery came significant improvements in clinical outcomes with better postoperative visual acuity, reduced incidence of high astigmatism, and faster visual rehabilitation when compared with extracapsular cataract extraction.1 Phacoemulsification, however, still carries a significant risk of posterior capsule rupture with vitreous loss, which engenders an eight-fold increased risk of endophthalmitis, a 10-fold increased risk of retinal detachment in the first three postoperative months and a four-fold risk of a final visual acuity of worse than 6/12.2 The rate of posterior capsular rupture depends on experience and although the National Cataract Surgery Survey in 1997–1998 showed a rate of 4%,3 this may be as high as 10% in the most junior trainees and lower than 1% in experienced surgeons.2, 4, 5 Other common postoperative complications after phacoemulsification include raised intraocular pressure, uveitis, and corneal oedema. Alternative small incision techniques for nuclear removal have been investigated, including lasers6 and most recently liquefaction using Aqualase,7 which is an option available on the Infiniti Vision System (Alcon Laboratories, Fort Worth, TX, USA).
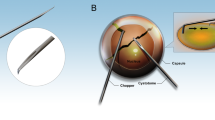
Aqualase employs pulses of warm balanced salt solution (57°C), which are propelled at up to a rate of 50 per second into the lens material, resulting in liquefaction, without the need for mechanical motion of the tip within the eye. The 4 μl pulses are generated by electrodes inside the reusable titanium handpiece and emerge from an orifice just inside the smooth polymer tip of the handpiece (Figure 1). These fluid pulses are deflected off the inside of the bevelled tip and are directed forwards from the main lumen, through which aspiration of liquefied fragments also occurs. Since the anterior chamber temperature is usually lower than body temperature during lens removal due to the high volume of cooler irrigation fluid flowing through the eye, the warm fluid pulses are not thought to raise the chamber temperature above physiological levels. Adjustable parameters in the Aqualase mode include the pulse rate, pulse magnitude and duty cycle (burst mode with intermittent fixed rate fluid pulses (on) punctuated by pauses (off)).
The proposed advantage of the Aqualase method for nuclear removal is a reduced risk of both posterior capsule rupture and thermal damage to the corneal wound when compared with phacoemulsification. We report here our experience of using Aqualase in 33 patients, with particular attention to intraoperative and postoperative complications, and final visual acuity.
Methods
In total, 33 consecutive patients undergoing Aqualase cataract extraction were included. Nuclear grade (sclerosis (ns) 0–4 according to LOCSII scoring system for opalescence),8 ocular comorbidity, and preoperative visual acuity were recorded and patients gave written informed consent prior to surgery. Following a 3.2-mm corneal stab incision and injection of viscoelastic, a continuous curvilinear capsulorrhexis and hydrodissection were performed before nuclear removal, using the Aqualase probe. Nuclear removal was followed by aspiration of cortical lens matter and lens implantation. Nuclear removal technique and intraoperative complications were noted. Clinical parameters from postoperative visits were collected, which included corneal clarity, anterior chamber inflammation (scored according to cellular activity 0–4+), intra-ocular pressure, and visual acuity (corrected by either autorefraction or pinhole). A clear cornea was defined as having the absence of descemet's folds, stromal haze, or overt stromal thickening. Central corneal thickness was not measured. A total of 25 patients were examined on the first postoperative day. All patients were seen within 1 month of surgery. An unpaired Student's t-test was used for statistical analysis and mean values are presented as ±standard error of the mean.
Results
Patient characteristics
Mean patient age was 71.4 years and 20 (60.6%) patients were female. Preoperative patient characteristics are detailed in Table 1.
Visual outcomes
Visual acuity was improved in 100% patients, and 22 of 23 (96%) patients without ocular comorbidity achieved a corrected visual acuity of 6/9 or better postoperatively (see Table 2). The remaining patient without comorbidity sustained the posterior capsule rupture during Aqualase and achieved 6/12 postoperatively from a preoperative acuity of 6/60. She had a clear cornea and normal retinal appearance postoperatively. Ocular comorbidity had a marked effect on visual outcome, with only three (33.3%) of these 10 patients achieving 6/9 and five (50%) having a final acuity worse than 6/18.
Complications
Intraoperative
Two posterior capsule ruptures occurred. One, unrelated to Aqualase, occurred during aspiration of cortical lens matter using bimanual irrigation and aspiration cannulae after nuclear removal. The second occurred during nuclear removal with the Aqualase probe. At the time of capsular breach, the tip made contact with the caspule with probe, aspirating without Aqualase. In this case, a small wick of vitreous prolapsed through the capsular defect and was cut by intraocular scissors. The lens implant was then placed in the capsular bag uneventfully, with no vitreous in the anterior chamber. Conversion to ultrasound phacoemulsification was necessary in one case with a relatively dense nucleus (ns3+) due to inability of the Aqualase to fragment the lens matter (see below). No other intraoperative complications occurred and in particular no thermal injury of the corneal wound was seen.
Postoperative
Of 25 patients reviewed on the first postoperative day, 22 had a completely clear cornea, with three having mild stromal haze, Descemet's membrane folds, and punctate epithelial staining, respectively. These three patients and those not seen on the first postoperative day had completely clear corneas by the next visit within 1 month of surgery. No intraocular pressure rises were noted. Only one patient developed significant postoperative anterior chamber inflammation, which was transient.
Nuclear removal
Adjustments to standard phacoemulsification methods for nuclear removal are required when using Aqualase. The smooth polymer tip is relatively ‘sticky’ when compared with phacoemulsification tips, so insertion requires the anterior wound lip to be held with forceps to apply counter-traction. When grooving, the end of the probe need not make direct contact with the lens material since liquefaction occurs in advance of the tip. A ‘divide and conquer’ technique with two grooves and ‘cracks’ perpendicular to each other can be achieved in a similar manner to phacoemulsification, but impaling a large nuclear fragment for a chop technique is more difficult with Aqualase, as the tip tends to shatter firmer nuclei, making vacuum building difficult. However, with slight adjustments, a chop technique is readily performed and eventually this ‘stop and chop’ method was felt to be the most efficient manner of nuclear removal. The Aqualase probe has excellent aspiration properties and, once the tip is occluded, is very effective at removing nuclear segments from the capsular bag for liquefaction in the anterior chamber. In addition, the aspiration of equatorial epinuclear material, often a treacherous moment during phacoemulsification, can be performed with more confidence, and the Aqualase pulses may be directed at a posterior capsular plaque for effective ‘polishing’.
One of the limitations of Aqualase is its inability to deal effectively with dense nuclei. We found that while the probe readily disrupts cataracts with nuclear sclerosis up to 2+, with increasingly firm cataracts Aqualase becomes less effective and ultrasound phacoemulsification is still superior for such cases, in our experience. Mean total number of Aqualase pulses per case was significantly higher in the ns2+ group (5522.9±717.5) compared with the ns1+ group (2499.0±250.5, P<0.001). In 30 of our patients, a subjective report was made by the surgeon after the procedure stating whether the procedure might have been easier with phacoemulsification. In eight of these cases (24.2%), it was adjudged that phacoemulsification might have been an easier method for dealing with that nucleus. Of these eight patients, seven were preoperatively assessed as having nuclear sclerosis 2+ or more. In the most dense nucleus attempted with Aqualase (ns3+), conversion to phacoemulsification was required due to an inability of the probe to fragment the lens material.
Discussion
Aqualase is a new method of nuclear removal during cataract surgery with some proposed advantages over ultrasound phacoemulsification, including reduced risk of posterior capsule rupture and thermal injury to the corneal wound. We have found Aqualase to be very effective for removal of soft to moderate density cataracts (up to nuclear sclerosis 2+), with a brief learning curve for those already proficient at phacoemulsification. Although no posterior capsular rupture occurred during active Aqualase pulsing, contrary to previous assertions, the smooth polymer tip is capable of rupturing the capsule when the vacuum causes occlusion of the tip by capsule, in a manner similar to capsule rupture with irrigation/aspiration cannulae during removal of cortical lens material. Therefore, although the warm water pulses may even be safely directed at the posterior capsule for the purpose of ‘polishing’, Aqualase should not be considered as an entirely ‘capsule-friendly’ technique. More extensive studies in time may demonstrate that Aqualase cataract extraction carries a reduced risk of capsule rupture when compared with phacoemulsification, and therefore have other advantages such as in the training of less experienced surgeons, but this was not the case in our study.
Surgical and visual acuity outcomes were good, and the high percentage of clear corneas on the first postoperative day would suggest that the procedure is well tolerated by the corneal endothelium. No published data are available pertaining to endothelial cell loss after Aqualase so it is unknown how the method compares in this regard to phacoemulsification, which is known to result in a significant detrimental effect,9 and we are in the process of studying this issue.
Thermal injury of the corneal incision site was not seen, but in view of the inability of Aqualase to effectively remove harder nuclei in which the risk of this complication during phacoemulsification is the greatest,10, 11 this benefit has questionable clinical relevance. We found that cases with nuclear sclerosis of 2+ were often felt to be more difficult with Aqualase than they would be with phacoemulsification, although this was entirely subjective. In our experience, those cases with greater than nuclear sclerosis of 2+ are best managed with phacoemulsification. It may be noted that the developments in Aqualase technology will allow more efficient removal of denser nuclei in the future but this remains to be seen, and for the present this aspect remains a significant limitation of Aqualase.
References
Minassian DC, Rosen P, Dart JK, Reidy A, Desai P, Sidhu M et al. Extracapsular cataract extraction compared with small incision surgery by phacoemulsification: a randomised trial. Br J Ophthalmol 2001; 85(7): 822–829.
Ionides A, Minassian D, Tuft S . Visual outcome following posterior capsule rupture during cataract surgery. Br J Ophthalmol 2001; 85(2): 222–224.
Desai P, Minassian DC, Reidy A . National cataract surgery survey 1997–8: a report of the results of the clinical outcomes. Br J Ophthalmol 1999; 83(12): 1336–1340.
Martin KR, Burton RL . The phacoemulsification learning curve: per-operative complications in the first 3000 cases of an experienced surgeon. Eye 2000; 14(Part 2): 190–195.
Tan JH, Karwatowski WS . Phacoemulsification cataract surgery and unplanned anterior vitrectomy—is it bad news? Eye 2002; 16(2): 117–120.
Fine IH, Packer M, Hoffman RS . New phacoemulsification technologies. J Cataract Refract Surg 2002; 28(6): 1054–1060.
Mackool RJ, Brint SF . AquaLase: a new technology for cataract extraction. Curr Opin Ophthalmol 2004; 15(1): 40–43.
Chylack Jr LT, Leske MC, McCarthy D, Khu P, Kashiwagi T, Sperduto R . Lens opacities classification system II (LOCS II). Arch Ophthalmol 1989; 107(7): 991–997.
Bourne RR, Minassian DC, Dart JK, Rosen P, Kaushal S, Wingate N . Effect of cataract surgery on the corneal endothelium: modern phacoemulsification compared with extracapsular cataract surgery. Ophthalmology 2004; 111(4): 679–685.
Sippel KC, Pineda Jr R . Phacoemulsification and thermal wound injury. Semin Ophthalmol 2002; 17(3–4): 102–109.
Bissen-Miyajima H, Shimmura S, Tsubota K . Thermal effect on corneal incisions with different phacoemulsification ultrasonic tips. J Cataract Refract Surg 1999; 25(1): 60–64.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary or financial interest in issues relating to this work
This work was presented in video format at the Annual Congress of the Royal College of Ophthalmologists, May 2005
Rights and permissions
About this article
Cite this article
Hughes, E., Mellington, F. & Whitefield, L. Aqualase for cataract extraction. Eye 21, 191–194 (2007). https://doi.org/10.1038/sj.eye.6702162
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702162