Abstract
Aim
To compare 6 months of treatment with bimatoprost and timolol in terms of their hypotensive efficacy and secondary effects, including changes in macular thickness and the inflammatory reaction induced in the anterior chamber.
Methods
A prospective, randomized, parallel-group trial performed on 30 eyes of 30 patients per group. The main outcome measure was the difference between the IOP value taken between the baseline visit and the 6-month-visit. Macular thickness determined through optical coherence tomography and anterior chamber inflammation estimated using the laser flare meter was also evaluated. Adverse events were recorded during the study period.
Results
Bimatoprost treatment gave rise to a significantly lower mean IOP than timolol in all follow-up visits as from the first month (P<0.05). Bimatoprost achieved high percentage IOP reductions from baseline in a significantly higher proportion of patients (P<0.05). Macular thickness and anterior chamber flare failed to vary significantly both between the two groups and within each group during the 6-month evaluation (P>0.05).
Conclusions
Bimatoprost 0.03% once daily showed a greater efficacy then timolol 0.05% twice daily in patients with elevated IOP. No significant differences were detected in macular thickness or anterior uveitis using optical coherence tomography and laser flare photometry.
Similar content being viewed by others
Introduction
Since the emergence in the 1990s of prostaglandin analogues there have been numerous case reports suggesting that these drugs could induce or reactivate inflammatory processes in the anterior chamber such as granulomatous uveitis,1 non granulomatous uveitis2 or even keratouveitis caused by herpes virus.3 The appearance of cystoid macular oedema has also been reported.4 However, there have been few prospective, randomized controlled clinical trials focusing on this issue and most published trials have evaluated the use of latanoprost.
Our study was designed to compare the hypotensive efficiency of topical 0.5% timolol maleate given twice daily with that of 0.03% bimatoprost taken once daily. We also evaluated the possible appearance of an inflammatory response in the anterior chamber, whether established or subclinical, through laser flare meter (LFM, Kowa FM-500, Japan) photometry and possible changes in macular thickness, including those undetectable on clinical examination, by Optical coherence tomography (OCT, Humphrey Zeiss Instruments, Dublin, CA, USA).
Materials and methods
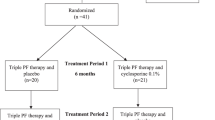
We designed a prospective, randomized, parallel 6-month trial performed on two treatment groups. The study protocol was approved by our institution's Ethics Committee and complied with the guidelines of the Declaration of Helsinki. Patients were recruited if they fulfilled the inclusion criteria: age over 18 years, primary open angle glaucoma, pseudoexfoliative glaucoma, pigmentary glaucoma, or ocular hypertension at least in one eye, capacity to follow the protocol's instructions, intraocular pressure (IOP) equal or greater than 22 mmHg at the time of enrolment and between 24 and 34 mmHg at the baseline visit after washing out previous glaucoma medication, and a visual acuity of 0.1 or better of the eye under study.
The exclusion criteria were: any anomaly impeding applanation tonometry, active infection or inflammation of the eye under study, history of allergy or systemic contraindication of any component of the drugs to be used, any macular or retinal pathology, diabetes, fertile women not using a reliable contraceptive method, a need for other chronic eye medication during the study, eye surgery during the 6 months prior to the study, laser treatment 3 months before the study, enrolment in another clinical trial during the 90 days preceding the baseline visit or severe visual field defects.
Participants were all the consecutive patients attending our clinic who fulfilled the inclusion criteria. All the patients approached gave their signed informed consent at the enrolment visit, and underwent a complete ophthalmologic exam including: visual acuity determination, gonioscopy, biomicroscopy, tonometry, funduscopy, and campimetry (using the Octopus program tG1, Interzeag AG., Switzerland). Patients fulfilling the inclusion/exclusion criteria were given an appointment for the baseline visit after having completed the appropriate washout period for their habitual glaucoma medication: 1 week for carbonic anhydrase inhibitors, 3 weeks for alpha-agonists, 4 weeks for beta-blockers, and 6 weeks for prostaglandins.
At the baseline visit, each patient was subjected to anterior flare determination using a laser flare meter, macular tomography using the OCT 3000 instrument and IOP measurement by applanation tonometry. Macular thickness was established using the ‘fast macular thickness’ procedure of the OCT.
Patients with an IOP between 24 and 34 mmHg determined at 0900, flare less than 10 photons/ms and normal macular thickness (<220 μm) were randomly assigned to one of the two treatment groups. One group of patients was treated with timolol maleate 0.5% twice daily (0900 and 2100) and the other with a single daily dose of bimatoprost (2100). Following the baseline visit, follow-up exams were conducted by an ophthalmologist blind to the treatment group at 2 weeks, and 1, 2, 3, and 6 months post-treatment.
Adverse events and specifically self-reported hyperaemia were recorded in an existing surveillance record (RD 561/1993).
The population size was calculated according to published reports of mean IOP reductions of 20–22.7% achieved with timolol and 30–32.4% with bimatoprost.5 According to our starting hypothesis of demonstrating a similar or greater IOP reduction at an alpha error or P≤0.05 in bilateral contrast with 90% power, 30 eyes were needed in each group.
For the statistical analyses, categorical variables were expressed as percentages and continuous variables as the mean, median, SD, minimum, maximum and number of observations. Categorical variables were compared by the χ2 or Fischer's exact tests. Continuous variables were compared by ANOVA for repeated measures or Manova test. The level of significance was set at P<0.05.
Results
Baseline mean IOPs were similar in the two treatment groups after the corresponding washout period (bimatoprost 24.1±3.2 mmHg, timolol 24.1±1.7 mmHg).
As from the first month, mean IOPs were significantly lower for the bimatoprost group in all follow-up visits (P≤0.004). After 6 months of treatment, mean IOP in the bimatoprost group was 13.5±3.1 mmHg and in the timolol group was 16.6±2.4 mmHg, the difference being statistically significant (P=0.003) (Figure 1).
The proportion of responders (an IOP drop ≥30% from baseline) in each follow up session was significantly greater in the bimatoprost group (Figure 2). Similarly, the proportion of patients reaching an IOP below 18 mmHg was higher in the group of patients treated with the prostaglandin (Figure 3).
No inter- or intra-group differences in macular thickness (P=0.790) were detected throughout the 6 months of follow-up (Table 1). Neither were any differences detected in anterior chamber flare (P=0.143) between or within groups during follow-up (Table 2).
No adverse events were registered in the timolol group throughout the study. In the group treated with bimatoprost, four patients developed hyperemia as from the second week of follow-up. This persisted mildly only in one of these patients in the 6-month follow-up visit. In two patients, eyelashes increased in number and thickness and darkened, both after the third month, and in a further patient there was hyperpigmentation of the skin around the eye after 6 months of treatment. No patient withdrew from the study on account of these secondary effects.
Discussion
The present results indicate that the hypotensive efficacy of 0.03% bimatoprost is greater than that shown by 0.5% timolol maleate, a finding consistent with most studies published to date. In a 2-year prospective study, Cohen et al6 noted a mean IOP decrease of 7.8 mmHg using bimatoprost and only a 4.6 mmHg reduction with timolol (P<0.001). The proportion of responders (IOP<18 mmHg) was also significantly greater in their bimatoprost group.
The present population size prevented us from detecting possible differences in macular thickness during follow-up between the two treatments. Since their launching on the market, prostaglandins have been linked to the development of cystoid macular oedema. However, it has not been possible to establish a direct causal relationship since most published reports include a limited number of cases.4, 7 Miyake et al8, 9 evaluated the incidence of macular oedema in patients treated with latanoprost, timolol maleate, and vehicles with and without preservatives following cataract surgery. Follow-up was performed for 5 weeks by fluorescein angiography. No cases of clinically significant macular oedema were detected in any of the groups. However, on fluorescein angiography similar dye leakage was noted in all the groups. This leakage had no repercussions on visual acuity and was related to the preservatives used in glaucoma drugs including both latanoprost and timolol. These authors proposed that the vehicles used could affect the blood–aqueous barrier. Furuichi et al10 used OCT to measure macular thickness in 68 patients with no risk factors for cystoid macular oedema under treatment with latanoprost. Over a 6-month period, these authors found no cases of macular oedema. Lima et al11 retrospectively evaluated 225 aphakic or pseudophakic patients treated with latanoprost, of whom 44% had a ruptured posterior capsule. Of these last patients, three underwent a drop in visual acuity of at least two Snellen lines, which was attributed to macular oedema. All three had had complicated surgery requiring anterior vitrectomy and one patient had already had a previous episode of macular oedema previous to glaucoma treatment.
We were unable to detect significant differences in our quantification of the inflammatory response induced in the anterior chamber based on flare photometry. Prostaglandin analogues have been linked to the induction and reactivation of inflammatory processes in the anterior segment.1, 12 However, most of the published data refer to isolated cases. In effect, it was not possible to demonstrate an enhanced inflammatory response in a prospective study performed on patients with glaucoma and high intraocular pressure treated with latanoprost.13 Moreover, in a controlled clinical trial, latanoprost applied four times daily for 2 weeks produced photophobia, moderate flare and a mild cell reaction in 15 of 28 healthy subjects with no predisposing risk factors.14 These authors noted a significant relationship between a latanoprost overdose and the onset of a moderate, often transient, inflammatory reaction. In a study comparing the efficacy and safety of bimatoprost vs timolol over 1 year, Cohen et al6 observed no differences between their treatment groups using laser photometry.
The appearance of several case reports in the literature could suggest a causal relationship between the use of prostaglandin analogues and clinically significant macular oedema or uveitis. However, no firm conclusions can be made concerning this relationship in the absence of adequately designed clinical trials to demonstrate differences related to the different treatments. Our results show that in patients with no risk factors, bimatoprost treatment could to be safe.
The main limitation of our study was the small population size. The number of patients, estimated for detecting differences in terms of hypotensive efficacy, was insufficient to draw conclusions on the effects of macular thickness and anterior chamber inflammation. Based on the trends observed, 2891 patients per group would be needed for the difference in macular thickness detected after 6 months of follow-up to reach significance with a statistical power of 90%. For anterior chamber inflammation, the population size would have to be 209 patients in each group. Notwithstanding, the differences in both variables observed between groups were minimal and even with a larger sample size, the clinical significance of the results would be questionable.
References
Parentin F . Granulomatous anterior uveitis associated with bimatoprost. A case report. Ocul Immunol Inflam 2003; 11: 67–71.
Smith SL, Pruitt CA, Sine CS, Hudgins AC, Stewart WC . Latanoprost 0.005% and anterior segment uveitis. Acta Ophthalmol Scand 1999; 77: 668–672.
Kroll DM, Schuman JS . Reactivation of herpes simplex virus keratitis after initiating bimatoprost treatment of glaucoma. Am J Ophthalmol 2003; 133: 401–403.
Wand M, Gaudio AR . Cystoid macular edema associated with ocular hypotensive lipids. Am J Ophthalmol 2002; 133: 403–405.
Higginbotham EJ, Schuman JS, Goldberg I, Gross RL, VanDenburgh AM, Chen K et al; Bimatoprost Study Groups 1 and 2. One-year, randomized study comparing bimatoprost and timolol in glaucoma and ocular hypertension. Arch Ophthalmol 2002; 120: 1286–1293.
Cohen JS, Gross RL, Cheetham JK, Vanderburgh AM, Berstein P, Whitcup SM . Two year double masked comparison of Bimatoprost with Timolol in glaucoma and ocular hypertension. Surv Ophthalmol 2004; 49: S45–S52.
Furuichi M, Chiba T, Abe K, Kogure S, Iijima H, Tsukahara S et al. Cystoid macular edema associated with the use of latanoprost in glaucomatous eyes with a normally functioning blood-ocular barrier. J Glaucoma 2001; 10: 233–236.
Miyake K, Ota I, Ibaraki N, Akura J, Ichihashi S, Shibuya Y et al. Enhanced disruption of the blood aqueous barrier and the incidence of angiographic cystoid macular edema by topical timolol and its preservative in early postoperative pseudophakia. Arch Ophthalmol 2001; 119: 387–394.
Miyake K, Ota I, Maekubo K, Ichihashi S, Miyake S . Latanoprost accelerates disruption of the blood aqueous barrier and the incidence of angiographic cystoid macular edema in early postoperative pseudophakia. Arch Ophthalmol 1999; 117: 34–40.
Furuichi M, Chiba T, Abe K, Kogure S, Iijima H, Tsukahara S et al. Cystoid macular edema associated with the use of Latanoprost. J Am Optom Asocc 1998; 69: 122–128.
Lima MC, Paranhos Jr A, Salim S, Honkanen R, Devgan L, Wand M et al. Visually significant cystoid macular edema in pseudophakic and aphakic patients with glaucoma receiving latanoprost. J Glaucoma 2000; 9: 317–321.
Smith SL, Pruitt CA, Sine CS, Hudgins AC, Stewart WC . Latanoprost 0.005% and anterior segment uveitis. Acta Ophthalmol Scand 1999; 77: 668–672.
Linden C, Nuija E, Alm A . Effects on IOP restoration and blood-aqueous barrier after long-term treatment with latanoprost in open angle glaucoma and ocular hypertension. Br J Ophthalmol 1997; 81: 370–372.
Linden C, Alm A . The effect on IOP of latanoprost once or four times daily. Br J Ophthalmol 2001; 85: 1163–1166.
Acknowledgements
This study was partly financed by the Instituto de Salud Carlos III, ‘Project C03/13: Clinical and basic research for the prevention of blindness’. The authors declare they have no commercial interests in any product, equipment or procedure mentioned in this article and that it has not been published elsewhere or submitted to another journal.
Author information
Authors and Affiliations
Corresponding author
Additional information
Section: Original clinical research article
Rights and permissions
About this article
Cite this article
Martin, E., Martinez-de-la-Casa, J., Garcia-Feijoo, J. et al. A 6-month assessment of bimatoprost 0.03% vs timolol maleate 0.5%: hypotensive efficacy, macular thickness and flare in ocular-hypertensive and glaucoma patients. Eye 21, 164–168 (2007). https://doi.org/10.1038/sj.eye.6702149
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702149
Keywords
This article is cited by
-
Long-term reduction of laser flare values after trabeculectomy but not after cyclodestructive procedures in uveitis patients
International Ophthalmology (2011)