Abstract
Purpose
To compare the accuracy of the potential acuity meter (PAM) and the illuminated near card (INC) in patients undergoing phacoemulsification.
Methods
During presurgical evaluations, both PAM and INC were tested on each study patient following dilation. Patients then rated the subjective ease of use of each test. Best spectacle-corrected visual acuity (BSCVA) was recorded at 4 and 12 weeks postoperatively. McNemar's χ2 test for paired associations was used to analyse categorical data; paired t-tests were used for continuous variables.
Results
Overall, the INC was more likely than the PAM to predict BSCVA within one Snellen line (P=0.002), but this difference decreased for accuracy within two lines. The PAM predicted BSCVA within one line in 87 (70.7%) eyes, as compared to 102 (82.9%) eyes by the INC. The PAM was accurate within two lines in 109 (88.6%) eyes; the INC was accurate in 115 (93.5%) eyes. The PAM was more likely to underpredict potential acuity (P<0.001), while the INC was more likely to overpredict (P=0.004) or give exact predictions of BSCVA (P<0.001). Accuracy of the INC declined in eyes with macular comorbidity. The PAM and INC were rated as ‘easy’ tests by 54 (45.4%) and 93 (78.2%) patients, respectively.
Conclusions
Both the PAM and the INC were useful for predicting BSCVA after phacoemulsification, but the PAM was more likely to underestimate potential acuity. The INC was easier for patients to use, and had better accuracy than the PAM in patients without macular comorbidity, but was more likely to overestimate potential acuity.
Similar content being viewed by others
Introduction
Many tools are available to measure potential acuity before cataract surgery, such as the potential acuity meter (PAM), the laser interferometer, the potential acuity pinhole, and others.1, 2 However, it is unknown what percentage of clinicians routinely evaluate cataract patients before surgery using a potential acuity device. A wider usage of potential acuity measurements may help surgeons give a more accurate estimate of postoperative acuity. This may decrease the number of patients disappointed with the results after surgery, or possibly decrease the number of surgeries performed without benefit to the patient. Alternatively, patients with macular disease who seem to have little hope for improved vision may in fact be candidates for cataract surgery based on potential acuity measurements.
The PAM, the most widely used potential acuity instrument, was developed in 1980 by Guyton and Minkowski.3 Mounted on a slit lamp, the PAM projects a point source of light approximately 0.1 mm in diameter into the patient's pupil. An image of a Snellen-type visual acuity chart is projected through the light source. Spherical refractive correction from −10.0 diopters to +15.0 diopters is possible by adjusting a knob that moves the visual acuity chart along the optical axis of an internal +12.0 diopter lens. In the original paper introducing the PAM, potential acuity was accurate within two Snellen lines in 77.3% of all eyes, and in 90% of eyes with preoperative acuities 20/200 or better.3 Subsequent studies have reported accuracy within two lines in all eyes ranging from 28 to 96%,2, 4, 5, 6, 7, 8, 9, 10 and in eyes 20/100 or better ranging from 45 to 96%.2, 5, 8, 9, 10
The illuminated near card (INC), first introduced in 1996,11 is a handheld device held 40.0 cm away from the patient. A fluorescent white light bulb is mounted behind a visual acuity chart with Sloan optotypes (Snellen-like letters) printed on transparent film. The lines of the chart are rotated by the examiner by turning a knob. The patient views the INC through a trial frame fitted with best distance correction, a +2.50 diopter lens, and a pinhole disc multiperforated with 1.0 mm pinholes. Thus far, the predictive value of the INC in cataract patients has only been evaluated in one study by Hofeldt and Weiss in 1998, who found a predictive accuracy within two lines in 91% of all patients, and 98% of patients with preoperative acuities of 20/100 or better.12
Our purpose was to evaluate the accuracy of the PAM and the INC, and compare their accuracies by performing both tests on a set of patients. Accuracy of these instruments in patients with macular disease was of special interest, and subgroup analyses were performed to determine if accuracy differed in these patients.
Methods
All patients in this prospective study were enrolled during the initial consultation preceding cataract surgery at Columbia Presbyterian Medical Center's Harkness Eye Institute between November, 2000 and September, 2002, and had phacoemulsification performed by one surgeon (REB). This study was approved by Columbia Presbyterian's Institutional Review Board (IRB). All patients with a Snellen preoperative best spectacle-corrected visual acuity (BSCVA) of 20/200 or better were available for enrollment when one of two study coordinators was present, and thus were nonconsecutive. Informed consent was obtained from each patient using an IRB-approved consent form before enrollment commenced.
Both PAM and INC tests were performed sequentially on each study patient in random order following dilation with 1% tropicamide. The patient was then asked to rate the ease of use of each test in the following categories: easy, slightly difficult, moderately difficult, and very difficult. Information was collected on a standardized data form. The age, sex, type, and grade of cataract, presence of macular comorbidity, and history of previous surgery were also recorded. Patients were categorized into groups according to the presence of macular comorbidity and history of previous surgery. Group 1 included patients with no macular pathology, while Group 2 included patients with macular pathology who had not undergone macular surgery as well as patients who had a history of macular pathology with subsequent macular surgery. The potential acuity tests were not used to determine need or benefit of cataract surgery.
Following cataract surgery, the patients' charts were reviewed to determine the Snellen BSCVA obtained at 1, 4, and 12 weeks after surgery. The best corrected visual acuity was recorded as the smallest Snellen line read without any mistakes. If the patient did not return for follow-up, the referring physician was contacted for their records. If 12-week follow-up was unavailable, information obtained at the 4-week-visit was used for analysis. Patients were excluded from the study if there was no follow-up available past 1 week, or if there was rapidly worsening macular degeneration or cystoid macular oedema postoperatively. Only one eye from each patient was included in the study in order to assure independence of all observations. In the event that phacoemulsification was performed on both eyes, the eye that was operated on first was included in the study.
Statistical methods
The McNemar's χ2 test and odds ratio for paired associations were used to compare the accuracy of the INC and PAM for categorical variables. These included the main outcome variable assessing whether the predicted potential acuity of each test was within 0, one, or two Snellen lines of the postoperative BSCVA. The underprediction and overprediction of potential acuity were also analysed. We converted Snellen acuities to LogMAR acuities, and determined the absolute difference between predicted and actual final best corrected visual acuities in terms of logMAR units (logMAR units of inaccuracy). The absolute values of these logMAR units obtained by the PAM and the INC were then compared using paired t-tests to compare the accuracy of the tests. Linear regression models were used to examine the relationships between the logMAR units of inaccuracy for each test and possible confounders such as age, sex, and preoperative visual acuity. Significance levels were set at two-tailed α=0.05. All statistical analyses were performed using STATA 6.0 (College Station, TX, USA).
A sample size calculation was performed, assuming α=0.05 and β=0.2. According to Hofeldt, the INC was accurate within two lines in 98% of eyes with pre-operative BSCVA of 20/100 or better.12 No other studies were available to provide additional data on the INC. Minkowski and Guyton's3 original paper found that the PAM was accurate within two lines in 90% of eyes with preoperative BSCVA of 20/200 or better. Other studies have found that the PAM accurately predicts postoperative acuity within two lines for 96,10 86,5 72,8 and 45%2 of eyes with preoperative BSCVA 20/100 or better, and 60%9 of eyes with preoperative BSCVA of 20/200 or better. A weighted average of these six figures gave an 80% accuracy rate to the PAM. We treated the PAM and INC tests performed on each patient as a pair, and defined discordant pairs as occurring when the two tests disagree, such as when one test is accurate within two lines, and the other is not. According to the numbers taken from the literature, the minimum number of paired tests or subjects needed to detect a difference between the accuracies of the PAM and the INC with 80% power and a two-tailed α of 0.05 is 41.
Results
Summary statistics
We enrolled a total of 143 patients in the study, of whom 12 did not return for surgery. A total of 131 patients underwent phacoemulsification, but of these, three were subsequently excluded due to postoperative cystoid macular oedema (1) or rapidly worsening macular degeneration (2), and five were excluded because no follow-up information was available after 1 week. The demographic data of the remaining 123 patients is shown in Table 1. These patients were divided into groups based on the presence or absence of macular pathology and history of macular surgery. There were 83 patients without macular pathology (Group 1). There were a total of 40 Group 2 patients: 14 of them had macular comorbidity without a history of macular surgery, while 26 patients had undergone surgery for their macular pathology (Table 2). Nuclear sclerosis was found in 110 (89.4%) patients. In all, 42 (34.1%) patients had cortical cataracts, while posterior subcapsular cataracts were found in 29 (23.6%).
Information for the 12-week follow-up BSCVA was available for all but six patients. At 12 weeks postoperatively, 109 of 117 (93.2%) patients improved to 20/40 or better. The PAM predicted that 109 (88.6%) patients would have a postoperative BSCVA of 20/40 or better, compared to 113 (91.9%) patients by the INC.
All subjects
Overall, the INC was more accurate than the PAM, with a smaller absolute number of logMAR units between predicted and actual logMAR acuities. For detailed statistics and numerical data, refer to Table 3. The INC was more likely than the PAM to predict the exact postoperative BSCVA (P=0.0001) and predict the BSCVA within one line (P=0.002). However, this difference between the PAM and the INC was not significant for prediction within two lines of BSCVA.
The PAM underpredicted acuity in 68 (55.3%) patients overpredicted the acuity of 18 (14.6%) and was exactly accurate in 37 (30.1%) patients. The INC underpredicted acuity in 31 (25.2%) patients, overpredicted in 28 (22.8%) patients, and made exact predictions of BSCVA in 64 (52.0%) patients. Overall, the PAM was more likely to underpredict acuity than the INC (P<0.00001), while the INC was more likely to overpredict acuity (P=0.004) or exactly predict the postoperative BSCVA (P=0.0001).
For both the INC and the PAM, there were no associations between age or sex and the number of LogMAR units differing between predicted and actual postoperative acuity. The LogMAR units of inaccuracy for the PAM were not related to preoperative LogMAR BSCVA (P=0.13). For the INC, there was a positive linear relationship between the preoperative LogMAR BSCVA and the number of LogMAR units of inaccuracy (P=0.001).
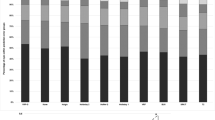
Subjective assessment of the ease of use of the tests was available for 119 patients (Figure 1). In all, 44 (45.4%) patients found the PAM to be an ‘easy’ test to take, 28 (23.5%) found it to be slightly difficult, 26 (21.8%) gave it a rating of ‘moderately difficult’, and 11 (9.2%) found the PAM to be ‘very difficult’. The INC was rated by 93 (78.2%) patients as ‘easy’, 23 (19.3%) found it ‘slightly difficult’, and three (2.5%) felt the INC was ‘moderately difficult’.
Stratified by group
We performed subgroup analysis of the data by stratifying the data based on the presence of macular pathology and/or macular surgery (Groups 1 and 2).
In Group 1 patients (no macular pathology), the accuracies of both the PAM and the INC were comparable to accuracies in the unstratified population (Table 3). We found that the accuracy of the INC declined in patients with macular comorbidity (Group 2) and that there were no significant differences in the accuracy of the instruments when used on these patients. Separate analysis of patients with macular pathology with and without previous macular surgery yielded similar results to combined analysis.
In Group 1 patients, the PAM was more likely to underestimate acuity (P<0.0001), while the INC was more likely to overestimate acuity (P=0.03), or give an exact prediction of BSCVA (P=0.0002). In Group 2 patients, the PAM was more likely to underestimate BSCVA (P=0.01) and the INC was more likely to overestimate acuity (P=0.05). However, the two tests were equally likely to give an exact prediction of visual acuity (P=0.21).
For both the PAM and the INC, there were no relationships between age and sex and number of lines of inaccuracy in either group. There was a positive linear relationship between the LogMAR units of inaccuracy of the INC and preoperative LogMAR BSCVA in Group 1 patients (P<0.001), but not in Group 2 patients (P=0.68). For the PAM, there was some association between LogMAR units of inaccuracy and preoperative LogMAR BSCVA in Group 1 (P=0.07), but not in Group 2 (P=0.83).
Patients with macular pathology did not find potential acuity tests to be more difficult than those patients without macular pathology. The percentages of each group who had difficulty with the PAM and the INC were not significantly different.
Discussion
Potential acuity testing before cataract surgery can be used to help the surgeon and the patient develop realistic expectations of results. We have previously reported that success of phacoemulsification in eyes with previous pars plana vitrectomy (PPV) is only limited by macular pathology.13 The use of a potential acuity device may thus be of greatest benefit in this group of patients.
It has been noted that potential acuity testing in patients with a preoperative BSCVA worse than 20/200 is inaccurate, and that underestimation of final postoperative BSCVA is common in these patients.3, 12 The degree of lens opacity present in these patients is the likely factor that limits potential acuity testing, especially when using methods that rely on a projection of a pinpoint light source such as the PAM and the INC. Thus, we chose to only include patients with a preoperative BSCVA of 20/200 or better in this study.
Our results indicate that both the PAM and the INC provide reasonable predictions of postoperative BSCVA, but the INC is more likely to give an exact prediction of postoperative BSCVA, and is more accurate than the PAM. The INC provided an exact prediction and prediction within one line in 52.0 and 82.9% of patients, respectively, vs 30.1 and 70.7%, respectively, by the PAM. While no longer statistically significant, the INC was still more accurate than PAM within two lines: 93.5% were predicted within two lines by the INC vs 88.6% by the PAM. Our accuracy rates for the INC and the PAM are similar, but slightly lower than the original accuracy rates found by Hofeldt12 and Minkowski.3
As expected, accuracy of both instruments was good in patients without macular comorbidity, but the INC was generally more accurate than the PAM. However, the accuracy of the INC decreased significantly in patients with macular comorbidity, from 0.06 LogMAR units in those without macular pathology to 0.10 LogMAR units in eyes with macular comorbidity. In contrast, the accuracy of the PAM did not change significantly (0.12 LogMAR units in those without macular pathology vs 0.11 LogMAR units in eyes with macular comorbidity). This is in contrast to Hofeldt's study, which found that the INC was more predictive in eyes with comorbid disease than in eyes without comorbid disease.12 Alio et al14 found that the PAM was less predictive in patients with age-related macular degeneration (ARMD) than in the overall study group. It is possible that the smaller size of our subgroup with macular comorbidity (n=40) or the particular types of macular disease in our study group may account for some of the difference in results. Caution should be exercised when using either instrument in patients with prior macular pathology, as the INC was more likely to overpredict potential acuity in these patients and the PAM was more likely to underpredict potential acuity.
The PAM and the INC underpredicted postoperative acuities by four Snellen lines in five patients and one patients, respectively. There were three patients who found the PAM to be a ‘very difficult’ test and had predicted acuities from the PAM that were worse than their preoperative BSCVA. There were no changes in our results or conclusions when these eyes were excluded from analysis. None of these three patients had macular pathology, extreme refractive errors, or major medical problems. One patient had 2−3+ nuclear sclerosis, another had a 1−2+ cortical cataract, and the third had a mixed nuclear sclerotic (2+) and cortical (2+) cataract. We tried to determine whether there were common factors in the remaining patients that made the tests more unreliable, but were unable to identify any similarities. In one patient, both the PAM and the INC underpredicted acuity by four lines. This patient had a mixed nuclear sclerotic (2–3+) and posterior subcapsular (3+) cataract, and did not have any history or evidence of macular disease, but had been complaining of decreased reading ability for the past 6 months. The other patient with poor prediction from the PAM had 3+ nuclear sclerosis, was status post-PPV for combined macular hole and pucker, and had a history of glaucoma.
For both tests, there was no relationship between the accuracy of the tests and age or sex. There appears to be a relationship between preoperative BSCVA and accuracy of both the PAM and the INC, but only in patients without macular disease. This is consistent with the expectation that the pinpoint charts of each test may be more easily projected through cataracts that are less opaque. In patients with macular disease, test inaccuracy may be due to macular pathology as well as the density of the cataract.
The differences in accuracy between the PAM and the INC are likely related to the difficulties of the two tests. During PAM testing, the examiner directs the point source of light into the patient's pupil. The patient may have to make minute head adjustments in order to find less opaque areas of the cataract. In contrast, patients using the INC may be able to see the eye chart through less opaque areas of the cataract by using larger head motions to find particular pinholes in the multiperforated disc that allow for optimum clarity. The PAM may thus be less accurate than the INC because patients are more dependent on the examiner to project the pinpoint chart through an optimal area of the cataract, and are less able to make such adjustments themselves. Subjectively, more patients found the PAM to be a more difficult test than the INC. Many patients complained of ‘grittiness’ when viewing the PAM eye chart and ‘jumping letters’. Patients with head movements or head instability also had more problems with the PAM, since it was difficult to keep the light source centred in the pupil. In addition, the PAM is able to correct for spherical refraction, but not for astigmatism, while the INC is able to correct for both spherical and astigmatic refractive errors.
Patients found that the INC was an easier test to use than the PAM. More than 75% of patients found the INC to be an ‘easy test’, while less than half thought the PAM was ‘easy’. Almost 10% of patients thought PAM was a ‘very difficult’ test, while none found the INC to be ‘very difficult’. While this subjective assessment certainly has its limitations, it provides a rough estimation of how tolerable this test is to patients.
Although this was a prospective study, certain limitations still exist. This study was conducted at a tertiary care centre, which may limit the generalizability of results. Refractions and assessments of visual acuity were made by different technicians working in different examination rooms. Although this may affect the overall accuracy of the data, there should not be any systematic bias that would favour one test over the other since each patient served as an internal control. It is possible that observer bias may be present, because the results of pre-operative PAM and INC testing were occasionally recorded in the chart. Thus, the technicians performing the postoperative BSCVA assessment were not blinded in this study. However, the study coordinators did not participate in postoperative BSCVA measurements, and recorded data by reviewing patient charts. Standard ETDRS charts were not routinely used in office examinations; thus, visual acuity was recorded in Snellen acuities, which are not as accurate, and may decrease the precision of our results. We did not quantitatively analyse the patients' subjective assessments of each test because we felt more reliable distinctions between categories were needed to give accurate results. A survey form with multiple, specific criteria would be useful to give consistent data for analysis. Ideally, a larger study sample, with more patients with macular disease, should be studied to give a more precise understanding of how accurately potential acuity may be predicted in these patients. A larger study sample may also clarify whether type of macular disease, or type of cataract affects the accuracy of potential acuity testing. We chose to analyse only one eye from each patient in order to assure the independence of each observation. This limited the number of eyes that we were able to enroll within the study recruitment period. In addition, there were five patients for whom we were unable to obtain a follow-up of more than 1 week, even after contacting their referring ophthalmologists. We chose to exclude these patients since a reasonable determination of BSCVA could not be made at the 1-week-visit.
In summary, both the PAM and the INC are reasonable predictors of potential acuity. The INC may be more accurate in patients without macular comorbidity, but may be more likely to overpredict than the PAM. The PAM is more likely to underpredict potential acuity, but may be a more difficult test for patients to use.
References
Minkowski JS, Guyton DL . New methods for predicting visual acuity after cataract surgery. Ophthalmic Technol 1984; 16: 512–516.
Melki SA, Safar A, Martin J, Ivanova A, Adi M . Potential acuity pinhole: a simple method to measure potential visual acuity in patients with cataracts, comparison to potential acuity meter. Ophthalmology 1999; 106: 1262–1267.
Minkowski JS, Palese M, Guyton DL . Potential acuity meter using a minute aerial pinhole aperture. Ophthalmology 1983; 90: 1360–1368.
Gus PI, Kwitko I, Roehe D, Kwitko S . Potential acuity meter accuracy in cataract patients. J Cataract Refract Surg 2000; 26: 1238–1241.
Severin TD, Severin SL . A clinical evaluation of the potential acuity meter in 210 cases. Ann Ophthalmol 1988; 20: 373–375.
Devereux CJ, Rando A, Wagstaff CM, Story IH . Potential acuity meter results in cataract patients. Clin Exp Ophthalmol 2000; 28: 414–418.
Graney MJ, Applegate MC, Miller ST, Elam JT, Freeman JM, Wood TO et al. A clinical index for predicting visual acuity after cataract surgery. Am J Ophthalmol 1988; 105: 460–465.
Cuzzani OE, Ellant JP, Young PW, Gimbel HV, Rydz M . Potential acuity meter vs scanning laser ophthalmoscope to predict visual acuity in cataract patients. J Cataract Refract Surg 1998; 24: 263–269.
Datiles MB, Edwards PA, Kaiser-Kupfer MI, McCain L, Podgor M . A comparative study between the PAM and the laser interferometer in cataracts. Graefe's Arch Clin Exp Ophthalmol 1987; 225: 457–460.
Ing MR . Potential acuity meter to predict postoperative visual acuity. J Cataract Refract Surg 1986; 12: 34–35.
Hofeldt AJ . Illuminated near card assessment of potential acuity. J Cataract Refract Surg 1996; 22: 367–371.
Hofeldt AJ, Weiss MJ . Illuminated near card assessment of potential acuity in eyes with cataract. Ophthalmology 1998; 105: 1531–1536.
Chang MA, Parides MK, Chang S, Braunstein RE . Outcome of phacoemulsification after pars plana vitrectomy. Ophthalmology 2002; 109: 948–954.
Alio JL, Artola A, Ruiz-Moreno JM, Ismail MM, Ayala MJ . Accuracy of the potential acuity meter in predicting the visual outcome in cases of cataract associated with macular degeneration. Eur J Ophthalmol 1993; 3: 189–192.
Author information
Authors and Affiliations
Corresponding author
Additional information
Meeting Presentation: Presented in part at the 2003 ARVO Annual Meeting, May 4, 2003, Ft. Lauderdale, Florida, USA (Poster Session)
Financial support: None
Proprietary interest: None
Rights and permissions
About this article
Cite this article
Chang, M., Airiani, S., Miele, D. et al. A comparison of the potential acuity meter (PAM) and the illuminated near card (INC) in patients undergoing phacoemulsification. Eye 20, 1345–1351 (2006). https://doi.org/10.1038/sj.eye.6702106
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702106