Abstract
Purpose
To study the incidence of acute postoperative presumed infectious endophthalmitis (PIE) in a UK district general hospital over a 10-year period. Consideration of such departmental healthcare-associated infection frequency rates as part of reflective and comparative quality practice in the light of local concerns.
Methods
Hospital-based retrospective case series: 12 831 cataract extraction operations from 01/01/1995 to 31/12/2004 were studied. All cases of PIE within 6 weeks of cataract surgery were ascertained and investigated in a standardised format. PIE incidence rate per 1000 cataract surgical procedures was contrasted with the existing literature.
Results
Seven isolated PIE cases occurred following phacoemulsification. None followed extra-capsular extractions. The PIE rate was 0.55 [95% CI; 0.22 to 1.12] cases per 1000 cataract extractions, or one PIE case within 6 weeks of surgery in every 1833 [95% CI; 893 to 4545] cataract operations undertaken. Five cases were culture positive. Details of PIE cases are presented.
Conclusion
PIE incidence rates in our department are slightly lower than reported case series in similar settings. Whether this is due to a variety of preventive measures deployed locally and/or methods of case ascertainment in published studies is problematic and is discussed. Departmental benchmarking data is important in relation to rare, but critical, patient safety incidents. Collection and monitoring of endophthalmitis outcomes is of merit and may inform patient choice. Surgical site infection surveillance systems of relevance are discussed. Implications for making healthcare safer, including reflective practice are, discussed in relation to cataract care.
Similar content being viewed by others
Introduction
Cataract surgery is the most commonly performed surgical procedure in the UK.1 Traditionally, clinical or performance outcome measures following cataract surgery focus on positive factors such as lines of vision gained or numbers treated, and waiting times. Analysis of error and failure, however, is seen as important for learning in high reliability organisations. Measuring the negative effects of clinical care can be justified on the grounds that such consideration may possibly detect root causes of problems or poor quality or practice, and further that negative impacts have significant indirect health economics and medico-legal implications as well as direct implications on both patients and staff.2 Taking preventative or corrective action should improve the net clinical benefit of the intervention to patients. Increasingly, the merit of analysis of systems is being recognised in healthcare as part of improving patient safety and enhancing quality.3
Infectious endophthalmitis or presumed infectious endophthalmitis (PIE) is the most devastating postoperative outcome for both cataract provider organisations and patients and is thus a priority topic. Most cases present acutely within the first week of cataract surgery and can be regarded, for practical purposes, as a healthcare-associated infection (HAI). While clinical outcomes are determined by the virulence of infecting microorganisms and timeliness and vigour of clinical treatment, prevention and surveillance of HAIs is increasingly recognised as paramount.4 The incidence of endophthalmitis after cataract surgery has dropped from approximately 10% in the late 1800s to 0.074% in the late 1980s.5 We wished to reflect on our local experience of PIE as a part of efforts to enhance patient safety and monitor HAI within local audit processes. The Royal College of Ophthalmologists recommends that postoperative endophthalmitis is a ‘critical incident’ that should be reported as part of clinical governance arrangements6 and further provides guidance on how outbreaks might be investigated.7 Furthermore, we had concerns about the disturbing incidence of three cases of PIE reported by a visiting overseas clinical team (OCT) deployed by neighbouring hospital management in 2002. (Unpublished data: Audit of ‘Operation Cataract’ at the Royal Lancaster Infirmary; presented by Netcare at the North Western Regional Ophthalmic Audit Meeting, University of Manchester, January 2003. Further details on request). We wished to have a local performance indicator for comparison with the observations of the visiting OCT.
Methods
Bolton is a former mill town in the northwest of England. The hospital serves a local population of approximately 261 000 residents, of whom 49% are male and 51% are female, 11% are nonwhite (mainly of South Asian origin), and 20% are aged over 60. Bolton has many areas of high social deprivation as indicated by a variety of deprivation indices.8, 9 Approximated social groups for the local census indicated that 80% of the local population are from low socioeconomic groups.9
The town is served by Bolton Hospitals National Health Service Trust, which has an Ophthalmology Department that provides the vast majority of elective cataract surgery for local residents as part of National Health Service (NHS) care. Cataract surgical patients are advised that should they develop any acute postoperative problems, to contact our department immediately. They will invariably be treated locally, in the first instance, in our department which maintained 24-h open patient access and examination by ophthalmic medical staff for urgent cases during the study period. There are no attendance costs to patients as services are provided within NHS provision. Endophthalmitis or PIE was diagnosed clinically by virtue of intention to treat patients presenting with acute symptoms. We reviewed all such patients presenting to our ophthalmic department over a 10-year period. We do not believe that local residents would either be inhibited from self-presenting or be referred elsewhere by their primary care physicians when suffering with acute postoperative problems shortly after surgery in our unit. It is unlikely that this study missed patients who developed endophthalmitis and moved or sought care elsewhere. Accordingly, we believe that all postoperative problems following cataract surgery, including patients with PIE, will present locally. A small number of local residents avail of private cataract surgery outside our unit. We do not believe this introduces any biases into this study, which is restricted to NHS care. The study reference period was the decade from 1 January 1995 to 31 December 2004, during which a total of 12 831 cataract operations were performed in our department. Patients with PIE within 6 weeks of surgery were ascertained using a combination of Hospital Episode Statistics returns for operation OPCS-4 Code C-71.2 for phacoemulsification, C71 for extra-capsular cataract surgery, C79.1 for anterior chamber tap, C79.2 for vitreous biopsy, C79.3 for vitreous injection, and additionally by hand searching of the surgical record register books and the operating theatre information technology system. (Theatreman, Healthcare Computer systems, Peterborough, Cambridge, UK). Of these cataract extractions 2467 were extra-capsular extractions in the earlier years and 10 364 were phacoemulsification procedures in later years, reflecting changing surgical practice. To validate PIE case ascertainment, we cross-checked pharmacy records for patients who had intravitreal antibiotics prepared in our pharmacy for PIE occurring within 6 weeks of cataract surgery during the study period. Further, we searched the microbiology database of all patients who had anterior chamber and vitreous tap samples sent for microbiological examination for PIE occurring within 6 weeks of cataract surgery. Furthermore all consultant ophthalmologists in the department were asked for details of any suspected PIE cases. Additionally, we also performed a word search for ‘endophthalmitis’ on all ophthalmic clinical correspondence word-processing software held in our department and checked local clinical governance ward records. All ascertained cases were then authenticated as having PIE within 6 weeks of cataract surgery performed in our institution only by examination of patient hospital records.
Patients who had PIE following operations other than cataract extractions, with or without intraocular lens implantation, were excluded. Patients with onset of PIE after 6 weeks of surgery were also excluded. Patients treated for PIE in our institution who had cataract surgery performed elsewhere were also excluded. Patient details were extracted from the hospital records in a standardised format. PIE incidence rates, differences in rates, and 95% confidence intervals (CI) were calculated using the software tool Stats Direct, version 2.3.7. (Stats Direct Ltd, Sale, Cheshire, UK) http://www.statsdirect.com.
Our cataract care includes systematic measures to reduce the risk of healthcare-associated infection. These barriers are embedded locally and were consistent for all staff working in the department during the study period. These include: examination at a preoperative nurse assessment clinic and again on the day of operation to rule out or treat any clinical suspicion of infection. If there is any suspicion of such infection, scheduled surgery is postponed (despite cancellations on the day of surgery being considered as ‘negative’ performance indicators). A single integrated care pathway for cataract surgery is deployed which includes: instillation of 5% aqueous povidone iodine in the anaesthetic room to irrigate the conjunctival fornices and again on the operating table; preoperative antisepsis of the eyelids and peri-orbital area with 10% aqueous povidone-iodine (except where iodine allergy was suspected, when chlorhexidine was used). Chloramphenicol 0.5% is instilled three or four times preoperatively on the day of surgery within the embedded protocol for pre-operative mydriatic drops. Our standard postoperative regime for all surgeons in the study period included sub-conjunctival injection of 125 mg cefradine and 2 mg betamethasone, along with postoperative topical 0.1% betamethasone and 0.5% neomycin eyedrops four times daily for 3 weeks between 1995 and 2001 (unless known allergies existed). In 2002, this was changed to 0.3% tobramycin and 0.1% dexamethasone postoperative eye drops with the same dosing regime and same sub-conjunctival antibiotics. Intra-cameral antibiotics or antibiotics in infused intraocular fluids were not used at any time. We adopt rigorous theatre procedures including hats and theatre-wear, thorough hand washing, minimise unnecessary theatre traffic and practice careful preparation and draping of the eye. Maximum use is made of disposable instruments and drapes and there is both vigilant immediate ultrasonic cleaning and on site sterilisation of any reusable surgical instruments. We are operational within a dedicated stand-alone ophthalmic surgical facility constructed 10 years ago. One of us was closely involved in the commissioning of this complex and an emphasis on facilities designed for safety and efficiency was embraced with the architectural and engineering consultants at that time. Laminar flow ventilation system is installed, which maintains approximately 25–30 air changes per hour. The air within the theatre space moves vertically downwards; thus, the possibility of introducing bacteria into the air stream by staff is reduced. No nonophthalmic surgery occurs in this theatre complex, thus reducing the risks of cross infections from other specialities. The patient day care/ward area was restricted to ophthalmology patients for most of the study period. Any potentially infected ophthalmic cases, such as cases of microbial keratitis, are nursed in a single room separate from the cataract patients. Clear corneal sutureless incisions have been used in latter years for most of the phaco-emulsification surgery undertaken in our department; however, incision techniques have varied. A variety of intraocular lens implant designs and materials were used during the study period.
A standard vitreous tap/inject protocol for management of PIE cases is followed locally, which involves aqueous and vitreous sampling and immediate inoculation onto enrichment media in the operating theatre followed by intra-vitreal injection of 1 mg vancomycin and 2.25 mg ceftazidime. Any growth of organisms was regarded as a positive culture result.
Results
Suspected post-operative PIE occurred in seven eyes of seven patients (Table 1 and 2). Two additional patients treated here, picked up by our various case ascertainment methods, who had their cataract surgery elsewhere, were excluded. PIE incidence was 0.55 cases (95% CI: 0.22–1.12) per 1000 cataract extractions or one case of PIE in every 1833 (95% CI: 893–4545) cataract operations undertaken. Five of the seven cases were positive on microbiological culture of both aqueous and vitreous samples. This is consistent with the culture-positive rates of 67% found in the Endophthalmitis Vitrectomy Study.10 Alpha haemolytic Streptococcus was the most common organism isolated (Table 2). All seven patients' eyes developed PIE after phacoemulsification of cataract; none followed extra-capsular extractions. One patient had intraoperative posterior capsular rupture requiring anterior vitrectomy and the implantation of an anterior chamber intraocular lens. The median time between cataract operation and endophthalmitis presentation/diagnosis was 6 days (range 2 to 19 days), with six of the seven patients presenting within the first postoperative week.
Discussion
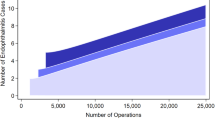
This study reports that one case of PIE occurred in every 1833 cataract operations undertaken at a district hospital in the northwest of England over the 10-year period up to the close of 2004. Considerable efforts have been applied to understand means to prevent postoperative endophthalmitis. Ciulla et al11 have provided a comprehensive analysis of peer-reviewed articles up to 2000 on the topic. Our PIE incidence of 0.55 (95% CI: 0.22 to 1.12) cases per 1000 cataract extractions within 6 weeks can be contrasted with the National Cataract Audit.12 This was a prospective UK multi-centre audit undertaken in unselected NHS units between September and December 1997, which reported 26 cases of endophthalmitis developing within 3 months of surgery amongst 15 787 patients for whom follow-up data was available, which is 1.65 PIE cases (95% CI: 1.08–2.41) per 1000 cataract extractions.12 PIE was also investigated in UK NHS care in a multi-centre surveillance study in 2000–2001 in reports to the British Ophthalmic Surveillance Unit (BOSU) and was recorded as 1.37 (95% CI:1.22–1.53) cases per 1000 cataract extractions within 6 weeks of surgery, which is approximately one case per 700 cataract extractions.13 Our PIE rates are thus comparable with and lower than both the National Cataract Audit and experiences reported to the BOSU investigators. Our results also compare favourably with another recent 10-year UK study where the PIE incidence was 1.65 (95% CI: 1.11–2.35) cases per 1000 cataract extractions (approximately one patient in every 600 operations) using a broadly similar study methodology in a similar single centre NHS setting.14 The report of three cases of endophthalmitis from the OCT deployed in the ‘Operation Cataract’ initiative involving 666 patients (922 eyes having phacoemulsification of cataract 7 having manual extra capsular extraction) or 3.23 (95% CI: 0.67 to 9.41) PIE cases per 1000 operations, in late 2002, at a neighbouring NHS hospital in the north west of England raised our concerns. (Unpublished data: Audit of ‘Operation Cataract’ at the Royal Lancaster Infirmary; presented by Netcare at the North Western Regional Ophthalmic Audit Meeting, University of Manchester, January 2003. Further details on request.) Reflection suggests that the higher rate encountered, in a similar healthcare and population setting, by the OCT, may be a cause requiring further deliberation. The Netcare visiting OCT reported three cases of PIE in 929 eyes undergoing cataract extraction in Lancaster. Seven cases were observed in 12 831 eyes undergoing cataract extraction in Bolton; this is a difference of 2.68 cases of PIE per 1000 operations (95% CI; 0.49 to 8.41), P=0.01. If the same rate of cataract surgery per patient treated in Bolton as in Lancaster is assumed, three cases of PIE were observed in 666 patients in the Lancaster Netcare initiative vs seven cases in 9199 Bolton patients; this is a difference of 3.74 PIE cases per 1000 patients treated (95% CI: 0.68 to 12.41), P=0.01. Both comparisons are clinically and statistically different. Further investigation of root causation is required so that any patient safety learning can be shared across healthcare organisations including the OCT concerned.2 An independent analysis is now awaited (The Healthcare Commission, 2004, unpublished personal communication).
Our results are also in line with prospective reporting studies such as the Norwegian national registry,15 where the PIE incidence was 1.56 cases per 1000 cataract extractions from 1996 to 1998, and the Swedish National Cataract Register, annual PIE incidence 1.06 cases per 1000 cataract extractions in 199816, 17 though case definitions of PIE vary somewhat. (Table 3 and 4). A recent study from Singapore18 using the same case definition as we did, reported an average annual PIE incidence of 0.76 (95% CI, 0.50 to 1.01) cases per 1000 cataract extractions within 6 weeks of cataract surgery, similar to our experience. The Endophthalmitis Population Study of Western Australia (EPSWA)19 reported a cumulative and stable endophthalmitis rate of 1.79 cases per 1000 cataract procedures over a 21-year study period. The EPSWA investigators provide a topical overview of published studies of endophthalmitis frequencies in their 2004 report.19 Strengths of our study include: standard operating procedures concerning endophthalmitis prophylaxis; robust case validation and thus likely accurate case ascertainment rates (numerator) from the surgical case load undertaken (denominator). We attribute the low PIE rate found to the range of systematic barriers described above, taken to reduce the potential risk of infection. It may be of interest to note that neither intra-cameral antibiotics nor antibiotics in infused intraocular fluids were used, as is in keeping with current UK cataract surgery practice.20 Conclusions should be drawn with some reservation, as our study, like most single centre studies, involves small numbers of PIE cases. We cannot be specific as to which infection prevention measure is paramount. Furthermore, it is problematic to study healthcare systems for relatively rare events such as endophthalmitis where there are a multitude of potential confounders, such as incision type, implant design and material, patient factors, chemo-prophylaxis regimes, hospital ward and theatre design, etc. The European Society of Cataract and Refractive Surgeons have thus recently instigated a prospective study of an anticipated 35 000 patients to consider possible risk factors and possible benefits of topical and intra-cameral antibiotics.
The variety of PIE reporting or surveillance methods, study designs of published case series and variable case definitions further complicates analysis (Table 3). Despite these epistemological limitations, certain features relevant to quality of patient care and service improvement are worthy of consideration. Reflection suggests that it is good practice for cataract surgical units to monitor their postoperative endophthalmitis frequencies in cultural benchmarking efforts. The ‘halo’ or Hawthorne effect may, however, be of relevance in quality improvement monitoring (ie a recognised effect in the direction expected but not for the reason expected; ie a significant positive effect that turns out to have no causal basis in the theoretical motivation for the intervention, but is apparently due to the effect on the participants of knowing themselves to be studied in connection with the outcomes measured).21 Postoperative endophthalmitis is not currently part of the surgical site infection (SSI) surveillance system recently proposed by the UK's Chief Medical Officer (CMO) even though, in our view, it fulfils several of the criteria described by the CMO within that policy document as requiring vigilant monitoring.4 Such SSI surveillance schemes have been shown to improve healthcare quality.22 There are no plans to extend the SSI scheme to cataract surgery at this time (personal communication, Sir Liam Donaldson, 2003).
If local PIE incidence rates are found to be higher than comparable departments, or from published studies, efforts should be made to investigate causation. A variety of measures and techniques have been suggested to attempt to prevent23 and investigate outbreaks of endophthalmitis.7 Many HAIs may be preventable.4 Patient safety incidents in England and Wales should be reported to the National Patient Safety Agency (NPSA). www.npsa.nhs.uk Clusters of rare events, such as PIE, might perhaps be detectable by the NPSA, or others, if the (voluntary) reporting by clinical staff of such events is accurate and timely. Under-reporting is a problem in voluntary reporting systems as was noted by both the BOSU endophthalmitis investigators11 and in surveys concerning PIE conducted in Germany24 and the Netherlands.25 Barriers to reporting patient safety incidents, especially by medical staff, are well recognised in healthcare.26 Optimal solutions for vigilance in endophthalmitis monitoring might be to collect data from all cataract surgeries in the UK within a register, which might then identify even a small inter-organisational or intra-departmental disparity of changes in endophthalmitis (or other indicator) frequencies that might not otherwise be evident either in conventional audit or in voluntary reporting systems. Systematic study of relatively rare outcomes, such as PIE, may require initiatives at national levels, as has been successfully undertaken in Norway13 and Sweden.14, 15 Similarly a National Joint Registry, a surveillance scheme for orthopaedic implants, has been recently initiated in England and Wales. www.njrcentre.org.uk We suggest that collection and monitoring of key performance indicators such as the incidence of PIE is of merit and might assist clinical teams in benchmarking their performance and in the identification of outliers or of clusters of infection. This might facilitate both best practice and further inform patient consent and is in line with current clinical governance and medico-legal policies.27, 28, 29, 30 Such information may also better inform patient choice, increasingly important given that central policy direction now encourages plurality of providers in UK cataract surgery.31 These suggestions may be pertinent with the more widespread deployment of OCTs into routine cataract care in England and where the current central focus on productivity32 is a concern to some.33
References
Department of Health. Hospital Episode Statistics (2002/03) NHS Hospitals in England. Department of Health: London, 2004.
Donaldson L . An Organization with a Memory. Report of an Expert Group on Learning from Adverse Events in NHS. Department of Health: London, 2000.
Reason JT . Human error: modes and management. BMJ 2000; 320: 768–770.
Chief Medical Officer. Winning Ways: Working Together to Reduce Healthcare Associated Infection in England. Department of Health: London, 200.
Kattan HM, Flynn HW, Pflugfelder SC, Robertson C, Forster RK . Nosocomial endophthalmitis survey. Current incidence of infection after intraocular surgery. Ophthalmology 1991; 98: 227–238.
The Royal College of Ophthalmologists. Critical Incidents in Ophthalmology, In: The Hospital Eye Service. The Royal College of Ophthalmologists: London, 2003.
The Royal College of Ophthalmologists. Investigating Outbreaks of Endophthalmitis. The Royal College of Ophthalmologists: London, 2004.
Office for National Statistics. Neighbourhood Statistics. Office for National Statistics: London, 2005. Accessed 23/02/2005.http://www.neighbourhood.statistics.gov.uk.
Bolton Metropolitan Council. Access Bolton: People in Bolton. Bolton Metropolitan Council: Bolton, 2003. Accessed 23/02/2005.http://www.bolton.gov.uk/pls/portal92/docs/7084.htm
Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study: a randomised trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 1995; 113: 1479–1496.
Ciulla TA, Starr MB, Maskett S . Bacterial endophthalmitis prophylaxis for cataract surgery: an evidence-based update. Ophthalmology 2002; 109: 13–26.
Desai P, Minassian DC, Reidy A . The National Cataract Survey 1997/1998: a report of the results of clinical outcomes. Br J Ophthalmol 1999; 83: 1336–1340.
Kamalarajah S, Silvestri G, Sharma N, Khan A, Foot B, Ling R et al. Surveillance of endophthalmitis following cataract surgery in the UK. Eye 2004; 18: 580–587.
Mayer E, Cadman D, Ewings P, Twomey JM, Gray RH, Claridge KG et al. A 10 year retrospective survey of cataract surgery and endophthalmitis in a single eye unit: injectable lenses lower the incidence of endophthalmitis. Br J Ophthalmol 2003; 87: 867–869.
Sandvig KU, Dannevig L . Postoperative endophthalmitis: establishment and results of a national registry. J Cataract Refract Surg 2003; 29: 1273–1280.
Lundstrom M, Stenevi U, Thorburn W . The Swedish National Cataract Register: a 9-year review. Acta Ophthalmol Scand 2002; 80: 248–257.
Montan P, Lundström M, Stenevi U, Thorburn W . Endophthalmitis following cataract surgery in Sweden. The 1998 national prospective survey. Acta Ophthalmol Scand 2002; 80: 258–261.
Wong TY, Chee SP . The epidemiology of acute endophthalmitis after cataract surgery in an Asian population. Ophthalmology 2004; 111: 699–705.
Li J, Morlet N, Ng JQ, Semmens JB, Knuiman MW, Team EPSWA . Significant non-surgical risk factors for endophthalmitis after cataract surgery: EPSWA Fourth ReportInvest. Ophthalmol Vis Sci 2004; 45: 1321–1328.
Gupta MS, McKee HDR, Stewart OG . Peri-operative prophylaxis for cataract surgery, survey of ophthalmologists in the north of England. J Cataract Refractive Surg 2004; 30: 2021–2022.
Mayo E . The human problems of an industrial civilization. MacMillan: New York, 1933.
Geubbels EL, Bakker HG, Houtman P, van Noort-Klaassen MA, Pelk MS, Sassen TM et al. Promoting quality through surveillance of surgical site infections: five prevention success stories. Am J Infect Control 2004; 32: 424–430.
Olson RJ . Reducing the Risk of Postoperative Endophthalmitis. Surv Ophthalmol 2004; 49(Suppl 2): S55–S61.
Schmitz S, Dick HB, Krummenauer F, Pfeiffer N . Endophthalmitis in cataract surgery: results of a German survey. Ophthalmology 1999; 106: 1869–1877.
Versteegh MF, Van Rij G . Incidence of endophthalmitis after cataract surgery in the Netherlands: several surgical techniques compared. Doc Ophthalmol 2000; 100: 1–6.
Lawton R, Parker D . Barriers to incident reporting in a healthcare system. Qual Saf Health Care 2002; 11: 15–18.
Department of Health. Reference Guide to Consent for Examination or Treatment. Department of Health: London, 2001.
Department of Health. Building a safer NHS for Patients. Department of Health: London, 2001.
Department of Health. An Organisation with a Memory. The Stationary Office: London, 2000.
Department of Health. Good Practice in Consent Implementation Guide: Consent to Examination or Treatment. Department of Health: London, 2001.
Department of Health. Choose & Book—Patient's Choice of Hospital and Booked Appointment. Department of Health: London, 2004.
Department of Health. Treatment Centres: Delivering Faster, Quality Care and Choice for NHS Patients. Department of Health: London, 2005.
Royal College of Ophthalmologists. Response to the Department of Health's press release and publication on Treatment Centres. The Royal College of Ophthalmologists: London, 2005. http://www.rcophth.ac.uk/about/press.html
Jensen MK, Fiscella RG, Crandall AS, Moshirfar M, Mooney B, Wallin T et al. A retrospective study of endophthalmitis rates comparing quinolone antibiotics. Am J Ophthalmol 2005; 139: 141–148.
Acknowledgements
We thank colleagues who encouraged us in this work. Credit for local post-operative results is due to the teamwork of clinicians and managers at Bolton Hospitals NHS Trust. We wish to thank Professor Brian Duerden for helpful comments on our manuscript.
Author information
Authors and Affiliations
Additional information
Poster presented at the Annual Congress of the Royal College of Ophthalmologists in May 2005. No competing interests.
Rights and permissions
About this article
Cite this article
Kelly, S., Mathews, D., Mathews, J. et al. Reflective consideration of postoperative endophthalmitis as a quality marker. Eye 21, 1419–1426 (2007). https://doi.org/10.1038/sj.eye.6701996
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701996