Abstract
Objectives
To report central corneal thickness (CCT) measurements on patients requesting refractive surgery and to search for possible associations between CCT and patient's origin, age, sex, and preoperative data.
Setting
Department of Ophthalmology, Soroka University Medical Center, and Enaim Refractive Center, Beer-Sheva, Israel.
Methods
Subjects were patients undergoing preoperative examination at our refractive centre during 2003. Patient's age, sex, preoperative CCT, refractive status, keratometry, and intraocular pressure (IOP) were obtained together with country of origin of the patients and their parents. Main outcome measures were CCT measurements and relationship between CCT and patient's origin and preoperative data.
Results
A total of 204 patients were included in the study. Patients of North African origin had statistically significantly thinner corneas than patients of other origins (518.9±31.5 vs. 545.4±30.4 μm in the right eye and 518.4±32.1 vs. 546.3±29.7 μm in the left eye; P<0.00001). Patients of North African origin were significantly older than patients of other origins (P=0.028). No differences were found when comparing for sex, intraocular pressure, refractive status, and keratometry. When multivariate analysis was performed patient's origin was the only independently associated factor associated with CCT.
Conclusions
This is the first work in reporting lower CCT in people of North African origin examined in a refractive surgery centre. Studies from similar populations are needed to confirm our results.
Similar content being viewed by others
Main
Central corneal thickness (CCT) measurements have been reported in several races, ethnic groups, and countries: Whites,1, 2, 3, 4, 5 African-Americans,2, 3, 4 Blacks,5 Latinos,4, 6 Greenland Eskimos,7 Asians4 (Hong-Kong,8, 9, 10 Chinese,11 Korean,12 Japanese,13 Singapore,14 and Mongolian,15), in Switzerland,16 Germany,17, 18 Spain,19 Denmark,20, 21 Holland,22 Turkey,23 Israel,24 Canada,25 New Zealand,26 India,27, 28 and Rwanda.29 According to Doughty and Zaman,30 who reviewed and performed a meta-analysis of more than 300 articles, if we consider that the normal cornea averages 536±0.031 μm, CCT was found to be significantly thinner (mean CCT values of less than 530 μm) in African-American, Mongolian, and Indian patients than in Caucasian, Asian, Hispanic, or European patients. To the best of our knowledge, CCT measurements have not been reported in African patients other than African-Americans living in the United States or Canada.
In recent years, importance has been attributed to CCT measurement in the screening, diagnosis, and management of ocular hypertension and glaucoma patients.31, 32 Similarly, with the development of refractive surgery procedures, CCT values are of enormous importance during the preoperative evaluation of the patients, the decision whether or not to perform surgery, the type of recommended procedure, and rate of postoperative complications.33, 34
Mixed populations are ideal for comparing CCT measurements in different ethnic groups under the supervision of the same investigators and the use of the same pachymeters. With people immigrating to Israel from almost all countries around the world, Israel demography provides an excellent opportunity to evaluate CCT in populations of different origin, including North Africa.
For this reason, people requesting refractive surgery in Israel constitute an ideal population for examining CCT measurements and for examining the relationship between CCT and patient's origin and preoperative data. It also allows describing CCT measurements in people from North African origin.
The present study was performed to report CCT for patients examined in a refractive surgery centre, and to search for possible associations between CCT and patient origin, age, sex, refractive status, keratometry, and intraocular pressure (IOP).
Methods
Patients included in this report were examined during 2003 in the Refractive Clinic at Soroka University Medical Center, in Beer-Sheva, Israel. The study included consecutive new patients presenting for refractive surgery. All data in this study are limited to the preoperative examinations, and were collected retrospectively. All patients were seen in year 2003.
The following data were collected from the preoperative examination: personal details, age, sex, manifest and cycloplegic refractions, automated keratometry, corneal topography (EyeSys® Vision, Houston, TX, USA), Goldmann applanation tonometry and CCT from both eyes. CCT was measured with an ultrasound pachymeter (Nidek US-1800). After applying a drop of benoxinate hydrochloride 0.4% for local anaesthesia, the pachymeter tip was placed perpendicular to the central cornea. A minimum of nine measurements were taken and the average reading was recorded. All measurements were performed by two of us (JL, TL) between 0400 and 0700. IOP was measured before the pachymetry measurement.
Patients were asked for their place of birth and that of their parents. Seven geographical zones were defined: (1) America, (2) Western and Central Europe, (3) Eastern Europe and Russia, (4) Asia, (5) North-Africa (ie Morocco, Algeria, Tunisia, Libya, and Egypt), (6) Israel, and (7) mixed origin, which included patients whose father and mother were born in different geographical zones. When both parents were born in the same country, patient's origin was recorded in one of the first six groups.
Inclusion criteria for this study were adults 18 years of age or older, no previous ocular surgery, and no contact lens use for 2 weeks before preoperative examination in the case of soft lenses or 4 weeks in the case of gas-permeable and hard lenses. Exclusion criteria included eyes with keratoconus or forme fruste keratoconus as demonstrated by corneal topography and/or Orbscan® (Baush & Lomb, Rochester, NY, USA). Eyes with suspected corneal dystrophy by slit-lamp examination, known ocular pathology, or previous ocular surgery were also excluded.
Data were analysed using SPSS for Windows (version 12.0, Chicago, IL, USA). The CCT measurements were averaged after collection and are presented as mean±SD. The two-tailed Student's t-test was used to compare mean values of parametric data. The categorical variables analysed were sex, and parents' and patient's place of birth. The continuous variables analysed were age, sphere, cylinder, IOP, keratometry, and CCT. Linear regression analysis and analysis of variance (ANOVA) were used to analyse the possible relationship between CCT and the other variables. Statistical analysis was performed for the right eye and the left eye separately. The results were considered significant for P-value of ≤0.05.
Results
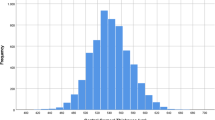
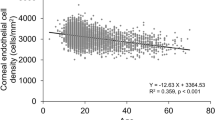
A total of 204 patients were included in this study. The demographic characteristics of the patients are given in Table 1. There were more females than males (58.8 vs 41.2%). The preoperative CCT, sphere, cylinder, keratometry, and IOP data of right and left eye are given in Table 2. In the total group, mean CCT was 529.91±33.66 μm in the right eye and 530.04±33.98 μm in the left eye. Patient's place of birth and origin (ie parents' place of birth) are given in Table 3. The majority of patients were born in Israel (n=144, 70.6%), and the majority of parents were born in North-Africa (n=121, 59.3%). Comparisons of preoperative examination data between patients of North-African origin and patients of other origins are presented in Table 4. CCT was found to be significantly thinner in patients of North-African origin (518.87±31.53 vs 545.36±30.44 μm in the right eye, and 518.43±32.07 vs 546.31±29.76 μm in the left eye; P≤0.0001). The distribution of the corneal thickness in the populations is presented in Figure 1. The majority of thinner corneas were present in people of North-African origin. People of North-African origin were also significantly older (35.9 vs 32.4 years, P=0.028). There were no differences between groups when comparing for sex (P=0.387), sphere (P=0.758 and 0.823), cylinder (P=0.60 and 0.619), keratometry (P=0.192 and 0.228), and IOP (P=0.070 and 0.073) for the right eye and the left eye, respectively.
The multivariate linear model of mean corneal thickness included sex, age, origin, preoperative sphere, cylinder, keratometry, and IOP. Only patient's origin was found to be independently associated with CCT (P<0.0001). The other tested variables were not independently associated with CCT (age, P=0.977; sex, P=0.987; sphere, P=0.998; cylinder, P=0.989; keratometry, P=0.978; and IOP, P=0.968).
Discussion
Doughty and Zaman30 recently performed a meta-analysis of the corneal thickness literature based on 300 articles. They concluded that the mean CCT of eyes reported as ‘normal’ was 534 μm. Overall, studies using slit-lamp-based pachymetry reported marginally lower CCT values (530±0.029 μm) compared to ultrasound-based studies (544±0.034 μm), but the authors attributed this difference to the type of individual studied (nonsurgical vs presurgical patients) rather than the technique itself.
CCT measurements have been reported in several ethnic groups and countries.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29 Overall, CCT was found to be significantly thinner in African-Americans with an average CCT value in the low 530's μm. Only in two studies from Mongolia15 and India,28 mean reported CCT was below 520 μm (495±32 and 519.92±33.36 μm, respectively). In the present study, we found significantly thinner corneas in people of North-African origin with an average of 518.87±31.53 μm (right eye) than people of other origins (545.36±30.44 μm, right eye) (Table 5).
CCT measurement can be affected by several factors: technique of measurement, age, diurnal effects, contact lens wearer, ocular disease, and previous ophthalmic surgery.30 Given the methodology used in this study, it is unlikely that methodological bias could be the explanation for the thinner corneas found in people from North-Africa. Specifically, all the measurements were performed with the same ultrasound pachymeter, by the same two examiners, at the same hours in the afternoon. All people coming to preoperative examination were instructed not to wear soft contact lenses 2 weeks before, or 4 weeks before in the case of gas-permeable and hard lenses. Finally, people with ocular disease (ie keratoconus, Fuchs dystrophy) or previous ocular surgery were excluded from this study. Regarding the age of the patients, we found that North-African people were significantly older (35.9 vs 32.4 years). A substantial age-related increase in CCT has been reported in ultrasound pachymetry studies (approximately 15 μm/decade).30 Thus, even accepting this possible age-related effect on CCT, we could expect thicker and not thinner corneas in people from North-Africa.
Preoperative parameters such as refractive status, keratometry, and IOP can theoretically affect CCT measurement, but no differences were found between the two groups. When we performed multivariate analysis, only patient's origin was found to be independently statistically associated with CCT. The other tested variables (age, sex, refractive status, keratometry, and IOP) were not associated with CCT.
To the best of our knowledge, there is only one report29 of CCT in people from Africa, other than African-Americans actually living in the United States and Canada. The authors reported that CCT measured by slit-lamp device in 38 males and 38 females in Rwanda was 524 and 521 μm, respectively, which is similar to the reported average CCT in a meta-analysis of 125 studies using slit lamp30 (525 vs 544 μm using ultrasound pachymetry). So these Rwanda people had ‘normal’ CCT values.
An important methodological issue is the decision to use the parents' place of birth and not the patient's place of birth as the indicator of ‘origin’ for the statistical analysis. Previous CCT measurements in different ethnic groups were based on self-definition by the patient and sometimes also confirmed by demographic information found in the patient's medical record. As Israel's present population originates from almost all around the world, a self-definition of ‘race’ would be problematic and racial backgrounds difficult to assess, so we preferred to gather ‘objective’ information on place of birth, leaving the determination of ‘origin’ to the algorithm created by the investigators. As a result of this variety, the Israeli population offers an excellent opportunity to compare people coming from different geographic regions.
One potential limitation of this report is that the study population was taken from people examined at a refractive clinic, and it is not a representative population-based sample. We can only conclude that people examined at a refractive clinic whose parents were born in North-Africa have significant thinner corneas than people of other origins. A population-based study is necessary to confirm our findings.
Possible reasons for different CCT values in different ethnic groups have not been reported. Genetic, environmental, climatic and/or multifactorial reasons could be responsible for these differences in CCT. What seems to be clear from our findings is the fact that people from North-Africa coming for refractive surgery had thinner corneas than the reported average values. With the advent of refractive laser procedures during the recent years, leaving a residual stromal bed of more than 250 μm in order to avoid postoperative keratectasia has been suggested.34 At this moment it is unknown whether or not North-African people are more prone to postoperative complications, certainly an issue that merits further study.
Also recently the importance of measuring CCT in all patients with glaucoma or ocular hypertension has been highlighted. In African-American people with glaucoma, Goldmann applanation tonometry uncorrected for CCT can lead to a higher morbidity probably secondary to delay in diagnosis and setting of inadequate treatment targets.4 In the mean time, until a larger study with different design can confirm our findings, it seems to be prudent to pay special attention to CCT in North-African people with glaucoma or at glaucoma risk.
References
Rapuano CJ, Fishbaugh JA, Strike DJ . Nine point corneal thickness measurements and keratometry readings in normal corneas using ultrasound pachymetry. Insight 1993; 18: 16–22.
La Rosa FA, Gross RL, Orengo-Nania S . Central corneal thickness of Caucasians and African Americans in glaucomatous and nonglaucomatous populations. Arch Ophthalmol 2001; 119: 23–27.
Brandt JD, Beiser JA, Kass MA, Gordon MO . Central corneal thickness in the Ocular Hypertension Treatment Study (OHTS). Ophthalmology 2001; 108: 1779–1788.
Shimmyo M, Ross AJ, Moy A, Mostafavi R . Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am J Ophthalmol 2003; 136: 603–613.
Nemesure B, Wu SY, Hennis A, Leske MC, Barbados Eye Study Group. Corneal thickness and intraocular pressure in the Barbados Eye Studies. Arch Ophthalmol 2003; 121: 240–244.
Hahn S, Azen S, Ying-Lai M, Varma R, Los Angeles Latino Eye Study Group. Central corneal thickness in Latinos. Invest Ophthalmol Vis Sci 2003; 44: 1508–1512.
Alsbirk PH . Corneal thickness. I. Age variation, sex difference and oculometric correlations. Acta Ophthalmol (Copenh) 1978; 56: 95–104.
Wong ACM, Wong CC, Yuen NSY, Hui SP . Correlational study of central corneal thickness measurements on Hong Kong Chinese using optical coherence, Orbscan and ultrasound pachymetry. Eye 2002; 16: 715–721.
Cho P, Lam C . Factors affecting the central corneal thickness of Hong Kong-Chinese. Curr Eye Res 1999; 18: 368–374.
Lam AK, Douthwaite WA . The corneal-thickness profile in Hong Kong Chinese. Cornea 1998; 17: 384–388.
Lam AK, Douthwaite WA . The effect of an artificially-elevated intraocular pressure on corneal thickness in Chinese eye. Ophthalmic Physiol Opt 1997; 17: 414–420.
Kang SW, Chung ES, Kim WJ . Clinical analysis of central islands after laser in situ keratomileusis. J Cataract Refract Surg 2000; 26: 536–542.
Wu LL, Suzuki Y, Ideta R, Araie M . Central corneal thickness of normal tension glaucoma patients in Japan. Jpn J Ophthalmol 2000; 44: 643–647.
Foster PJ, Wong JS, Wong E, Chen FG, Machin D, Chew PT . Accuracy of clinical estimates of intraocular pressure in Chinese eyes. Ophthalmology 2000; 107: 1816–1821.
Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ . Central corneal thickness and intraocular pressure in a Mongolian population. Ophthalmology 1998; 105: 969–973.
Copt RP, Thomas R, Mermoud A . Corneal thickness in ocular hypertension, primary open-angle glaucoma, and normal tension glaucoma. Arch Ophthalmol 1980; 117: 14–16.
Bechmann M, Thiel MJ, Neubauer AS, Ullrich S, Ludwig K, Kenyon KR et al. Central corneal thickness measurement with a retinal optical coherence tomography device versus standard ultrasonic pachymetry. Cornea 2001; 20: 50–54.
Wirbelauer C, Sholz C, Hoerauf H, Engelhardt R, Birngruber R, Laqua H . Corneal optical coherence tomography before and immediately after excimer laser photorefractive keratectomy. Am J Ophthalmol 2000; 130: 693–699.
Maldonado MJ, Ruiz-Oblitas L, Munuera JM . Optical coherence tomography evaluation of the corneal cap and stromal bed features after laser in situ keratomileusis for high myopia and astigmatism. Ophthalmology 2000; 107: 81–87; discussion 88.
Olsen T, Ehlers N . The thickness of the human cornea as determined by a specular method. Acta Ophthalmol (Copenh) 1984; 62: 859–871.
Nissen J, Hjortdal JO, Ehlers N, Frost-Larsen K, Sorensen T . A clinical comparison of optical and ultrasonic pachometry. Acta Ophthalmol (Copenh) 1991; 69: 659–663.
Wolfs RC, Klaver CC, Vingerling JR, Grobbee DE, Hofman A, de Jong PT . Distribution of central corneal thickness and its association with intraocular pressure: The Rotterdam Study. Am J Ophthalmol 1997; 123: 767–772.
Ustundag C, Bahcecioglu H, Ozdamar A, Aras C, Yildirim R, Ozkan S . Optical coherence tomography for evaluation of anatomical changes in the cornea after laser in situ keratomileusis. J Cataract Refract Surg 2000; 26: 1458–1462.
Morad Y, Sharon E, Hefetz L, Nemet P . Corneal thickness and curvature in normal-tension glaucoma. Am J Ophthalmol 1998; 125: 164–168.
Dohadwala AA, Munger R, Damji KF . Positive correlation between Tono-Pen intraocular pressure and central corneal thickness. Ophthalmology 1998; 105: 1849–1854.
Herse P, Yao W . Variation of corneal thickness with age in young New Zealanders. Acta Ophthalmol (Copenh) 1993; 71: 360–364.
Thomas R, Korah S, Muliyil J . The role of central corneal thickness in the diagnosis of glaucoma. Indian J Ophthalmol 2000; 48: 107–111.
Kunert KS, Bhartiya P, Tandon R, Dada T, Christian H, Vajpayee RB . Central corneal thickness in Indian patients undergoing LASIK for myopia. J Refract Surg 2003; 19: 378–379.
Forsius H, Maertens K, Fellman J . Change of the eye caused by the climate in Rwanda, Africa. Ophthalmic Epidemiol 1995; 2: 107–113.
Doughty MJ, Zaman ML . Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol 2000; 44: 367–408.
Brandt JD . Corneal thickness in glaucoma screening, diagnosis, and management. Curr Opin Ophthalmol 2004; 15: 85–89.
Shih CY, Graff Zivin JS, Trokel SL, Tsai JC . Clinical significance of central corneal thickness in the management of glaucoma. Arch Ophthalmol 2004; 122: 1270–1275.
Pallikaris IG, Kymionis GD, Astyrakakis NI . Corneal ectasia induced by laser in situ keratomileusis. J Cataract Refract Surg 2001; 27: 1796–1802.
Binder PS . Ectasia after laser in situ keratomileusis. J Cataract refract Surg 2003; 29: 2419–2429.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article has been accepted for oral presentation at the next American Society of Cataract and Refractive Surgery symposium, Washington, April 2005.
Rights and permissions
About this article
Cite this article
Lifshitz, T., Levy, J., Rosen, S. et al. Central corneal thickness and its relationship to the patient's origin. Eye 20, 460–465 (2006). https://doi.org/10.1038/sj.eye.6701911
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701911
Keywords
This article is cited by
-
Central corneal thickness in southern Egypt
International Ophthalmology (2014)
-
The impact of central corneal thickness on intraocular pressure among Ethiopian glaucoma patients: a cross-sectional study
BMC Ophthalmology (2012)