Abstract
Aim
To study the feasibility of a modified fast-track protocol for periocular basal cell carcinoma (BCC).
Methods
A modified protocol was set up with an aim to examine all periocular BCCs within 6 weeks of referral to our oculoplastic clinic. An audit of this protocol was performed over a 2-year period.
Results
A total of 65 patients were referred as a ‘possible BCC’ over the 2-year period. In all, 32 of these patients were referred by dermatologists (49%), followed by fellow consultant ophthalmologists (20 patients, 31%) and general practitioners (11 patients, 17%). The clinical suspicion in the oculoplastic clinic agreed with the referral diagnosis in 71% (46 of the 65) of patients. This figure was particularly high for referrals from dermatologists (84%). In all, 44 out of the 46 ‘clinically suspected BCC’ underwent surgical excision. Histopathology confirmed BCC in 39 of these 44 patients, a diagnostic accuracy of 89%. Among the subgroup of patients referred by the dermatologists, the largest source of referrals, 24 out of 30 patients that underwent surgical excision had histologically proven BCC; a diagnostic accuracy of 80%.
Conclusion
Our study shows that the modified fast-track protocol for periocular BCCs is practical and feasible. Such a practice is highly desirable since it prevents a long wait for patients who are aware of a possible malignant periocular lesion.
Similar content being viewed by others
Introduction
The department of health set a target in year 2000 that all suspected cancers should be seen within 2 weeks of referral.1 This has prompted a considerable debate in dermatology literature regarding the impracticality of including basal cell carcinomas (BCCs) in this fast-track protocol.2, 3, 4, 5 Although BCCs form the commonest periocular malignancy.6 there has been no published report on this subject in the ophthalmology literature.
Materials and methods
We set up a modified protocol in December 2000 wherein all letters with suspected periocular BCC referred to our oculoplastic service were vetted by one of the authors (SSM). Target was set for all ‘possible BCC’ patients to be seen within 6 weeks of referral. Each weekly oculoplastic clinic was prebooked to have two vacant ‘new patient’ appointment slots to accommodate such referrals. Slots that remained unused until a week prior to the clinic were given to any patient with other oculoplastic problems. After allowing some time for the system to become established, we audited the outcome of our practice over a 2-year period from July 2001 until June 2003.
Results
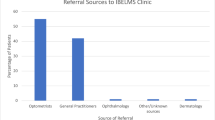
During the 2-year period 65 referral letters were received that were suggestive of a periocular BCC. The number of such referrals does not reflect the total number of cases of BCC in our practice since several other unsuspected (based on referral letters) cases of BCC were also seen eventually on a routine basis. Majority of patients were referred by dermatologists (32 patients, 49%), followed by fellow consultant ophthalmologists (20 patients, 31%) and general practitioners (11 patients, 17%) (Figure 1). Of the 65 ‘BCC-referrals’, 59 patients (91%) were seen in the oculoplastic clinic within the planned 6 weeks of referral (mean 4.5 weeks, range 1–10.1 weeks). Three patients were delayed by more than 8 weeks due to an administrative error in the early part of the study period.
At the time of first examination in the oculoplastic clinic 46 patients were suspected clinically of having a BCC. No surgical intervention was possible in two patients (one patient refused any surgery, one deceased prior to the surgery). BCC was confirmed on histopathology in 39 of the remaining 44 patients (88%). The distribution of the clinical and histological diagnosis is shown in Table 1.
Discussion
Several reports in the dermatology literature have sought to exclude BCCs from the 2-week cancer referral rule. The arguments are based on their high incidence, generally benign behaviour, little potential for handicap and a possible delay in seeing patients with other urgent conditions.2, 3, 4, 5 In our modified protocol we have tried to address these issues by allowing BCCs to be seen within 6 weeks of referral. By allocating two ‘new patient’ slots in each weekly oculoplastic clinic, we did not have to displace other patients to accommodate patients with a possible BCC. Any slots that remained unused were offered to patients with other oculoplastic problems, thus avoiding any wastage of resources.
In our series covering a 2 year period, 80% of the patients referred to our oculoplastic service with a possible BCC had been seen earlier either by consultant dermatologists or fellow consultant ophthalmologists; this would reflect a prior patient awareness of the possible diagnosis of a malignant periocular lesion. The clinical suspicion in the oculoplastic clinic agreed with the referral diagnosis in 71% (46 of the 65) of patients referred as BCC. This figure was particularly high for referrals from dermatologists (84%, 27 of 32 patients), which formed the single largest source of referrals. Malignant eyelid tumours are often misdiagnosed clinically by nondermatologists.7 In all, 14 of the 33 patients (42%) referred by nondermatologists with a possible diagnosis of BCC, were not considered to have a malignant lesion when seen in the oculoplastic clinic. These are patients who would otherwise have been needlessly anxious about their possible diagnosis of a malignant lesion. These statistics emphasise a clear need for a protocol to fast-track BCCs in ophthalmic practice.
The case mix in our cohort of 65 patients comprised of 60% histologically confirmed BCC, 29% clinically nonmalignant lesions and 8% that turned out to be nonmalignant histologically (in two clinically suspected BCC patients, histological confirmation was not possible). This is similar to a previously reported series where out of the 115 patients with a possible diagnosis of cutaneous BCC histologically confirmed BCC was 58% and 38% cases were nonmalignant lesions.5 Our outcome of 39 histologically proven BCCs among the 44 that underwent surgery reflects a diagnostic accuracy (DA) of 89% and index of suspicion 113% which compares well with published DA of 92% and index of suspicion 109% in a large series of 139 periocular BCC.8
Patients who may even be remotely aware that they might have cancer often want to see a specialist as soon as possible. Reassurances that BCC is a slowly progressive cancer may do little to relieve the anxiety suffered by such patients. This was often evidenced by our patients’ remarks when they attended the oculoplastic clinics. In our series 60% (39 out of 65) of patients referred as a ‘possible BCC’ were histologically confirmed to have BCC. If we consider the subgroup of patients referred by dermatologists, the single largest source of referrals of suspected BCC in our series, 24 out of the 30 patients had histologically proven BCC; a diagnostic accuracy of 80% as compared to 59–70% reported in the dermatology literature.8, 9 These figures clearly demonstrate that patients referred to our oculoplastic service as ‘possible BCC’ form a select group and adopting a fast-track protocol for this group gave a fairly high ‘positive yield’ in our practice without wasting valuable resources. We were able to see most of the patients within the set timeframe. The patients that were delayed by more than 8 weeks due to an administrative error were all in the initial part of the study period and this problem has been rectified since.
In conclusion, our study shows that the fast-track protocol to include BCC is practical; it does not waste resources and is desirable since it prevents a long wait for the patient who is aware of a possible malignant periocular lesion. For busy oculoplastic units, setting such a 6-week fast track for a select group of referrals such as by the dermatologists could be considered.
References
Department of Health. Faster and fairer access to cancer care — new cancer referral guidelines published. Press release ref. 2000/0200. Published 31/3/2000.
Cox NH . Evaluation of the UK 2-week referral rule for skin cancer. Br J Dermatol 2004; 150: 291–298.
Gordon PM, Cox NH, Paterson WD, Lawrence CM . Basal cell carcinoma: are early appointments justifiable? Br J Dermatol 2000; 142: 446–448.
Morris AD, Gee BC . The 2-week wait: to BCC or not to BCC? Br J Dermatol 2003; 148: 608–609.
Narayan S, de Berker D . Basal cell carcinomas and the 2-week wait. Br J Dermatol 2002; 147 (Suppl 62): 47.
Cook BE, Bartley GB . Epidemiologic characteristics and clinical course of patients with malignant eyelid tumours in an incidence cohort in Olmsted County, Minnesota. Ophthalmology 1999; 106: 746–750.
Lober CW, Fenske NA . Basal cell, squamous cell and sebaceous gland carcinomas of the periorbital region. J Am Acad Dermatol 1991; 25: 685–690.
Kersten RC, Ewing-Chow D, Kulwin DR . Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology 1997; 104: 479–484.
Presser SE, Taylor JR . Clinical diagnostic accuracy of basal cell carcinoma. J Am Acad Dermatol 1987; 16: 988–990.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interests: None.
Declaration: This paper has been previously presented as a poster at the annual meeting of the British Oculoplastic Surgery Society, 2004.
Rights and permissions
About this article
Cite this article
Bhatnagar, A., Mohamad, S. & Sandramouli, S. ‘Fast-tracking’ cancer referrals: application for periocular basal cell carcinoma. Eye 20, 428–430 (2006). https://doi.org/10.1038/sj.eye.6701894
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701894