Abstract
Aim
This prospective study aimed to clinically correlate the various ocular findings with the neurological status in cases of closed head injury.
Methods
A total of 200 consecutive cases of closed head injury admitted to a major teaching hospital underwent a thorough ophthalmic assessment. The Glasgow coma scale (GCS) and the Revised trauma score (RTS) were applied to grade the severity of injury and assess the prognosis. Kendall's tau-b and Fisher's exact test were used in the analysis.
Results
The main causes of head injury were road traffic accidents 52.5% followed by assaults in 34%. Ocular involvement was found in 167(83.5%) cases. These included corneal and scleral tears in 2%, subconjunctival haemorrhage or ecchymosis in 46%, orbital fractures 12%, pupillary involvement 6.5%, papilloedema 5.5%, intraocular trauma 5.5%, proptosis 3%, lateral rectus palsy 2%, lacrimal gland prolapse 1%, and optic nerve trauma 0.5%. All 21 patients (10.5%) who died had eye involvement. In all, 150 cases (75%) with a RTS of 12 had a good prognosis. Of these 124 (82.6%) had ocular involvement of no neurological significance.
Conclusions
Although sophisticated imaging techniques are available to localize lesions, early ophthalmic assessment in correlation with the GCS aids in prognosticating outcomes. Pupillary involvement, papilloedema, and ocular motor paresis pointed to a more severe head injury. To our knowledge, this is the only prospective study recording ocular findings in the first few hours and attempting a correlation with the final outcome.
Similar content being viewed by others
Introduction
A head injury occurs every 15 s and a patient dies of head injury every 12 min.1 Over 50% of all trauma deaths are associated with head injury and close to 60% of vehicular trauma deaths are due to head injuries.1
Head injuries are frequently associated with ophthalmic manifestations and consequent morbidity.2 Many of the ophthalmic findings are often ignored and present much later to specialist neuro-ophthalmic clinics. Clinical correlation of the ophthalmic findings is important in early localization of the site of injury, ongoing assessment, management and prognosis of the patient with head injury.
There are several studies of patients with head injuries in Rehabilitation units being referred for missed Neuro-ophthalmic findings.2, 3, 4, 5, 6, 7, 8 This study aims to record the various ocular findings in closed head injury and to attempt a correlation between the neurological signs, ocular signs, GCS, and outcome, thus getting closer to pinning down prognosticators of adverse outcome. To our knowledge, this is the only prospective study recording ocular findings in the first few hours following closed head injury.
Materials and Methods
A prospective study of 200 consecutive patients with isolated closed head injury admitted to a surgical unit of a busy University teaching hospital was carried out. The Glasgow coma scale (GCS) and the Revised trauma score (RTS) were applied to grade the severity of head injury and assess the prognosis in all cases. All patients with moderate and severe head injury and those dropping two scales on the GCS were CT scanned as appropriate by the neurosurgical team treating the patient. In all, 38 cases needed surgical intervention (19%).
Ophthalmic assessment of all patients with head injury was carried out irrespective of the presence or absence of ocular involvement. All the cases were reviewed daily by the same ophthalmic team, until the patients were discharged from the hospital. The Kendall's tau-b was applied to test the significant association of GCS and the patient's outcome in our study. The association between the GCS and ocular findings, neurodeficit and the final outcome of the patient was evaluated using the Fisher's exact test.
Results
In this study of 200 cases of closed head injury, 194 (97%) were males and six (3%) were females. The age ranged from 5 to 67 years, with a mean of 28.08 years. The age range for men was 5–67 years with a mean of 27.85 years. For women, the age ranged from 14 to 47 years with a mean of 35.33 years. Young adult males (21–30 years) were more vulnerable to head injury, 62% (n=124), as opposed to the 41–50-year-old bracket among the females, 2% (n=4) (Figure 1).
A majority of the 200 patients with head injury in our study were victims of road traffic accidents (52.5%), closely followed by assaults (34%) (Table 1). Other causes of head injury included falls, pedestrians hit by motor vehicles or cattle and, in one patient, walking into a cement wall.
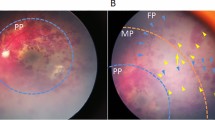
Ophthalmic examination was carried out in all the head injury cases within the first few hours of admission. Ocular involvement was found in 167 cases (83.5%). In all, 36/200 (18%) had intraocular involvement (Table 2a) of which four cases (2%) had corneal or scleral tears requiring surgery. Enucleation was inevitable in one case due to a large scleral tear. Optic nerve trauma resulted in blindness in one case.
The commonest eye finding was ecchymosis in 54/200 (27%) followed by subconjunctival haemorrhages in 38/200 (19%) patients (Table 2b). Orbital fractures were seen in 24 patients (12%) and of these four cases (16.7%) had a blow out fracture (Table 2c). In all, 51 /167 (30.5%) patients had a combination of two or more ocular findings such as ecchymosis, subconjunctival haemorrhage, orbital fracture, hyphaema, and scleral tears. The more severe injury was taken as the main ocular finding in head injury (Table 4)
Ophthalmic eye signs of neurological significance were found in 32/200 patients (16%), 28 of these patients (87.5%) were also associated with neurodeficits (Table 3). Pupillary involvement in 13/200 cases (6.5%) was the commonest neuro-ophthalmic sign followed by papilloedema in 11/200 cases (5.5%). All cases of papilloedema, abducent nerve palsy and traumatic optic neuropathy had additional neurodeficit. Majority of the patients with pupillary involvement (84%) and a third of the patients with ptosis also exhibited additional neurodeficit. The three patients with ptosis did not have any direct ocular trauma and the ptosis could be neurogenic in nature. Proptosis resolved in two cases but not completely in four. One of these was associated with persistent neurodeficit.
The association between ocular signs and the outcome was significant (P=0.003). A total of 21 patients (10.5%) with head injury died. Three died early (within 4 h), while five died within 24 h. A total of 13 patients died after 48 h.
All the patients that died had ocular involvement of neurological significance, and 13% of patients with ocular involvement died.
A correlation of ocular findings with the GCS and RTS in the first few hours following head injury was attempted (Table 4). In all, 150 patients (75%) had a mild head injury (GCS of 14–15 and RTS of 10–12) of which 124 (82.7%) patients had eye involvement of no neurological significance, including unilateral and bilateral ecchymosis (49), subconjunctival haemorrhages (38), orbital margin fractures in 12, proptosis in six, blow out fractures of the orbit in four, macular oedema in three cases, unilateral traumatic mydriasis, lacrimal gland prolapse, and scleral and corneal tears in two cases each, and hyphaema and vitreous haemorrhage in one case each (Table 5). None of the mild head injury cases died and only four of the 150 cases (2.7%) had minimal residual neurodeficit.
A total of 29 patients (14.5%) were graded as having incurred moderate head injury (GCS 9–13) of which 24 patients (82.8%) had ocular involvement. Nine patients had pupillary signs. Three patients with pupil involvement survived of which two had unilateral miosis and 1 had unilateral traumatic mydriasis. The initial papillary examination of six patients that died showed unilateral miosis (Hutchison's stage I) in one case, moderate unilateral pupillary dilatation (Hutchison's stage II) in three cases and unilateral dilation with miosis of the other pupil (Hutchison's stage III) in two cases. Papilloedema was seen in three (all of these patients died), lateral rectus palsy in four cases (two of these patients died), ecchymosis and orbital margin fractures in two cases each, retinal haemorrhage, macular oedema, ptosis, and traumatic optic neuropathy in one case each (Table 4). A total of 11 of the 29 (38%) patients with moderate head injury died and one case (3.4%) of traumatic optic neuropathy had residual neurodeficit.
There were 21 cases (10.5%) of severe head injury, of which eight patients that had papilloedema, and two patients with bilateral dilated pupils (Hutchison's stage IV) died. Six patients with orbital margin fractures and three with unilateral ecchymosis survived (Table 4).
The outcome was worse in patients with ocular involvement and neurodeficit (Table 5). In 21 of the severe head injury cases (GCS 3–8), 10 patients (47.6%) with associated ocular signs and neurodeficit, all died. Neuro-ophthalmic findings of pupillary involvement or papilloedema were a constant feature in the four patients (2%) who died (GCS 3–5 and RTS 0–3). Of the 11 patients that survived, two had neither eye signs nor demonstrable neurodeficit, while nine patients had only neurodeficit without any demonstrable ocular signs. Of the 179 patients with mild and moderate head injury 33 (18.4%) had associated demonstrable ocular signs and neurodeficit and a third of these patients died. A total of 168 patients with mild-to-moderate head injury had eye signs with neurodeficit in 22 patients, only eye signs in 115 patients, only neurodeficit in 11 patients, and no abnormalities in 20 (Table 5).
There was no significant difference between patients with eye signs displaying neurodeficit (26%) and those with no eye signs having neurodeficit (33%). Hence patients with eye signs were not more likely to have neurodeficit.
The following observation were made
-
Pupillary abnormalities (6.5%), papilloedema (5.5%) and lateral rectus palsy pointed towards a poorer outcome (Table 3).
-
The presence of eye signs did not mean that a patient was more likely to have neurodeficit (Table 5).
-
Association between the ocular signs and the outcome was significant (P=0.003) (Table 6). All the patients that died had ocular involvement and 13% of patients with ocular signs died.
-
In this study, patients with eye signs of neurological significance were more likely to have neurodeficit and to die than those with other eye signs or no eye signs.
-
There is a significant association between neurodeficit and outcome. Neurodeficit was found in all the patients that died (Table 6).
-
The outcome is worse in patients with GCS 6–8 with ocular involvement and neurodeficit (P<0.001 - Fisher's exact test), and those with GCS 11–12 and ocular signs (P=0.04) (Table 6).
The GCS, Neurodeficit and ocular signs contribute significantly to the prediction of outcome.
Discussion
Head injuries can be defined as those in which there is evidence of involvement of the brain including concussion, with loss of consciousness or post-traumatic amnesia, neurologic signs of brain injury or skull fractures.9 The Glasgow coma score and the Revised trauma scores are commonly used in grading the severity of head injury. The RTS is a triage tool and the score is inferred from physiologic derangement on initial evaluation. The data derived from these vital signs and levels of consciousness mathematically culminate into a single variable that correlates with mortality.1
Most head injury cases are mild and can be treated as out-patients. Those that need neuro-observation are treated as in-patients for 24–48 h. Less than one in 100 has a severe injury to the brain.10 The eyes are often involved in head injury (directly and indirectly) with neuro-ophthalmic deficits.2, 4, 5, 6, 7, 8, 11, 12
Most ophthalmologists when faced with injured patients tend to focus on obvious ocular manifestations such as contusions and laceration. Subtle manifestations may be equally important and may go unrecognized. Neuro-ophthalmic evaluation is challenging in head injury patients with reduced consciousness or coexisting injuries.
The incidence of head injury has been reported as 109 per 100 000 cases.13 As was found in our study, high velocity impact due to RTA is the commonest cause of head injury reported,4 with young men most frequently involved.2 Trauma patients often have multiple injuries including ocular involvement. Several retrospective studies have reported neuro-ophthalmic findings a few months after head trauma.2, 3, 4, 5, 6, 7, 8
This study has looked at the ocular findings in the acute stage of head injury. These included physical ocular trauma, orbital fractures and neuro-ophthalmic findings. Comprehensive ocular assessment can contribute significantly to the overall understanding of the acute injury and the prognosis of the patient as well as ocular motor involvement, profoundly affecting their rehabilitation.12 There is no formal estimate of the percentage of the total number of closed head injury patients who had visual symptoms or signs. An informal estimate was in the range of 30–50%.5
Patients with neuro-ophthalmic deficit following head trauma can be a diagnostic and therapeutic challenge partly due to the frequently vague nature of their visual complaints and their coexistent neurologic deficits. Pupil size and reaction to light is very important in the initial assessment of head injury cases. Apart from pupillary signs of uncal herniation and associated primary injuries to the globe, the ocular findings are of secondary importance during emergency management of the patient. Early signs of temporal herniation include ipsilateral miosis due to oculomotor nerve irritation (Hutchison's stage I) followed by paresis causing ipsilateral pupillary dilatation and a sluggish response to light (Hutchison's stage II). Progressive dilatation of the ipsilateral pupil and miosis of the contralateral pupil (Hutchison's stage III), heralds progressive IIIrd nerve palsy due to temporal lobe herniation, followed by bilateral dilation of the pupil (Hutchinson's stage IV). Bilateral dilated nonreactive pupils can also be due to inadequate brain perfusion.1 The eye and its adnexa are innervated by one-half of the cranial nerves, and 38% of all fibres in the central nervous system are concerned with visual function, so clinical findings of neuro-ophthalmological interest are frequently noted with head injury.3
Accurate ocular motility assessment within the first few hours of head injury is not possible with patients in coma. Many signs and symptoms like third nerve misdirection arise a few months after trauma.3 This could account for a different spectrum of ocular findings in our study as compared to other studies.5, 7 Our study reported lower ocular motor involvement (abducent nerve palsy in 2% of head injury cases), as compared to other retrospective studies which have included patients referred specifically for ophthalmic problems, even beyond 12 months after the initial head injury.5, 7 Moster et al8 reported III cranial nerve palsy in 30%, IV cranial nerve palsy in 26% and VI cranial nerve palsy in 22% cases. Mariak, after brain autopsy in 12 patients, found serious cranial nerve involvement in 75% of the fatal closed head injury cases.
Kowal's5 study reported problems of poor accommodation with one or more cases, convergence insufficiency or acquired pseudomyopia in 36%, vitreoretinal disturbances in 5.6% and vitreous haemorrhages in 3.7% patients. There was one case each of a macular hole, retinal tear and retinal detachment and the one patient who developed bilateral idiopathic blepharospasm also had unexplained diplopia.5 Ptosis without any evidence of oculomotor nerve palsy or lid or orbital damage was present in 2.5% cases,5 which was more than that seen in our study. We observed greater physical intraocular (5.5%) and extraocular (47%) trauma.
As in this prospective study, several retrospective studies have reported a high incidence of neuro-ophthalmologic findings after severe head injury.8 Commonly reported abnormalities by Moster et al were, traumatic optic neuropathy (18% as opposed to 0.5% in our study), homonymous hemianopia (15%) and Horner's syndrome (7%) and multiple abnormalities (42%).3, 5, 8 Cortical blindness was reported in 0.4–0.6% by Banks et al14 that was not seen in our series. Optic nerve disorder will cause some disturbance of visual function which may have nonspecific symptoms. Specific tests of optic nerve function such as contrast sensitivity, colour vision and optic nerve head morphology, field testing, and visually evoked potential could not be carried out in the acute setting of this study, hence subtle optic neuropathy, especially in cases with normal or near normal Snellen acuity, could have been missed.5
The mechanism of injury for optic neuropathy can be direct, indirect, or due to papilloedema.2 Contusion injuries to the optic nerve are not uncommon after a head injury. An amaurotic pupil is objective proof of an afferent lesion in the pupillary reflex (or a conduction defect in the optic nerve), while at the same time the motor limb (or a the third cranial nerve) is intact. It implies that a total and irrecoverable loss of vision has occurred in the affected eye although the optic nerve head may appear normal on admission. Countercoup contusion to the optic nerve has been reported to be transmitted through the temporal bone.3
Visual field testing was not possible in acute head trauma where the stabilization of the patient was more important. Surprisingly, none of the patients complained of double vision while admitted in hospital, however, seven patients did seek ophthalmic opinion for diplopia within a month of being discharged after their head injury.
Pupillary signs are of grave importance in indicating the site and severity of injury and in the prognosis of head injury. It aids in localizing the site of supratentorial injuries, extradural and subdural haemorrhages, and pontine lesions. Hutchison's pupillary signs indicate progressive coning and the need for emergent life-saving intervention. In this study, pupillary abnormalities, papilloedema, and lateral rectus palsy pointed towards a poorer outcome. Identifying these early would logically reduce the incidence of consequent morbidity and mortality (Table 3).
We faced some problems during patient assessment due to the fact that GCS is heavily weighted towards speech and eye opening. Some patients were unable to speak due to facial injury and eye opening was hindered by severe periorbital trauma/oedema.
Our present study has led us to make the following observations:
-
The presence of physical (non-neuro-ophthalmic) eye signs did not mean that a patient was more likely to have neurodeficit. Table 5.
-
Association between the ocular signs and the outcome was significant (P=0.003). In all, 13% of the patients with ocular signs died. Neurologically significant eye signs were present in 19% (32/167) patients with ocular involvement. All of the 21 patients who died had neurologically significant eye signs (Tables 3 and Table 4).
-
There is a significant association between neurodeficit and outcome. Neurodeficit was found in all the patients who died.
-
Patients with ocular signs and neurodeficit exhibited a progressively worse outcome as the GCS worsened (Table 4).
-
The GCS, neurodeficit and ocular signs contribute significantly to the prediction of outcome. This emphasizes the importance of integrating ophthalmic assessment into the routine head injury assessment. This aids in the follow-up, prognosis and further management of neurological deficits, thus reducing the incidence of late/missed diagnosis.
This study highlights the importance of a detailed early ophthalmological assessment in correlation with an overall clinical assessment of patients of head injury in prognosticating outcomes.
To our knowledge this is the only prospective study attempting a correlation between ocular findings and outcome of head injury.
References
ACS Committee on Trauma. Advanced Trauma Life Support Course for Physicians,, 3rd edn. Student Manual, American College of Surgeons: Chicago, 1993.
Van Stavern GP, Biousse V, Lynn MJ, Simon DJ, Newman NJ . Neuro-Ophthalmic manifestations of head trauma. J Neuro-Ophthalmol 2001; 21 (2): 112–117.
Smith JL . Some neuro-ophthalmological aspects of head trauma. Clin Neurosurg 1966; 13: 181–196.
Sabates N, Gonce M, Farris B . Neuro-ophthalmological findings in closed head trauma. J Clin Neuroophthalmol 1991; 11: 273–277.
Kowal L . Ophthalmic manifestations of head injury. Austra New Zealand J Ophthalmol 1992; 20: 35–40.
Lepore F . Disorders of ocular motility following head trauma. Arch Neurol 1995; 52: 924–926.
Mariak Z, Mariak Z, Stankiewicz A . Cranial nerve II – VII injuries in fatal closed head trauma. Eur J Ophthalmol 1997; 7: 68–72.
Moster ML, Volpe NJ, Kresloff MS . Neuro-ophthalmic findings in head injury. Neurol 1999; 52 (Suppl 2): A23.
Annegers JF, Grabow JD, Kurland LT, Laws ER . The incidence, causes, and secular trends of head trauma in Olmsted County, Minnesota, 1935–1974. Neurology 1980; 30: 912–919.
Clinical Guideline 4. Head Injury. Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults. National Institute for Clinical Excellence: London, June 2003.
Keane JR . Neurologic eye signs following motor vehicle accidents. Arch Neurol 1989; 46: 761–762.
Baker RS, Epstein AD . Ocular motor abnormalities from head trauma. Surv Ophthalmol 1994; 35: 245–267.
Thurman DJ, Jeppson L, Burnett CL, Beaudoin DE, Rheinberger MM, Sniezek JE . Surveillance of traumatic brain injury in Utah. West J Med 1996; 165: 192–196.
Banks M, Lessell, Simmons MD . Neuro-ophthalmology and Trauma. Int Ophthalmol Clin Ocular Trauma 2002; 42 (3): 1–12.
Acknowledgements
We would like to thank Mr Peter Nightingale, Statistics Department, University of Birmingham for the statistical analysis, and Mr Prasanna Pimpalnerkar, Microsoft Certified Professional for his technical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Poster presentation, Royal the College of Ophthalmologists Annual Congress, Manchester 2004.
Rights and permissions
About this article
Cite this article
Kulkarni, A., Aggarwal, S., Kulkarni, R. et al. Ocular manifestations of head injury: a clinical study. Eye 19, 1257–1263 (2005). https://doi.org/10.1038/sj.eye.6701753
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701753
Keywords
This article is cited by
-
Potential Mechanisms of Acute Standing Balance Deficits After Concussions and Subconcussive Head Impacts: A Review
Annals of Biomedical Engineering (2021)
-
Severe cranial neuropathies caused by falls from heights in children
Graefe's Archive for Clinical and Experimental Ophthalmology (2016)
-
Yield and clinical efficacy of funduscopic examinations performed in the pediatric emergency room
European Journal of Pediatrics (2014)
-
Ocular manifestations of head injury and incidence of post-traumatic ocular motor nerve involvement in cases of head injury: a clinical review
International Ophthalmology (2014)
-
A management algorithm for cerebrospinal fluid leak associated with anterior skull base fractures: detailed clinical and radiological follow-up
Neurosurgical Review (2012)