Abstract
Purpose
To study the safety and efficacy of immediate argon laser peripheral iridoplasty (ALPI) as initial treatment of acute phacomorphic angle-closure (phacomorphic glaucoma) before cataract extraction.
Methods
In all, 10 consecutive patients with acute phacomorphic angle-closure and intraocular pressure (IOP) ⩾40 mmHg were recruited into the study. Each patient received topical atropine (1%) and timolol (0.5%), and immediate ALPI as initial treatment. The IOP at 15, 30, 60, and 120 min, and then 1 day, after ALPI were documented by applanation tonometry. Systemic IOP-lowering drugs were only started if IOP remained above 40 mmHg at 2 h after ALPI. Cataract extraction was subsequently performed as definitive treatment.
Results
In total, 10 patients (five male, five female), with a mean age±SD of 73.1±10.3 years were recruited. Mean duration of symptomatic attack was 128±232 h. After ALPI, the mean IOP was reduced from 56.1±12.5 to 45.3±14.5 mmHg at 15 min, 37.6±7.5 mmHg at 30 min, 34.2±9.7 mmHg at 60 min, 25.5±8.7 mmHg at 120 min, and 13.6±4.2 mmHg at 1 day. In one patient, systemic acetazolamide was administered, because the IOP remained above 40 mmHg at 2 h after ALPI. All 10 patients had uncomplicated cataract extraction performed within 4 days after ALPI. No complications from the laser procedure were encountered.
Conclusion
Immediate ALPI, replacing systemic antiglaucomatous medications, appeared to be safe and effective as first-line treatment of acute phacomorphic angle-closure.
Similar content being viewed by others
Introduction
Acute phacomorphic angle-closure results from a rapid increase in antero-posterior diameter of a swollen, mature cataract. The thick cataract causes acute closure of the drainage angle, and hence rapid and gross elevation of intraocular pressure (IOP).1, 2, 3 Acute phacomorphic angle-closure was formerly known as ‘phacomorphic glaucoma’. Nowadays, a consensus is gradually established that the term ‘glaucoma’ implies glaucomatous optic neuropathy. In ‘phacomorphic glaucoma’, optic neuropathy is not inevitable, if the disease is recognized and treated early. For this reason, the authors believe that ‘acute phacomorphic angle-closure’ is a more appropriate name for this disease.
Acute phacomorphic angle-closure is still common in developing regions of the world where cataract extraction is not easily accessible. Patients with acute phacomorphic angle-closure usually complain of severe ocular pain, eye redness, headache, nausea, and vomiting. Treatment includes the immediate lowering of IOP with medications, and then subsequently removing the cause by cataract extraction,1, 3, 4 with or without a preceding laser iridotomy.5 Cataract extraction by both intracapsular4 and extracapsular6 techniques have been described in the literature. It may sometimes be necessary to combine cataract extraction with a filtration procedure to maintain IOP control.4, 7
The conventional initial treatment for acute phacomorphic angle-closure aims at rapidly reducing IOP, so as to relieve excruciating symptoms and prevent further irreversible ocular tissue damage,8 before the definitive treatment with cataract extraction can be safely performed. The initial treatment may involve one or more of the following IOP-lowering drugs: (1) topical beta-blocker, for example timolol;6 (2) systemic (oral/intravenous) carbonic anhydrase inhibitor, for example acetazolamide;1, 4, 6 (3) oral hyperosmotic agent, for example glycerol;4, 6 (4) intravenous hyperosmotic agent, for example mannitol.1, 4, 6 Topical miotic agent, for example pilocarpine,1, 4 and topical cycloplegic agent, for example, atropine, have both been used as part of the initial IOP-lowering regime in acute phacomorphic angle-closure. The authors favour a cycloplegic, rather than a miotic agent, as the miotic agent may increase axial lens thickness and cause anterior lens movement, and thus further shallowing the anterior chamber.9 Topical steroid may also be used to control inflammation before surgery.1
These treatments may fail to reduce IOP in up to 37.5% of acute phacomorphic angle-closure cases.4 Even when they are effective, they may take hours, or even days, to reduce IOP to a safe and symptom-free level. The longer the IOP is raised, the more irreversible damage there will be to the optic nerve head, iris, lens, and drainage pathways.8 Patients may suffer prolonged periods of excruciating symptoms. Furthermore, the systemic drugs may cause systemic side effects, such as paraesthesiae and drowsiness, or even confusion, loss of appetite, polydipsia and polyuria. More serious systemic side effects may also occur with carbonic anhydrase inhibitors, such as metabolic acidosis and electrolyte disturbance,10, 11 respiratory failure,12 Stevens–Johnson Syndrome,13 and blood dyscrasias.14 Systemic hyperosmotic agents can cause metabolic disturbance such as acidosis, pulmonary oedema and congestive heart failure, acute renal failure, and even intracranial haemorrhage and anaphylactic reaction.15, 16 For these reasons, current medical regimens to control IOP in acute phacomorphic angle-closure patients are not ideal.
Argon laser peripheral iridoplasty (ALPI)17 has been used to mechanically open up the angle in acute primary angle-closure (APAC). It involves the placement of a ring of contraction burns on the peripheral iris to contract the iris stroma near the angle. This mechanically pulls open the angle and lowers the IOP, allowing the eye to become quiet before the definitive treatment of laser peripheral iridotomy in APAC. The usual practice is to perform ALPI after maximal medications fail to control the IOP in APAC.17, 18 Peripheral iridoplasty has recently been applied as the initial IOP-reducing measure for APAC with good clinical outcomes, replacing systemic medications altogether.19, 20, 21, 22 The authors' randomized controlled trial has shown that in APAC, ALPI is safe, and more effective than conventional systemic medications in lowering IOP.21 No serious laser complications were encountered during the trial. The good results of ALPI as an initial treatment in APAC have led the authors to hypothesize that ALPI may work as effectively as a first-line therapy, replacing systemic IOP-lowering medications, in an analogous clinical situation: acute phacomorphic angle-closure. The efficacy of ALPI in reducing IOP in acute phacomorphic angle-closure has also been suggested by earlier studies.23, 24, 25
In summary, the potential advantages of immediate ALPI are: (1) shortening the period of high IOP, and thus minimizing the extent of ocular tissue damage, especially optic nerve head damage; (2) replacing the use of systemic carbonic anhydrase inhibitor and hyperosmotic agents, so that patients are spared the risk of any systemic side effects.21
This pilot study aims to investigate if ALPI is safe and effective as the initial IOP-lowering measure, replacing systemic IOP-lowering medications, in acute phacomorphic angle-closure before cataract extraction.
Materials and methods
The authors obtained prior approval of the study protocol by the Ethics Committee of The Chinese University of Hong Kong.
Acute phacomorphic angle-closure was diagnosed when a patient presented with one or more of the following symptoms: (1) acute onset of ocular pain; (2) headache; (3) nausea and vomiting; and on slit-lamp examination, the following signs were found: (1) grossly elevated IOP; (2) dense and swollen cataract; (3) severe diffuse anterior chamber shallowing; (4) corneal oedema; (5) anterior chamber inflammation and ciliary injection.
Study inclusion criteria were: (1) age over 18 years, and able to give informed consent and cooperate during laser procedure; (2) first acute attack of acute phacomorphic angle-closure; (3) IOP greater than or equal to 40 mmHg. Exclusion criteria included: (1) treatment received prior to presentation; (2) corneal opacity preventing laser treatment to over 90° of the peripheral iris; (3) patients in whom beta-blocker was contraindicated, for example, patients with chronic obstructive airway disease (COAD) and asthma. The study period was from January 2002 to December 2003.
In all, 10 consecutive patients fulfilling the above criteria were recruited into this study. Informed consents were obtained. Documentation of duration of symptomatic attack, best-corrected visual acuity, pain, nausea and vomiting, IOP, corneal oedema, pupillary reaction and size, and gonioscopy were performed. Each affected eye with acute phacomorphic angle-closure received one drop of 1% atropine eye drop, and one drop of topical timolol (0.5%). Immediate ALPI treatment was then applied to the attack eye.
ALPI was performed under topical anaesthesia with 1% amethocaine. The laser beam was focused onto the peripheral iris as close to the limbus as possible, with the use of an Abraham Iridectomy Laser Lens (Ocular Instruments, Inc., Bellevue, USA). All four quadrants (360°) were treated whenever possible. The end point was reached when localized iris contraction at area of treatment was visible.
IOP was measured using Goldmann applanation tonometry at 15 min, 30 min, 1 h, 2 h, and 1 day after ALPI. If IOP remained above 40 mmHg at 2 h, systemic medications would be started: intravenous acetazolamide 500 mg, and then oral acetazolamide 250 mg four times a day, with oral potassium supplement. If IOP remained above 40 mmHg at 4 h, intravenous mannitol would be administered (200 ml of 20% mannitol infused over 1 h). IOP would be documented hourly until it returned to below 25 mmHg.
Any pain, nausea and vomiting were documented 1 h after ALPI. Visual acuity, corneal oedema, and pupil size were recorded 1 h and 1 day after ALPI. Gonioscopy was repeated 1 day after treatment.
In all patients, the treated eye was maintained on topical 1% atropine twice a day, topical 0.5% timolol twice a day, and topical 1% Pred Forte six times a day, until the definitive treatment of cataract extraction could be performed.
Cataract extraction was performed as soon as IOP was controlled and the inflammation had largely settled. The date and time of performing cataract extraction were recorded. Any side effects and complications of treatment were recorded. Best-corrected visual acuity was documented 2 months after cataract extraction.
Results
In all, 10 consecutive patients with their first presentation of acute phacomorphic angle-closure were recruited into the study. The mean age±SD was 73.1±10.3 years (range, 60–91 years). There were five male and five female patients. There were five right and five left eyes. All 10 patients were of Chinese ethnic origin, with dark-brown irides. All 10 patients had no history of glaucoma or eye treatments.
The duration of symptomatic attack prior to presentation, as determined by the onset of symptoms, ranged from 5 h to 1 month (mean±SD, 127.8±232.1 h). One single patient presented particularly lately at 1 month after onset of symptoms. If this patient's duration of symptomatic attack was not counted, the mean±SD would have been 52.3±53.6 h.
The visual acuity at presentation ranged from light perception only (LP) to being able to count fingers (CF). Seven of the 10 patients had visual acuity of being able to detect hand movement only (HM) at the time of presentation.
Nine of the 10 eyes had a pupil nonreactive to light at presentation. The mean pupil diameter±SD was 4.2±1.3 mm (range, 2–6 mm). In the two patients with a relatively clear cornea, the angle was found to be closed on gonioscopy. In the remaining eight patients, we were not able to visualize the angle because of the corneal oedema.
At presentation, the IOP ranged from 41 to 75 mmHg (mean±SD, 56.1±12.5 mmHg). All ALPIs were performed within 30 min from the clinical diagnosis. ALPI was performed in the far periphery in all 360° of the iris. The mean number of contraction burns placed±SD was 46.6±11.9 (range, 32–75 burns). The mean laser power setting±SD was 264±73.4 mW (range, 180–420 mW). A laser spot size of 500 μm and a duration of 0.5 s were used in all 10 patients. All ALPIs were completed within 5–10 min.
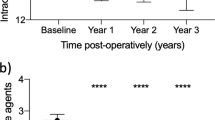
At 15 min after the ALPI, the mean IOP±SD dropped to 45.3±14.5 mmHg (range, 26–76 mmHg) (Figure 1). This represented a 19.3% reduction in mean IOP within 15 min from ALPI.
At 30 min after ALPI, the mean IOP±SD was 37.6±7.5 mmHg (range, 24–50 mmHg) (Figure 1). This represented a further 17.0% reduction in IOP, compared to the IOP at 15 min after ALPI, or a total reduction in IOP of 33.0% after 30 min.
At 1 h after ALPI, the mean IOP±SD dropped to 34.2±9.7 mmHg (range, 19–48 mmHg) (Figure 1). At 2 h after ALPI, the mean IOP±SD was 25.5±8.7 mmHg (range, 16–40 mmHg) (Figure 1). At 2 h, five of the 10 patients had IOP of 25 mmHg or below, and eight of the 10 patients were relieved of any eye pain or discomfort. One patient had IOP of 40 mmHg at 2 h after ALPI, and so was given intravenous and oral acetazolamide, with potassium supplement, according to the study protocol. The IOP in all 10 eyes returned to below 25 mmHg by 4 h after ALPI, and no patient was given intravenous mannitol for IOP control. No complications have arisen from the application of ALPI in the 10 patients.
On day 1 after ALPI, the mean IOP±SD was 13.6±4.2 mmHg (range, 7–20 mmHg) (Figure 1). Only one patient was receiving a systemic IOP-lowering drug (oral acetazolamide 500 mg four times a day), with potassium supplement. Visual acuity remained poor on day 1, due to the dense swollen cataract (range, LP to CF). All 10 eyes had re-established corneal clarity. On repeating gonioscopy on day 1, eight of the 10 eyes had an angle opening of grade 0 on the Shaffer scale in all 360°. In one eye, the angle was grade 0 on the Shaffer scale only in three quadrants, while in another eye, the angle had re-opened to grade 1 to 2 on the Shaffer scale in three quadrants.
Cataract extraction was performed on day 2 in three patients, day 3 in four patients, and day 4 in three patients. Six eyes had extracapsular cataract extraction by expression of complete nucleus, while four eyes had cataract extraction by phacoemulsification through a small incision. All 10 eyes had intraocular lens implanted at the completion of cataract extraction. All 10 patients were discharged from hospital soon after cataract extraction, and they have been followed up in the Glaucoma Subspecialty Clinic since discharge.
At the time of writing, the mean follow-up duration±SD for the 10 patients was 8.1±8.6 months (range, 1–23 months). The mean best-corrected or pin-hole visual acuity±SD at the last follow-up visit was 0.28±0.22 (range, 0.05–0.7, or 6/120 to 6/9). The diminished best-corrected or pin-hole visual acuity was due largely to glaucomatous optic neuropathy in seven eyes, and age-related macular degeneration in three eyes. In the eye with visual acuity of 0.05 (6/120), the optic nerve head was pale and deeply cupped, with a vertical cup-to-disk ratio of 0.95.
Mean IOP±SD at the final follow-up was 12.3±3.4 mmHg (range, 9–19 mmHg). One of the 10 eyes required topical timolol 0.5% to control IOP, while the remaining nine eyes required no IOP-lowering drug. None of the 10 eyes required any systemic IOP-lowering drug at the last follow-up visit. All 10 corneas were clear at the last visit. The mean cup-to-disk ratio±SD at the final visit was 0.52±0.17 (range, 0.3–0.9).
Up to the last follow-up, no major laser complications have arisen in the anterior segment of the 10 study eyes from the ALPI. None of the 10 eyes had irreversible peripheral corneal opacity or oedema. There was no irido-corneal adhesion. In all 10 eyes, there were faint laser marks still visible on the peripheral iris, but no significant iris atrophy was found in any of the 10 study eyes.
Discussion
ALPI was shown to be more effective than systemic medications in controlling IOP in a clinical condition analogous to acute phacomorphic angle-closure: APAC.21 In both APAC and acute phacomorphic angle-closure, the drainage angle is acutely closed, though with different mechanisms of closure. In both conditions, the IOP rises rapidly, giving rise to severe symptoms and also endangering ocular tissues. There is an urgent need to rapidly reduce IOP in both situations, before the definitive treatments (laser peripheral iridotomy in APAC, and cataract extraction in acute phacomorphic angle-closure) can be safely performed. This study sets out to examine whether ALPI can be an effective and safe alternative to systemic medications in the initial treatment of acute phacomorphic angle-closure, as in the case with APAC.
Our study demonstrated that ALPI can effectively lower the mean IOP from 56.1 to 25.5 mmHg in only 2 h in this series of acute phacomorphic angle-closure patients. In all 10 patients, the IOP was lowered to below 25 mmHg at 4 h after ALPI. In nine of these 10 patients, systemic IOP-lowering medications were not necessary, and so nine of these elderly patients (mean age, 73.1 years) were spared the potential systemic adverse effects of these medications. We were unable to compare the efficacy of ALPI directly with systemic medications, as there was not a control group in this preliminary study. Neither were there data documenting the IOP profile in phacomorphic patients after the administration of systemic IOP-lowering drugs in the published literature, as far as the authors are aware. Nevertheless, the fact that immediate ALPI alone was able to control the IOP in 90% of acute phacomorphic angle-closure patients compares favourably with published data on medical treatment of acute phacomorphic angle-closure. It was shown that medical treatment failed to control IOP in up to 37.5% of acute phacomorphic angle-closure patients.1
The mid-term clinical outcome of acute phacomorphic angle-closure patients treated with ALPI followed by cataract extraction is also encouraging. In our series, nine of the 10 eyes (90%) did not require any medications to control IOP at the final follow-up. In the literature, the proportion of acute phacomorphic angle-closure patients not requiring medications to control IOP after treatment with systemic medications and cataract extraction ranged from 754 to 93%.1
ALPI appears to be safe in acute phacomorphic angle-closure in this study. We have encountered no major laser complications. The only side effect we documented was the faint laser marks on the peripheral iris, which should not have any optical or functional effects, and were not noticed by any of our patients or their relatives.
Prudent case selection is essential to ensure safety. The authors believe that ALPI is relatively contraindicated in eyes with very severe corneal oedema, and very shallow anterior chamber. In the former situation, some corneal clarity can still be re-established by topical glycerin or hypertonic saline prior to ALPI. In the latter situation, laser applications can be timed enough apart to prevent the heat build-up that could injure the corneal endothelium. ALPI should also be used with caution in eyes with known poor corneal endothelial cell count or function, and in patients with known corneal endothelial dystrophy. ALPI is absolutely contraindicated in eyes with flat anterior chamber.
In a previous study of ALPI as the initial IOP-lowering treatment in APAC, it was shown by ultrasound biomicroscopy that ALPI re-opened the drainage angle in the APAC eyes.20 However, in the present study, eight of the 10 eyes had a closed angle in all 360° on repeating gonioscopy on day 1 after ALPI, despite a sustained reduction of IOP to below 21 mmHg. Mechanisms other than the reopening of the drainage angle may, therefore, be responsible for the IOP reduction. The authors postulate that the inflammation induced by ALPI might have caused increased aqueous outflow via the uveoscleral route. Alternatively, some reduction in aqueous production might also have resulted from the iridocyclitis induced by ALPI. These hypotheses were not tested by the present study.
One major shortcoming of ALPI in the management of acute phacomorphic angle-closure is that it requires a round-the-clock availability of both laser facility and an ophthalmologist who is experienced in anterior segment laser procedures. Acute phacomorphic angle-closure has higher incidence in developing countries, where early cataract surgery may not be accessible by all. The availability of laser facilities and expertise may be particularly difficult in these countries where the disease is most prevalent.
In one patient, the IOP actually increased from 50 to 76 mmHg after ALPI. It was in this patient that systemic acetazolamide was eventually administered, because the IOP was still 40 mmHg by 2 h after ALPI. The authors postulated that the initial IOP increase may be the result of iris pigment release and increase in inflammation caused by ALPI. The authors postulated that there were two opposing forces affecting IOP: pigment release and inflammation caused by ALPI that would decrease trabecular aqueous drainage and increase IOP, and reopening of the drainage angle by ALPI that would increase trabecular aqueous drainage and decrease IOP. In the majority of patients (nine out of 10), the latter force predominated and so IOP decreased. But in this single patient, the former force predominated and so there was an initial increase in IOP. It was not obvious to us why this particular patient had responded somewhat differently to the ALPI.
Figure 2 compares the IOP profiles after ALPI in acute phacomorphic angle-closure patients vs APAC patients. The APAC data were derived from the authors' earlier randomized controlled trial that compared ALPI against systemic IOP-lowering medications in the first-line treatment of APAC.21 In this earlier study, a total of 54 APAC eyes were randomized into the treatment group receiving immediate ALPI.21 There was no statistically significant difference between the presenting IOP of the APAC patients and the acute phacomorphic angle-closure patients (P=0.27, Student's t-test). However, the IOP at 15, 30, 60, and 120 min were significantly lower in the APAC patients than in the acute phacomorphic angle-closure patients (P=0.01, 0.03, 0.00, 0.00, respectively, Student's t-test). There was no statistically significant difference in IOP on day 1 between the two groups of patients (p=0.26, Student's t-test). It appears that ALPI reduces IOP more rapidly in APAC than in acute phacomorphic angle-closure patients. This does not, however, mean that ALPI is not an effective treatment in acute phacomorphic angle-closure. We would still need to compare ALPI directly with conventional systemic IOP-lowering medications to see if ALPI is more effective than the current treatment in acute phacomorphic angle-closure or not. It is the authors' impression that IOP reduction in acute phacomorphic angle-closure responds less readily to systemic medications than that in APAC, which may be explained by the difference in mechanism of angle closure. It was, therefore, not surprising to the authors that the IOP reduction from ALPI was less rapid in acute phacomorphic angle-closure, compared to APAC.
In conclusion, this preliminary study suggested that immediate ALPI could safely and effectively replace conventional systemic IOP-lowering medications in the initial treatment of acute phacomorphic angle-closure in the majority of patients, before the definitive treatment of cataract extraction. A large-scale randomized controlled trial to directly compare the efficacy and safety of immediate ALPI vs conventional systemic medications in the initial treatment of acute phacomorphic angle-closure is underway to find the best treatment for this disease.
References
Jain IS, Gupta A, Dogra MR, Gangwar DN, Dhir SP . Phacomorphic glaucoma-management and visual prognosis. Indian J Ophthalmol 1983; 31: 648–653.
Lim TH, Tan DT, Fu ER . Advanced cataract in Singapore—its prognosis and complications. Ann Acad Med Singapore 1993; 22: 891–894.
Epstein DL . Diagnosis and management of lens-induced glaucoma. Ophthalmology 1982; 89: 227–230.
Angra SK, Pradhan R, Garg SP . Cataract induced glaucoma—an insight into management. Indian J Ophthalmol 1991; 39: 97–101.
Tomey KF, al Rajhi AA . Neodymium:YAG laser iridotomy in the initial management of phacomorphic glaucoma. Ophthalmology 1992; 99: 660–665.
Prajna NV, Ramakrishnan R, Krishnadas R, Manoharan N . Lens induced glaucomas—visual results and risk factors for final visual acuity. Indian J Ophthalmol 1996; 44: 149–155.
Das JC, Chaudhuri Z, Bhomaj S, Sharma P, Gupta R, Chauhan D . Combined extracapsular cataract extraction with Ahmed glaucoma valve implantation in phacomorphic glaucoma. Indian J Ophthalmol 2002; 50: 25–28.
David R, Tessler Z, Yassur Y . Long-term outcome of primary acute angle-closure glaucoma. Br J Ophthalmol 1985; 69: 261–262.
Abramson DH, Franzen LA, Coleman DJ . Pilocarpine in the presbyope. Demonstration of an effect on the anterior chamber and lens thickness. Arch Ophthalmol 1973; 89: 100–102.
Chaparon DJ, Gomolin IH, Sweeney KR . Acetazolamide blood concentrations are excessive in the elderly: propensity for acidosis and relationship to renal function. Clin Pharmacol 1989; 29: 348–353.
Cowan RA, Hartnell GG, Lowdell CP, Baird IM, Leak AM . Metabolic acidosis induced by carbonic anhydrase inhibitors and salicylates in patients with normal renal function. Br Med J (Clin Res Ed) 1984; 289: 347–348.
Coudon WL, Block AJ . Acute respiratory failure precipitated by a carbonic anhydrase inhibitor. Chest 1976; 69: 112–113.
Shirato S, Kagaya F, Suzuki Y, Joukou S . Stevens–Johnson syndrome induced by methazolamide treatment. Arch Ophthalmol 1997; 115: 550–553.
Mogk LG, Cyrlin MN . Blood dyscrasias and carbonic anhydrase inhibitors. Ophthalmology 1988; 95: 768–771.
D'Alena P, Ferguson W . Adverse effects after glycerol orally and mannitol parenterally. Arch Ophthalmol 1966; 75: 201–203.
Spaeth GL, Spaeth EB, Spaeth PG, Lucier AC . Anaphylactic reaction to mannitol. Arch Ophthalmol 1967; 78: 583–584.
Ritch R, Liebmann JM . Argon laser peripheral iridoplasty. Ophthalmic Surg Lasers 1996; 27: 289–300.
Ritch R . Argon laser treatment for medically unresponsive attacks of angle-closure glaucoma. Am J Ophthalmol 1982; 94: 197–204.
Lai JS, Tham CC, Lam DS . Limited argon laser peripheral iridoplasty as immediate treatment for an acute attack of primary angle closure glaucoma: a preliminary study. Eye 1999; 13 (Part 1): 26–30.
Lam DS, Lai JS, Tham CC . Immediate argon laser peripheral iridoplasty as treatment for acute attack of primary angle-closure glaucoma: a preliminary study. Ophthalmology 1998; 105: 2231–2236.
Lam DS, Lai JS, Tham CC, Chua JK, Poon AS . Argon laser peripheral iridoplasty versus conventional systemic medical therapy in treatment of acute primary angle-closure glaucoma: a prospective, randomized, controlled trial. Ophthalmology 2002; 109: 1591–1596.
Tham CC, Lai JS, Lam DS . Immediate argon laser peripheral iridoplasty for acute attack of PACG (addendum to previous report). Ophthalmology 1999; 106: 1042–1043.
Liebmann JM, Ritch R . Glaucoma associated with lens intumescence and dislocation. In: Ritch R, Shields MB, Krupin T (eds). The Glaucomas. CV Mosby Co: St Louis, 1989, Chapter 49.
Ritch R, Solomon IS . Laser treatment of glaucoma. In: L'Esperance FAJ (ed). Ophthalmic Lasers, 3rd ed. CV Mosby Co: St Louis, 1989.
Ritch R, Liebmann J, Tello C . A construct for understanding angle-closure glaucoma: the role of ultrasound biomicroscopy. Ophthalmol Clin N Am 1995; 8: 281–293.
Acknowledgements
Financial support: Nil.
Proprietary interest: Nil.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented in part as a poster at the 7th Congress of the European Glaucoma Society in Florence, Italy, from 30 May to 4 June 2004.
Rights and permissions
About this article
Cite this article
Tham, C., Lai, J., Poon, A. et al. Immediate argon laser peripheral iridoplasty (ALPI) as initial treatment for acute phacomorphic angle-closure (phacomorphic glaucoma) before cataract extraction: a preliminary study. Eye 19, 778–783 (2005). https://doi.org/10.1038/sj.eye.6701651
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701651
Keywords
This article is cited by
-
Prospective study on retinal nerve fibre layer changes after an acute episode of phacomorphic angle closure
International Ophthalmology (2012)
-
Retrospective case series on the long-term visual and intraocular pressure outcomes of phacomorphic glaucoma
Eye (2010)
-
Immediate argon peripheral iridoplasty (ALPI) as initial treatment phacomorphic glaucoma: a safe and cost-effective treatment?
Eye (2006)
-
Reply to S Thyagarajan
Eye (2006)