Abstract
Purpose To report the use of commercially available preservative-free intravitreal triamcinolone acetonide for the treatment of macular oedema due to retinal vascular diseases.
Design Retrospective interventional case series.
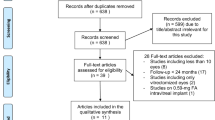
Methods Charts of eyes that received 4 mg preservative-free intravitreal triamcinolone acetonide for the treatment of persistent macular oedema due to retinal vascular diseases were reviewed. Patients were included if they had a follow-up of at least 3 months. Visual acuity, intraocular pressure, presence of an anterior chamber reaction, and mean macular thickness on optical coherence tomography (OCT) were recorded.
Results A total of 10 eyes of 10 patients were identified. Visual acuity improved by a mean of 1.1 Snellen lines at 1 month and 1.3 lines at 3 months. Macular thickness on OCT decreased by a mean of 183.5 μm at 1 month (P<0.0001). Intraocular pressure increased from a mean of 13.5 mmHg at baseline to 15.3 at 1 month, and 14.5 at 3 months. Only the 1-month change in intraocular pressure was statistically significant (P=0.0274). There were no cases of endophthalmitis, anterior chamber reaction, or retinal detachment.
Conclusion In this small retrospective, noncomparative series, commercially available preservative-free intravitreal triamcinolone acetonide had no adverse outcomes. Macular oedema was noted to decrease following treatment.
Similar content being viewed by others
Introduction
Intravitreal triamcinolone acetonide has been used for the treatment of macular oedema due to a variety of diseases. It has been shown to decrease macular thickness and improve vision in patients with macular oedema due to central retinal vein occlusions,1 diabetic retinopathy2 and uveitis.3 There are, however, concerns about the toxicity of the preservative used in commercially available Kenalog-40 (Bristol-Myers-Squibb, Peapack, NJ, USA). In addition to reports of bacterial endophthalmitis,4, 5, 6 sterile endophthalmitis has been reported following intravitreal triamcinolone injection.5, 7, 8 Sterile endophthalmitis presents as an anterior chamber reaction and vitritis approximately 3 days following intravitreal triamcinolone injection, and in one series has been described in 0.87% of eyes treated with intravitreal triamcinolone.9 The reason for this is unclear, but may be related to the vehicle or preservative used in commercially available Kenalog-40.
Benzyl alcohol, the preservative in intravitreal triamcinolone, was found to affect the B-wave on electroretinography, at concentrations higher than 1 mM.10 Hida et al11 investigated the vehicles in commercially available steroid compounds and found that the vehicle used in intravitreal triamcinolone was nontoxic in the four rabbit eyes administered it.
Benzyl alcohol has been found to be neurotoxic in the epidural space, where its use is discouraged. One case study12 reported flaccid paralysis of a primigravida who inadvertently received 40 ml sodium chloride 0.9% containing benzyl alcohol 1.5% in the epidural space. The authors identified benzyl alcohol as the probable cause of the neurotoxicity, although they did not expect the 600 mg dose given to elicit the reaction it did. Burk et al13 describe a technique for removal of the benzyl alcohol in their desire to avoid alcohol contact with the corneal endothelium during triamcinolone-assisted anterior vitrectomy. However, a more reliable way to remove the benzyl alcohol is not to include it in the preparation of the compound.
Methods
We obtained commercially available preservative-free triamcinolone acetonide from the New England Compounding Center, Framingham, MA, USA. Its ingredients are triamcinolone acetonide, polysorbate 80, dibasic sodium phosphate and monobasic sodium phosphate as buffering agents, polyglycol and sodium chloride 0.22%. It does not contain the 0.99% benzyl alcohol found in Kenalog-40. Its shelf life is 45 days.
We performed a review of 10 eyes of 10 patients who received 4 mg in 0.1 ml preservative-free triamcinolone for the treatment of macular oedema. The injections were performed as previously described, in an office setting.14 A drop of proparacaine 0.5% and a drop of ofloxacin 0.3% were administered to the eye. The eye was prepped with 10% povidone-iodine. An amount of 0.5 cc of lidocaine 1% was injected subconjunctivally. Following this, triamcinolone acetonide 4 mg in 0.1 ml was injected into the vitreous cavity 3.5 mm posterior to the limbus in the inferotemporal quadrant. An anterior chamber tap was then done to lower the intraocular pressure postinjection.
To be eligible for inclusion in the study, the indication for treatment was persistent macular oedema that did not respond to focal laser treatment (in cases of diabetic macular oedema and branch retinal vein occlusion) or posterior subtenon triamcinolone (in the case of the patient with sarcoid uveitis). All patients had a follow-up of 3 months. This was intended as a pilot study primarily to assess the safety profile of the preparation, as well as to assess visual outcomes and reduction in macular oedema using optical coherence tomography (OCT). Best corrected Snellen visual acuity, macular thickness on OCT and Goldmann intraocular pressure were noted from the charts at baseline, 1 week, 1 month, and 3 months after preservative-free intravitreal triamcinolone injection.
Results
The outcomes of the 10 eyes treated with preservative-free intravitreal triamcinolone are illustrated in Table 1. Two patients had cystoid macular oedema due to central retinal vein occlusion, and two patients had cystoid macular oedema due to branch retinal vein occlusion. Three patients had diabetic macular oedema, two had pseudophakic cystoid macular oedema (Irvine-Gass syndrome), and one patient had cystoid macular oedema due to chronic sarcoid panuveitis.
Visual acuity improved a mean of 1.1 Snellen lines at 1 month and 1.3 Snellen lines at 3 months. Macular thickness on OCT decreased by a mean of 183.5 μm, representing a 38.3% mean decrease in macular thickness at 1 month. The change in macular thickness was statistically significant (P<0.0001). There was no clinically significant rise in intraocular pressure for the 3 month follow-up period. Intraocular pressure increased from a mean of 13.5 mmHg at baseline to 15.3 mmHg at 1 month, and 14.5 mmHg at 3 months. Only the 1-month change in intraocular pressure was statistically significant (P=0.0274). There were no cases of endophthalmitis, pseudoendophthalmitis, anterior chamber reaction, or retinal detachment. No patients reported an acute worsening of vision.
With such a small number of patients in this pilot study, it is difficult to compare the standard intravitreal triamcinolone with the preservative-free triamcinolone. Although no patients in this series had a high intraocular pressure rise, we have previously noted a 10 mmHg or greater rise in intraocular pressure in 27.9% of 43 eyes within 12 weeks of a single 4 mg injection of intravitreal Kenalog-40.15 In our clinical observation, the triamcinolone appeared to disperse more in the vitreous rather than to clump, as was the tendency with the standard preparation of Kenalog-40. We have found that triamcinolone acetonide lasts for approximately 93 days in nonvitrectomized eyes,14 but without a pharmacokinetic study on the preservative-free intravitreal triamcinolone, it is unknown as to whether the intraocular duration of triamcinolone is different.
Conclusions
Preservative-free intravitreal triamcinolone appears to have a good safety profile in this pilot series of 10 patients. No patient had any adverse effects. There was a statistically significant reduction in macular thickness on OCT, suggesting that the medication is efficacious. Patient in our series had persistent macular oedema unresponsive to prior laser treatments, which may explain why some of them did not have any change in visual acuity. It may be that due to the chronic nature of macular oedema in these eyes, there was irreversible retinal damage, and concurrent macular ischemia, limiting further visual acuity improvement despite anatomic resolution of the oedema. Further studies are needed to compare the safety profile of intravitreal preservative-free triamcinolone with the standard preparation of Kenalog-40.
References
Greenberg PB, Martidis A, Rogers AH, Duker JS, Reichel E . Intravitreal triamcinolone acetonide for macular ooedema due to central retinal vein occlusion. Br J Ophthalmol 2002; 86(2): 247–248.
Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E et al. Intravitreal triamcinolone for refractory diabetic macular oedema. Ophthalmology 2002; 109(5): 920–927.
Antcliff RJ, Spalton DJ, Stanford MR, Graham EM, Ffytche TJ, Marshall J . Intravitreal triamcinolone for uveitic cystoid macular oedema: an optical coherence tomography study. Ophthalmology 2001; 108(4): 765–772.
Moshfeghi DM, Kaiser PK, Scott IU, Sears JE, Benz M, Sinesterra JP et al. Acute endophthalmitis following intravitreal triamcinolone acetonide injection. Am J Ophthalmol 2003; 136(5): 791–796.
Nelson ML, Tennant MT, Sivalingam A, Regillo CD, Belmont JB, Martidis A . Infectious and presumed noninfectious endophthalmitis after intravitreal triamcinolone acetonide injection. Retina 2003; 23(5): 686–691.
Benz MS, Murray TG, Dubovy SR, Katz RS, Eifrig CW . Endophthalmitis caused by Mycobacterium chelonae abscessus after intravitreal injection of triamcinolone. Arch Ophthalmol 2003; 121(2): 271–273.
Sutter FK, Gillies MC . Pseudo-endophthalmitis after intravitreal injection of triamcinolone. Br J Ophthalmol 2003; 87(8): 972–974.
Roth DB, Chieh J, Spirn MJ, Green SN, Yarian DL, Chaudhry NA . Noninfectious endophthalmitis associated with intravitreal triamcinolone injection. Arch Ophthalmol. 2003; 121(9): 1279–1282.
Moshfeghi DM, Kaiser PK, Bakri SJ, Scott IU, Sears JE, Benz M et al. Sterile endophthalmitis following intravitreal triamcinolone acetonide injection. Ophthalmic Surg Lasers Imaging, Submitted for publication.
Walter P, Luke C, Sickel W . Antibiotics and light responses in superfused bovine retina. Cell Mol Neurobiol 1999; 19(1): 87–92.
Hida T, Chandler D, Arena JE, Machemer R . Experimental and clinical observations of the intraocular toxicity of commercial corticosteroid preparations. Am J Ophthalmol 1986; 101(2): 190–195.
Craig DB, Habib GG . Flaccid paraparesis following obstetrical epidural anesthesia: possible role of benzyl alcohol. Anesth Analg 1977; 56(2): 219–221.
Burk SE, Da Mata AP, Snyder ME, Schneider S, Osher RH, Cionni RJ . Visualizing vitreous using Kenalog suspension. J Cataract Refract Surg 2003; 29(4): 645–651.
Beer PM, Bakri SJ, Singh RJ, Liu W, Peters III GB, Miller M . Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology 2003; 110(4): 681–686.
Bakri SJ, Beer PM . The effect of intravitreal triamcinolone acetonide on intraocular pressure. Ophthalmic Surg Lasers Imaging 2003; 34: 386–390.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bakri, S., Shah, A., Falk, N. et al. Intravitreal preservative-free triamcinolone acetonide for the treatment of macular oedema. Eye 19, 686–688 (2005). https://doi.org/10.1038/sj.eye.6701602
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701602
This article is cited by
-
Intravitreal Corticosteroids in the Management of Diabetic Macular Edema
Current Ophthalmology Reports (2013)
-
Retinal toxicity of triamcinolone’s vehicle (benzyl alcohol): an electrophysiologic and electron microscopic study
Graefe's Archive for Clinical and Experimental Ophthalmology (2007)