Abstract
Purpose
To assess the intraocular pressure (IOP) and corneal endothelial changes, over a 6-month period, after a single injection of intravitreal triamcinolone (ivTA) in Chinese patients.
Methods
A total of 43 eyes of 43 consecutive Chinese patients with various macular diseases received a single bolus injection of 4 mg ivTA, of which, 14 eyes with significant cataracts underwent simultaneous phacoemulsification and primary intraocular lens implantation. IOP was measured preoperatively and weekly in the first month, and then monthly until 6 months postinjection. Specular microscopy was performed on 24 of the 29 eyes without simultaneous cataract surgery, preoperatively and at months 1, 3, and 6.
Results
All patients completed 6 months of follow-up. Nine out of 43 (20.9%) eyes had IOP >21 mmHg. Their mean maximum IOP was 29.2 mmHg (range 23.0–37.0), necessitating the use of 2.0 types of topical antiglaucomatous medications on average. The IOP elevation occurred at a mean of 5.2 weeks (range 1–17) postinjection. All IOPs returned to normal, without additional antiglaucomatous medications, by 6 months. There was no statistically significant difference (paired t-test, P<0.05) in the corneal endothelial cell count and other specular microscopy parameters up to 6 months after the injections.
Conclusion
A single 4 mg bolus injection of ivTA appeared to have no harmful effects on the corneal endothelium. IvTA caused transient IOP elevations in 20.9% of Chinese patients, similar to that observed in Caucasians. As the IOP rise can occur as early as 1 week after the injection, early monitoring will help its early detection and prevent optic nerve damage.
Similar content being viewed by others
Introduction
In recent years, there have been promising reports of using triamcinolone acetonide as an intravitreal injection for the treatment of macular oedema that develops as a result of a number of ocular conditions, including diabetic retinopathy,1, 2 age-related macular degeneration,3 and others.4, 5, 6, 7, 8, 9 Although intravitreal triamcinolone (ivTA) has been shown to be relatively safe in animal models,10, 11 adverse events have been reported in humans.3, 12, 13, 14, 15, 16, 17 Elevation of intraocular pressure (IOP), thought to be a steroid response, is by far the most common adverse event, occurring in up to 52%13 of the patients who received the injection. An understanding of the dynamics of this elevation, including its timing and extent, would facilitate clinicians to have an early detection of the IOP rise and to initiate treatment promptly to prevent or minimize permanent damage to the optic nerve.
Previous reports have documented a difference in the prevalence of glaucoma in the Chinese population when compared to that in Caucasians,18 and that there was a differential glucocorticoid responsiveness in patients with primary open-angle glaucoma.19 Therefore, conceivably, Chinese patients may have a different prevalence of steroid-induced glaucoma, although there are no published figures on this. To our knowledge, there has been no study that examines the changes in IOP after ivTA injection in the Chinese populations and whether there is any difference in the response between this and the Caucasian population. In addition, the IOP response during the first few weeks after ivTA injections has not been clearly established. The first aim of the study was to investigate the early and mid-term IOP response to ivTA, including the timing of the responses. We then compared these changes with those reported in the literature on non-Chinese patients.
The increasing use of ivTA has led to concerns about its potential toxicity to the various ocular structures. Our recent in vitro studies showed that triamcinolone could exert a cytotoxic effect on retinal pigment epithelial cells and glial cells.20, 21 In addition to localizing in the vitreous cavity, triamcinolone has been detected in the aqueous humor after intravitreal injections.22 The presence of triamcinolone acetonide in the anterior chamber may affect the health of the corneal endothelium, which plays an important role in the function of the cornea. The second aim of the study was to investigate whether there were any adverse changes in the corneal endothelium following ivTA.
Materials and methods
The ethical approval for the study was obtained from the Clinical Research Ethics Committee of the Chinese University of Hong Kong, and the research was carried out according to the tenets of the Declaration of Helsinki. This prospective interventional case series was carried out at the Hong Kong Eye Hospital. Patients were recruited between July 2002 and June 2003, and informed consent was obtained from all patients.
A single bolus injection of ivTA (4 mg) was administered to Chinese patients above 18 years, with various macular conditions. These patients had central macular thickness of at least 250 μm as documented on ocular coherent tomography (StratusOCT™, Carl Zeiss). Patients with a history of raised IOP were not excluded, but the IOP had to have been stable and under control (less than 21 mmHg) for at least 3 months prior to enrolment. The exclusion criteria were: (1) previous ocular trauma and ocular surgery other than cataract extraction; (2) ocular or laser surgery within a 3-month period before injection; (3) presence of vitreous haemorrhage; and (4) proliferative diabetic retinopathy and other ocular conditions requiring immediate treatment. If significant lens opacity was present, cataract extraction by phacoemulsification with intraocular lens implantation was performed, and the ivTA injection was given at the end of the cataract surgery. For patients who received bilateral ivTA injections, only the first injected eye was included for analysis, to eliminate the problem of correlation between the two eyes of a patient.
Intravitreal injection procedure
The procedure was performed using standard aseptic techniques. After sterilization with 5% povidone iodine, 2% lidocaine hydrochloride gel (Xylocaine, AstraZenec) was applied as a local anaesthetic. Triamcinolone acetonide (4 mg (0.1 ml of 40 mg/ml)) (Kenacort A, Bristol-Myers Squibb, Anagni, Italy) was injected through the pars plana (4 mm post-limbus in phakics and 3.5 mm post-limbus in pseudophakics) using a 27 G needle. From our experience, we know that the volume effect of the ivTA can cause a significant immediate spike in IOP up to 50 mmHg post injection; therefore, anterior chamber paracentesis with a K-blade (K20-1710, Katena Products, Inc., Denville, USA) was performed if necessary to counteract this effect. Indirect ophthalmoscopy and IOP examination were performed after the procedure. Gutt Levofloxacin (Cravit, Santen, Osaka, Japan) was given stat, then 4 times per day for 2 weeks.
Simultaneous cataract extraction
Under topical anaesthesia and after standard cataract extraction by phacoemulsification and intracapsular intraocular lens implantation, 4 mg of triamcinolone was injected through the pars plana, 3.5 mm posterior to the limbus using a 27 G needle. There were no perioperative complications in any of our patients. Postoperatively, Gutt 1% prednisolone acetate (Predforte, Allergan, Westport, Ireland) and Gutt Levofloxacin or Gutt 0.5% Chloramphenicol (Martindale Pharmaceuticals, Romford, England) were used four times a day for 1 week, and then weaned down weekly over a 3-week period.
The patients were examined preoperatively and postoperatively at weeks 1,2,3,4 and months 2,3,4,5 and 6 for data collection. In addition, the patients also attended on postoperative day 1 and as necessary to ensure patient safety. At each data collection visit, which took place between 2 and 5 pm, the IOPs were measured with a non-contact tonometer (Xpert NCT Plus. Reichert Ophthalmic Instruments), taken as the average of three reliable readings. If the IOP was greater than 20 mmHg, it was verified with a Goldman applanation tonometer. Previous studies have demonstrated that the Xpert NCT system provided reliable IOP measurements, especially in the normal range,23, 24 and we believe that it served as a good non-invasive alternative to applanation tonometry for screening purposes.
While IOP was measured on all the eyes, for corneal endothelial changes, we did not include eyes with simultaneous cataract surgery, since intraocular surgery is known to affect the corneal endothelium. Non-contact specular microscopy (SM), using the Konan Noncon Robo Ca Sp 8000 specular microscope (Konan Inc., Hyogo, Japan), was performed on the central cornea before ivTA injection and at months 1, 3, and 6 after the injection.
Statistical analysis was performed with the Analysis ToolPak of Microsoft Excel 2002 (Microsoft Cooperation.), using the t-test. A difference was considered statistically significant if P<0.05.
Results
Single bolus ivTA injections (4 mg) were administered in a total of 43 eyes of 43 consecutive patients. In all, 29 eyes received ivTA injection alone and 14 had simultaneous cataract surgery. Of the 43 patients, 22 were male and 21 female. The average age was 67 years (range 34–86 years). In all, 38 eyes had macular oedema, caused by diabetes in 28 and by central or branch retinal vein occlusion in 10. Five eyes had other miscellaneous macular conditions (myopic choroidal neovascularization, cellophane maculopathy, age-related macular degeneration, Coates-like disease, and radiation retinopathy). All patients completed 6 months of follow-up.
IOP analysis
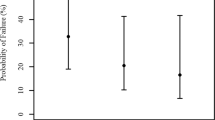
In all, 43 eyes of 43 patients were included in the analysis. The mean baseline IOP was 12.9 mmHg (standard deviation, SD 2.9 mmHg), the mean maximum IOP was 18.9 mmHg (SD 6.2 mmHg), and the difference was statistically significant (paired t-test, P<0.001). The mean maximum IOP was calculated as the group average of the maximum IOP recorded for each individual. Nine out of 43 eyes (20.9%) developed an IOP of >21 mmHg. In terms of IOP elevation, 17 (39.5%) had a rise of 2.0–4.9 mmHg, 11 (25.6%) had a rise of 5.0–9.9 mmHg, and seven (16.3%) had a rise of ≥10 mmHg. For the nine eyes with IOPs of more than 21 mmHg, the mean maximum IOP was 29.2 mmHg (range 23.0–37.0 mmHg) and the mean elevation from baseline was 14.2 mmHg (range 6.7–23.0 mmHg). The distribution of maximum IOPs is summarized in Figure 1. Topical antiglaucomatous treatments were initiated if the IOP rose above 21 mmHg and additional medications were added, until the IOP was controlled to below 21 mmHg. An average maximum of 2.0 additional topical antiglaucoma medications per eye was required. The treatment was tapered or stopped when the ivTA crystals were no longer visualized in the vitreous space and if the IOP was under control. The duration of time during which the additional antiglaucoma treatment was required to control the IOP to below 21 mmHg is summarized in Figure 2. All the IOPs returned to normal on no additional antiglaucomatous treatment by 6 months. Out of the 43 eyes, one had a history of primary open-angle glaucoma (POAG) and one had ocular hypertension (OHT). Both eyes were in the ivTA alone group and both developed an IOP of >21 mmHg. Their maximum IOPs were 26 and 37 mmHg (mean 31.5 mmHg) with rises of 6.7 and 23.0 mmHg, respectively. For those without a raised IOP history, the rate of IOP >21 mmHg was 7/41 (17.1%), and the mean rise was 5.6 mmHg (SD 5.0 mmHg). The difference in the extent of IOP elevation between those with and without a raised IOP history was statistically significant (t-test, P=0.02). Most of the patients initially developed an IOP of >21 mmHg at or before 2 months (see Figure 3). The mean interval between injection and IOP rise was 5.2 weeks (SD 4.9 weeks).
The comparative data between the groups with and without simultaneous cataract surgery are summarized in Table 1. The average age of patients with an IOP rise of >21 mmHg was 64.6 years and those without was 68.1 years (no statistically significant difference, t-test P=0.32).
Specular microscopy
SM examination was added after the start of the study and was not performed on the initial five eyes. It was performed on 24 of the 29 eyes that had ivTA injections alone without simultaneous cataract surgery. Of these, 18 were phakic and six were pseudophakic. The following parameters, generated by the specular microscope's built-in software, were analysed: (1) endothelial cell density (cell/mm2); (2) mean cell size (unit: 100 mm2); (3) coefficient of variation of cell area (standard deviation/average) × 100; and (4) percentage of hexagonal cells (%).
In terms of all the four parameters mentioned above, there was no statistically significant difference (paired t-test, P<0.05) between the findings at baseline and at 1, 3, and 6 months. The findings, including the power calculations, are summarized in Table 2. Of note, the average baseline corneal endothelial cell count (2555±SD372/mm2) was not significantly different from that at 6 months (2518 ±SD 363/mm2) (paired t-test, P=0.52).
Discussion
The ocular hypertensive effects of ivTA injection are well documented. Depending on the dosage of triamcinolone used, the definition of IOP elevation, and whether eyes with a history of glaucoma were excluded, the percentage of IOP rise ranged from 11 to 52%.1, 2, 3, 12, 13, 14, 25 In concordance with the published studies, we found an increase in IOP in a significant proportion of eyes (20.9%, >21 mmHg), and the ocular hypertensive effect was mostly transient.
There were two main findings in our study. First, by reviewing the patients frequently during the first month after injection, we noted that the IOP response could appear as early as 1 week post injection. This occurred in one eye with a history of ocular hypertension that received ivTA alone. Five out of the nine eyes (55%) with IOP elevation developed the initial rise at or before 3 weeks, and eight out of nine (88%) before 3 months. In most of the previously published studies, after the postoperative day 1 visit, the patients were followed up at 1 or 3 months, in which case these 55 or 88% of eyes with IOP elevation would have been missed, respectively. If the IOP elevations were not detected and treated, the IOP could rise to a much higher level than reported here.
Second, the steroid response rate in our Chinese patient population was similar to those studies carried out in Caucasian patients when 4 mg of ivTA was used. Concurring with other studies, the probability and extent of IOP rise was higher in those with a history of POAG or OHT. Thus, a history of raised IOP can be considered a relative contraindication to ivTA treatment and these patients warrant careful monitoring if ivTA was given. Contrary to a previous report,13 we did not find the IOP elevation to be related to patient age. It was also interesting to note, from our study and other published articles, that the proportion of patients with an IOP rise with 4 mg is generally lower than the published figures of the one group who used 25 mg.2, 13, 25 Since the dose of 25 mg was mainly used by Jonas et al only, it was difficult to draw conclusions regarding whether triamcinolone caused a dose-dependent ocular hypertensive effect or whether the higher dose conferred any additional therapeutic benefit. A randomized controlled trial with different dosages of triamcinolone is necessary to answer this question.
When the eyes were divided into ivTA alone and ivTA plus cataract surgery groups, we had anticipated that the ivTA plus cataract surgery group would develop more of an IOP response, due to the additional topical steroids given in the postoperative period. However, if we excluded the two eyes with a raised IOP history, that were both in the ivTA alone group, the average maximum extent of IOP rise from baseline in the ivTA alone group was 6.4±SD 5.7 mmHg and 4.0±SD 2.8 mmHg in the ivTA plus cataract surgery group. The difference did not reach statistical significance (P=0.13).
Insults on the cornea, since as cataract surgery26 and ageing,27 can cause a deterioration of the corneal function, which is reflected by a decrease in the number of corneal endothelial cells, and an increase in variation of cell area (polymegethism) and cell size (pleomorphism). The variation of cell area is represented by the mean cell size and the coefficient of variation. The variation of cell size is represented by the percentage of hexagonal cells. In our study, ivTA injections did not have a statistically significant effect on the corneal endothelial cell numbers, areas, and sizes within the 6-month period. We also believe that the changes observed are unlikely to be of clinical significance. For example, for the endothelial cell count, it has been suggested that a loss of 2–3% should be considered with caution;28 in our series, however, the mean endothelial cell loss was only 0.85% by 6 months.
The major drawbacks in both parts of the study were the short follow-up time, the heterogeneous nature of the patients, the relatively small patient numbers, the lack of a control group, and the use of non-contact tonometry instead of Goldman applanation. The anterior chamber paracentesis performed at the time of the injection would have lowered the IOP, but the effect was transient and should counteract the volume effect of ivTA injection. We trust that it would not have significantly affected the IOP at 1 week.
While our patient number was relatively small, we had a zero dropout rate. In addition, we had frequent initial IOP monitoring that was not performed in other published studies.
In conclusion, a single bolus injection of 4 mg ivTA exerted an ocular hypertensive effect in a significant proportion of patients, which could be brought under control with topical antiglaucomatous medications. The IOP elevation usually resolved when the triamcinolone crystals were absorbed. In clinical practice, ivTA should be used with caution in patients with a history of POAG and OHT. To detect the ocular hypertensive response promptly, it is worth considering more frequent follow-ups in the first few weeks post injection. A single injection of 4 mg ivTA did not appear to cause appreciable SM changes within 6 months of injection. Since the therapeutic effects of ivTA may be transient,1, 2, 4 repeated injections may be necessary and further studies have to be conducted to characterize the IOP response to repeated injections in the long term.
References
Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology 2002; 109: 920–927.
Jonas JB, Kreissig I, Sofker A, Degenring RF . Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol 2003; 121: 57–61.
Spaide RF, Sorenson J, Maranan L . Combined photodynamic therapy with verteporfin and intravitreal triamcinolone acetonide for choroidal neovascularization. Ophthalmology 2003; 110: 1517–1525.
Park CH, Jaffe GJ, Fekrat S . Intravitreal triamcinolone acetonide in eyes with cystoid macular edema associated with central retinal vein occlusion. Am J Ophthalmol 2003; 136: 419–425.
Young S, Larkin G, Branley M, Lightman S . Safety and efficacy of intravitreal triamcinolone for cystoid macular oedema in uveitis. Clin Exp Ophthalmol 2001; 29: 2–6.
Benhamou N, Massin P, Haouchine B, Audren F, Tadayoni R, Gaudric A . Intravitreal triamcinolone for refractory pseudophakic macular edema. Am J Ophthalmol 2003; 135: 246–249.
Martidis A, Duker JS, Puliafito CA . Intravitreal triamcinolone for refractory cystoid macular edema secondary to birdshot retinochoroidopathy. Arch Ophthalmol 2001; 119: 1380–1383.
Alldredge CD, Garretson BR . Intravitreal triamcinolone for the treatment of idiopathic juxtafoveal telangiectasis. Retina 2003; 23: 113–116.
Rechtman E, Allen VD, Danis RP, Pratt LM, Harris A, Speicher MA . Intravitreal triamcinolone for choroidal neovascularization in ocular histoplasmosis syndrome. Am J Ophthalmol 2003; 136: 739–741.
McCuen BW, Bessler M, Tano Y, Chandler D, Machemer R . The lack of toxicity of intravitreally administered triamcinolone acetonide. Am J Ophthalmol 1981; 91: 785–788.
Hida T, Chandler D, Arena JE, Machemer R . Experimental and clinical observations of the intraocular toxicity of commercial corticosteroid preparations. Am J Ophthalmol 1986; 101: 190–195.
Wingate RJ, Beaumont PE . Intravitreal triamcinolone and elevated intraocular pressure. Aust NZJ Ophthalmol 1999; 27: 431–432.
Jonas JB, Kreissig I, Degenring R . Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol 2003; 87: 24–27.
Bakri SJ, Beer PM . The effect of intravitreal triamcinolone acetonide on intraocular pressure. Ophthalmic Surg Lasers Imaging 2003; 34: 386–390.
Sutter FK, Gillies MC . Pseudo-endophthalmitis after intravitreal injection of triamcinolone. Br J Ophthalmol 2003; 87: 972–974.
Roth DB, Chieh J, Spirn MJ, Green SN, Yarian DL, Chaudhry NA . Noninfectious endophthalmitis associated with intravitreal triamcinolone injection. Arch Ophthalmol 2003; 121: 1279–1282.
Benz MS, Murray TG, Dubovy SR, Katz RS, Eifrig CW . Endophthalmitis caused by Mycobacterium chelonae abscessus after intravitreal injection of triamcinolone. Arch Ophthalmol 2003; 121: 271–273.
Quigley HA . Number of people with glaucoma worldwide. Br J Ophthalmol 1996; 80: 389–393.
Clark AF . Steroids, ocular hypertension, and glaucoma. J Glaucoma 1995; 4: 354–369.
Yeung CK, Kwok PC, Chan CK, Pang CP, Lam DS . The cytotoxicity of triamcinolone on cultured human retinal pigment epithelial cells: comparison with dexamethasone and hydrocortisone. Jpn J Ophthalmol 2004 (in press).
Yeung CK, Kwok PC, Chiang SW, Pang CP, Lam DS . The toxic and stress responses of cultured human retinal pigment epithelium (ARPE19) and human glial cells (SVG) in the presence of triamcinolone. Invest Ophthalmol Vis Sci 2003; 44: 5293–5300.
Beer PM, Bakri SJ, Singh RJ, Liu W, Peters III GB, Miller M . Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology 2003; 110: 681–686.
Hansen MK . Clinical comparison of the XPERT non-contact tonometer and the conventional Goldmann applanation tonometer. Acta Ophthalmol Scand 1995; 73: 176–180.
Popovich KS, Shields MB . A comparison of intraocular pressure measurements with the XPERT noncontact tonometer and Goldmann applanation tonometry. J Glaucoma 1997; 6: 44–46.
Jonas JB, Kreissig I, Hugger P, Sauder G, Panda-Jonas S, Degenring R . Intravitreal triamcinolone acetonide for exudative age related macular degeneration. Br J Ophthalmol 2003; 87: 462–468.
Bourne WM, Kaufman HE . Cataract extraction and the corneal endothelium. Am J Ophthalmol 1976; 82: 44–47.
Laule A, Cable MK, Hoffman CE, Hanna C . Endothelial cell population changes of human cornea during life. Arch Ophthalmol 1978; 96: 2031–2035.
Kohnen T . Corneal endothelium: an important structure for cataract and refractive procedures. J Cataract Refract Surg 1997; 23: 967–968.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial and proprietary interest: Nil.
Financial Support: Nil.
Presentation: The data in this paper were presented in part as an oral presentation at the 4th Congress of the Asian-Oceanic Glaucoma Society, 1–4 October 2003, Hong Kong.
Rights and permissions
About this article
Cite this article
Chan, C., Fan, D., Chan, Wm. et al. Ocular-hypertensive response and corneal endothelial changes after intravitreal triamcinolone injections in Chinese subjects: a 6-month follow-up study. Eye 19, 625–630 (2005). https://doi.org/10.1038/sj.eye.6701585
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701585
Keywords
This article is cited by
-
Intraoperative intravitreal triamcinolone acetonide injection for prevention of postoperative inflammation and complications after phacoemulsification in patients with uveitic cataract
BMC Ophthalmology (2021)
-
Short-term effect of intracameral triamcinolone acetonide on corneal endothelium using the rabbit model
Eye (2007)