Abstract
Purpose
To compare the additive intraocular pressure (IOP)-lowering effects of latanoprost 0.005% and brimonidine 0.2% in primary open-angle glaucoma (POAG) patients uncontrolled on fixed combination of timolol 0.5% and dorzolamide 2% (TDC) alone.
Methods
In all, 80 eyes of 80 POAG patients with IOP inadequately controlled by TDC were randomly assigned to receive either latanoprost 0.005% or brimonidine 0.2%. IOP measurements were recorded at 1000 (peak effect) and 1600 (trough effect) on day 0 (baseline) and at 1 and 3 months. At each stage and time point, the mean IOP reductions from baseline were evaluated for both groups, and success rates (minimum 15% reduction) were determined.
Results
At baseline, the mean peak/trough IOPs with TDC were 20.2/21.6 and 19.9/21.4 mmHg in latanoprost and brimonidine groups, respectively. Latanoprost+TDC reduced the mean peak/trough IOP by 4.4/3.4 and 5.2/3.5 mmHg at 1 and 3 months. The corresponding values for brimonidine+TDC were 3.9/2.9 and 4.6/2.9 mmHg. Each of these results represented a significant reduction from baseline (P<0.001 for all); however, the groups’ peak/trough reductions from baseline did not differ at any time point (P>0.05 for all). With the latanoprost+TDC combination, the peak/trough success rates at 1 and 3 months were 76.3%/42.1% and 77.1%/40%. The corresponding values with the brimonidine+TDC combination were 71.8%/41% and 77.7%/41.7%. There were no significant differences in the groups’ success rates at any time point (P>0.05 for all).
Conclusion
Addition of latanoprost 0.005% or brimonidine 0.2% to TDC reduces peak/trough IOPs significantly and the effects of these combinations are comparable.
Similar content being viewed by others
Introduction
Increased intraocular pressure (IOP) can lead to glaucoma, and lowering the IOP is the only treatment that effectively preserves optic nerve function and stability of visual fields.1, 2, 3, 4, 5 Recent clinical trials, such as the Advanced Glaucoma Intervention Study (AGIS) and the Collaborative Initial Glaucoma Treatment Study (CIGTS), have shown the importance of lowering IOP for preventing progression of visual field loss.3, 4 The results of the AGIS showed that visual field progression was prevented only in eyes that had IOP lower than 18 mmHg at all clinical visits during the study.3 The results also revealed that IOP values in the low teens were required to prevent further damage in eyes with advanced glaucoma damage.3 In line with these findings, 5-year data from the CIGTS showed the importance of lowering IOP aggressively from baseline to prevent visual field damage.4 These two studies demonstrated that the target pressures required to prevent visual field progression are lower than previously thought.
In recent years, the monotherapy options for medical treatment of glaucoma have increased with the development of many new drugs; however, most patients require more than one pharmacological agent to lower IOP aggressively and achieve target pressures. Today, we can combine topical carbonic anhydrase inhibitors, prostaglandin analogues, and α2-adrenergic agonists with IOP-reducing agents that are already widely used, such as beta-blockers. This has substantially increased the number of possible combinations and the efficacy of treatment.
Combinations of two IOP-lowering agents with different mechanisms of action are often used to treat glaucoma patients whose target pressures cannot be achieved with monotherapy. In some cases where target pressures cannot be reached with two-drug combinations, it is acceptable to attempt adding a third drug as a last step before surgery. Efficacy, safety, and compliance are the most important aspects of these multi-drug therapies.
Cosopt® (timolol 0.5% and dorzolamide 2%, Merck Sharp & Dohme, NJ, USA) is a commercially available fixed combination of timolol and dorzolamide (TDC). This product requires instillation of fewer drops per day than the concomitant use of the two drugs separately. Such combination agents are more convenient to use, and thus may increase patient compliance with therapy. Combining TDC with other agents may be a good three-drug option in patients whose target pressures cannot be reached with other treatments. Using the combination drug TDC with a second agent, such as latanoprost or brimonidine, requires only two bottles of medicine and three or four drops per day, which is a fairly simple and practical regimen.
Latanoprost and brimonidine have both become popular among ophthalmologists for combination purposes, and as effective monotherapies.6, 7, 8, 9, 10, 11 Latanoprost is a PGF2α agonist that increases aqueous outflow mainly via the uveoscleral pathway.8, 9, 10, 12 It is advantageous as a complement to timolol or dorzolamide because of its additive effect with these agents.6, 7, 8 Brimonidine is a highly selective α2-adrenergic agonist that has also proven to be an effective IOP-lowering agent when used as an adjunct to other antiglaucoma medications.8, 10, 13
The aim of this study was to investigate the efficacy and safety of latanoprost and brimonidine as adjunctive therapies for glaucoma patients whose IOP is uncontrolled by TDC.
Materials and methods
This prospective, open-labelled, randomized study was designed to compare the efficacy and safety of latanoprost 0.005% (Xalatan®, Pharmacia & Up-John, Kalamazoo, Michigan, USA) and brimonidine 0.2% (Alphagan®, Allergan, Irvine, California, USA) as adjunctive therapies with a fixed timolol 0.5% and dorzolamide 2% combination (Cosopt®) in primary open-angle glaucoma (POAG). The investigation included 80 eyes of 80 Caucasian patients who were diagnosed with POAG and whose IOPs were inadequately controlled by TDC. The study was conducted between November 2001 and June 2002 and the patients were recruited in a continuous cohort after approval from the hospital ethics committee. In each patient, data from the eye with the highest IOP at baseline were recorded for analysis. All the subjects had been on TDC for 4–6 months when they were enrolled in the study. The patients had all been treated with beta-blockers or prostaglandin analogues in the past, and had switched to TDC treatment because of insufficient IOP control with monotherapy. Only eyes that had at least two IOP measurements higher than 18 mmHg in the 3 months prior to the study were included. For each of these individuals, this IOP level exceeded the target pressure that was set for the patient by their physician.
The exclusion criteria were as follows: known sensitivity/allergy to the study medications; IOP higher than 34 mmHg; women of childbearing age, presence of any uncontrolled systemic disease; any corneal surface abnormality, best-corrected visual acuity worse than 20/200; history of previous laser surgery or intraocular surgery; any type of closed-angle or secondary glaucoma. Patients with cup-to-disc ratio greater than 0.8 and patients with only one eye were not included in this study.
IOPs were measured with a Goldmann applanation tonometer twice daily at 1000 (±30 min) and 16:00 (±30 min) h on day 0 (baseline) and at the end of 1 and 3 months. At least three measurements were taken by an examiner who was unfamiliar with the patients and the groups in which they were assigned. The average of these three measurements was then recorded for analysis in each case. All measurements were taken by the same examiner with the same equipment throughout all the study period.
Patients were maintained on their pre-established twice-daily regimen of TDC (0730/1930 h) and were randomly assigned treatment with either latanoprost once daily (2200 h) or brimonidine twice daily (0800/2000 h).
The 1000 h IOP records were chosen to reflect the peak drug efficacy for dorzolamide (2.5 h after dose was administered), brimonidine (2 h after dose), and latanoprost (12 h after dose). The 1600 h IOP measurements were taken to reflect the trough drug efficacy for dorzolamide (approximately 8.5 h after dose), brimonidine (8 h after dose), and latanoprost (18 h after dose).
Effective therapy was defined as a minimum 15% reduction from baseline IOP. Each patient was asked about any adverse effect(s) without emphasizing on particular symptom at each visit. Every visit included measurement of visual acuity levels with Snellen chart, biomicroscopic evaluation of the anterior segment structures, and fundus for each patient. The therapy was discontinued if the complaint(s) of the patient or physician's assessment(s) were severe and thought to be drug-related.
Statistical analyses were performed using a commercially available statistical package (SPSS for Windows v9.0, SPSS Inc., Chicago, USA). Two-tailed, independent-sample t-tests were used to compare the differences between baseline and treatment IOP in the two study groups. Paired-sample t-tests were used to compare findings within the treatment groups. χ2 testing was used to analyse nominal and dichotomous data, including numbers of eyes with 15% or more IOP reduction, patient sex, and number of eyes with adverse events. The study had 64% power to detect a difference of 1 mmHg and had 99% power to detect a difference of 2 mmHg for IOP change from baseline for both study groups, assuming a standard deviation of 2.65, α=0.05, two tailed. The power was 87% to detect a difference of 1 mmHg between the two study groups, assuming a standard deviation of 2.05, α=0.05, two tailed.
Results
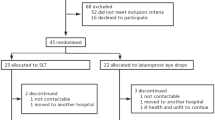
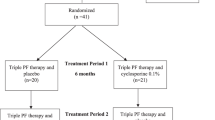
During the first month, two patients in the latanoprost group and one patient in the brimonidine group were removed from the study. Another three patients from the latanoprost group and three patients from the brimonidine group were removed from the study before the end of 3 months. Of the five latanoprost cases, two eyes were lost to follow-up and treatment was discontinued due to adverse events in three eyes. Of the four brimonidine cases, two were lost to follow-up and treatment was discontinued due to adverse events in two eyes. Due to these changes, 1-month follow-up data were available for 38 eyes in the latanoprost group and 39 eyes in the brimonidine group, and 3-month follow-up data were available for 35 eyes in the latanoprost and 36 eyes in the brimonidine group. Table 1 summarizes the demographic data for the 80 total patients who were initially enrolled in the study.
The main outcome measures of this study were the IOP-lowering effects of latanoprost and brimonidine as adjunctive therapy to TDC. There were no significant differences between the mean baseline IOP measurements in the two study groups (P=0.808 for 1000 h and P=0.810 for 1600 h measurements). In both groups, the mean IOP reductions at the 1000 h visits were greater than the reductions observed at the 1600 h visits.
Table 2 summarizes the mean IOP values and mean IOP reductions for both groups. After 1 month of treatment, the mean IOP reduction at the 1000 h visit was 4.4 mmHg (21.8%) in the latanoprost group and 3.9 mmHg (19.6%) in the brimonidine group. These were both significant decreases from the groups’ baseline mean IOPs (P<0.001 for both). After 3 months of treatment, the mean IOP reduction at the 1000 h visit was 5.2 mmHg (25.7%) in the latanoprost group and 4.6 mmHg (23.1%) in the brimonidine group (Figure 1). These were also significant reductions from the baseline mean IOPs (P<0.001 for both).
Comparison of the 1000 h findings at each of the three stages (baseline, 1 month, 3 months) revealed no significant differences between the groups with respect to mean IOP values or mean IOP reductions from baseline (mean IOP values: P=0.695 for 1 month and P=0.491 for 3 months; mean IOP reductions: P=0.565 for 1 month and P=0.367 for 3 months).
For the 1600 h visits, after 1 month of treatment the mean IOP reduction was 3.4 mmHg (15.7%) in the latanoprost group and 2.9 mmHg (13.6%) in the brimonidine group. Both these decreases were statistically significant (P<0.001 for latanoprost, P=0.003 for brimonidine). After 3 months of treatment, the mean IOP reduction at the 1600 h visit was 3.5 mmHg (16.2%) in the latanoprost group and 2.9 mmHg (13.6%) in the brimonidine group (Figure 2). These reductions were also statistically significant (P<0.001 for both).
Comparison of the 1600 h findings at each of the three stages (baseline, 1 month, 3 months) revealed no significant differences between the groups with respect to mean IOP values or mean IOP reductions from baseline (mean IOP values: P=0.595 for 1 month and P=0.543 for 3 months; mean IOP reductions: P=0.650 for 1 month and P=0.494 for 3 months).
After 1 month of therapy, 29 of 38 (76.3%) eyes in the latanoprost group and 28 of 39 (71.8%) eyes in the brimonidine group showed at least 15% IOP reduction with the adjunctive therapy at the 1000 h visit. In contrast, only 16 of 38 (42.1%) eyes in the latanoprost group and 16 of 39 (41.0%) eyes in the brimonidine group showed this degree of change at the 1600 h visit. There were no significant differences between the groups with respect to the numbers of eyes with 15% or more IOP reduction after 1 month (P=0.651 for 10:00, P=0.923 for 1600 h).
After 3 months of treatment, 27 of 35 (77.1%) eyes in the latanoprost group and 28 of 36 (77.7%) in the brimonidine group showed a minimum 15% IOP reduction at the 1000 h visit. At the 1600 h visit, 14 of 35 (40%) eyes in the latanoprost group and 15 of 36 (41.7%) eyes in the brimonidine group showed this degree of change. There were also no significant differences between the groups with respect to the numbers of eyes with 15% or more IOP reduction after 3 months (P=0.949 for 1000 h, P=0.886 for 1600 h).
Both brimonidine and latanoprost were well tolerated throughout the study period, and few side effects were noted. As mentioned above, three patients in the latanoprost group and two in the brimonidine group withdrew from the study due to adverse events. Ocular itching and burning was the reason for discontinuation in two patients in the latanoprost group and one patient in the brimonidine group. The other case in the latanoprost group developed diffuse redness, tearing, and swollen lids. One patient in the brimonidine group developed eye irritation with diffuse punctate epitheliopathy. There was no significant difference between rates of adverse events in the groups (P=0.644). There were no systemic side effects in either group during the study period.
Discussion
This study compared the efficacy and safety of latanoprost and brimonidine as adjunctive therapies for POAG patients whose IOPs were not adequately controlled by TDC. Each of the groups showed significant reductions from baseline mean IOP at both visit times at 1 and 3 months; however, the group results were similar at each visit time during each stage of the study.
Success rate was defined as the number of eyes that achieved a minimum 15% IOP reduction, and both study groups had high success rates at the 1000 h visits. However, the success rates at the 1600 h visits were nearly half those observed at the morning. We consider both these combinations efficacious in the morning hours, but the lower success rates in the afternoon indicate that the dosing regimens would have to be changed to increase the efficacy. Both regimens include three different pharmacological agents, so finding the optimal dosing regimen that covers all 24 h of the day is a complex task. Shifting the second dose of TDC to an earlier hour, around 1600 h, may help achieve better diurnal IOP control.
Our main focus in this study was to determine whether three-agent combination therapy is logical, effective, and safe in POAG patients. This also raises a second question: What is the number of drugs can be used as maximal medical therapy for glaucoma, and do fixed combinations like TDC (Cosopt®) count as one or two agents when totalling the number of drugs used? Today, the target IOP values in glaucoma management are lower than they were in the past. This, combined with the potential for serious complications in filtering surgery, is why multi-agent combinations are still popular. Over the past 15 years, three new classes of IOP-lowering drugs (topical carbonic anhydrase inhibitors, α2-mimetics, and prostaglandin analogs) have been added to the armamentarium for antiglaucoma therapy. There are many pharmacological agents in these drug classes, and this has led to tens of new drug combinations. Currently, there is little or no clinical information available concerning the efficacy and safety of most of these combinations.
When using multi-agent therapies, the three important issues are efficacy, safety, and compliance. Both combinations in this study were safe and effective at lowering IOP. Also, since both combinations require patients to carry only two bottles and instill four or less drops per day, one would not expect compliance to be any different from a regimen involving two separate drugs. Both of these combinations require fewer drops per day compared to the once-popular combination of beta-blocker twice daily and pilocarpine four times daily. Further studies would be required to determine patient compliance for the combinations used in our study.
One possible source of bias in this study is the different number of bottles that the patients have been given. The physician who took the IOP measurements was masked to the group assignments, but the unequal instillation schedule between the groups as the use of two-drugs BID in one group and one-drug BID and one-drug QHS in the other prevents this study to be double-masked. A possible design would be masking the bottles by giving two bottles for each patient (each bottle containing the same medication in brimonidine group, and one bottle containing latanoprost and one bottle containing saline in the latanoprost group). On the other hand, this would increase the number of bottles used (three bottles for each patient) in the study, whereas we were testing the efficacy of two-bottle therapy and may cause a decrease in compliance of the patients.
Many previous investigations have demonstrated the effect of adding timolol to dorzolamide.14, 15, 16 Both these agents reduce IOP via the same mechanism of action, namely, inhibition of aqueous formation. It has been speculated that the both drugs we tested in this study have additive IOP-lowering effects with TDC, since latanoprost increases uveoscleral outflow and brimonidine increases the outflow and also inhibits aqueous formation.
Simmons and Samuelson8 have examined the additive IOP-lowering effects of latanoprost and brimonidine as third-line adjunctive agents. In that report, 20 patients who were receiving a non selective beta-blocker and dorzolamide were randomly assigned to receive either brimonidine or latanoprost. At the peak drug effect, the IOP reductions were 5.29 mmHg (26.8%) for the brimonidine group and 3.21 mmHg (17.2%) for the latanoprost group. Defining success as 15% or more IOP reduction, the authors observed 84.6% success in the brimonidine group and 66.7% in the latanoprost group. There were no significant differences between the two groups with respect to mean IOP reduction and success rates, but the success rate was lower in the patients who received latanoprost. These results are comparable to our IOP reductions and success rates at the 1000 h visit times (peak drug effect). However, as described above, we noted lower drug effectiveness in the afternoon hours. Unfortunately, the corresponding data were not reported in the previous study. In contrast to our observations, the authors noted that 10% of the patients in the brimonidine group had to be removed from the study due to allergic adverse effects.
In another study that involved 52 eyes, latanoprost was added to a regimen of timolol and dorzolamide, and a diurnal tension curve for each eye was derived from four IOP measurements per day.17 The mean maximum IOP reduction at peak drug effect was 16.6%, and the mean minimum IOP reduction at trough drug effect was 15.6%. In the same report, 36.3% of the eyes achieved IOP reduction greater than 20%, and 59% reached IOP reduction greater than 10%.
The above results and the findings of our investigation demonstrate that the triple-agent combined therapies that we used have additive IOP-lowering effects, yield good success rates especially at peak drug effect, and produce no significant side effects. However, the success rate (min. 15% IOP reduction from baseline level) drops to 40% level at 1 and 3 months in both treatment groups at 1600 h measurements that reflected the trough drug efficacy. This result confirms the previous studies that documented the importance of multiple IOP measurements during the day in order to evaluate the effectiveness of a specific glaucoma therapy.18, 19, 20, 21 Another important outcome of this result is that only in a short percentage of patients (40%), the drug combinations that we tested were effective throughout the whole 24-h interval. In the remaining 60% of patients whose IOP were uncontrolled with a three-agent combination, probably, surgery should be the next step in treatment.
Single-agent therapy is always the first strategy used in patients with glaucoma. No second agent is added until monotherapy with different classes of agents has been attempted and has failed. The second step in the treatment algorithm is two-agent combination therapy, and fixed combinations are good choices for this purpose. When target IOPs cannot be achieved with a two-drug regimen, adding a third agent can be tried as a last step before surgery. To avoid increasing the number of solutions that need to be instilled each day, a fixed-combination drug such as TDC can be combined with an α2-mimetic or a prostaglandin analogue. Our study results show that latanoprost+TDC and brimonidine+TDC are both effective and safe combinations. In order to select the best combination regimen, each patient must be evaluated individually, especially with respect to risk factors for side effects. In addition, the effectiveness of the chosen combination must be monitored closely.
References
Sommer A, Tielsch JM, Katz J, Quigley HA, Gottsch JD, Javitt J et al. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch Ophthalmol 1991; 109: 1090–1095.
Kass MA, Heuer DK, Higginbotham EJ, Johnson JA, Keltner JL, Miller JP et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 701–713.
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 2000; 130: 429–440.
Lichter PR, Musch DC, Gillespie BW, Guire KE, Janz NK, Wren PA et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology 2001; 108: 1943–1953.
Leske CM, Connell AM, Wu SY, Hyman LG, Schachat AP . Risk factors for open-angle glaucoma. The Barbados Eye Study. Arch Ophthalmol 1995; 113: 918–924.
DesMarchais B, Candal E, Weitzman M, Shields MB . Effect of latanoprost as adjunctive therapy. Can J Ophthalmol 2000; 35: 214–217.
Watson P, Stjernschantz J . Latanoprost Study Group. A six-moth, randomized, double-masked study comparing latanoprost with timolol in open-angle glaucoma and ocular hypertension. Ophthalmology 1996; 103: 126–137.
Simmons ST, Samuelson TW, Alphagan/Xalatan Study Group. Comparison of brimonidine with latanoprost in the adjunct treatment of glaucoma. Clin Ther 2000; 22: 388–399.
O’Connor DJ, Martone JF, Mead A . Additive intraocular pressure lowering effect of various medications with latanoprost. Am J Ophthalmol 2002; 133: 836–837.
Simmons ST, Earl ML, Alphagan/Xalatan Study Group. Three-month comparison of brimonidine and latanoprost as adjunctive therapy in glaucoma and ocular hypertension patients uncontrolled on beta-blockers: tolerance and peak intraocular pressure lowering. Ophthalmology 2002; 109: 307–314.
Kampik A, Arias-Puente A, O’Brart DP, Vuori ML, The European Latanoprost Study Group. Intraocular pressure- lowering effects of latanoprost and brimonidine therapy in patients with open-angle glaucoma or ocular hypertension: a randomized observer-masked multicenter study. J Glaucoma 2002; 11: 90–96.
Higginbotham EJ, Feldman R, Stiles M, Dubiner H, Fixed Combination Investigative Group. Latanoprost and timolol combination therapy vs monotherapy: one-year randomized trial. Arch Ophthalmol 2002; 120: 915–922.
Arici MK, Sayici M, Toker M, Erdogan H, Topalkara A . A short term study of the additive effect of timolol and brimonidine on intraocular pressure. Eye 2002; 16: 39–43.
Clineschmidt CM, Williams RD, Snyder E, Adamsons IA, The Dorzolamide-Timolol Combination Study Group. A randomized trial in patients inadequately controlled with timolol alone comparing the dorzolamide–timolol combination to monotherapy with timolol or dorzolamide. Ophthalmology 1998; 105: 1952–1959.
Strahlman ER, Vogel R, Tipping R, Clineschmidt CM, The Dorzolamide Additivity Study Group. The use of dorzolamide and pilocarpine as adjunctive therapy to timolol in patients with elevated intraocular pressure. Ophthalmology 1996; 103: 1283–1293.
Choudhri S, Wand M, Shields MB . A comparison of dorzolamide-timolol combination versus the concomitant drugs. Am J Ophthalmol 2000; 130: 832–833.
Suzanna Jr R, Nicolela MT, Oga E . Additive effect of latanoprost to the combination of timolol and dorzolamide. J Glaucoma 2000; 9: 183–186.
Hughes E, Spry P, Diamond J . 24-hour monitoring of intraocular pressure in glaucoma management: a retrospective review. J Glaucoma 2003; 12: 232–236.
Sacca SC, Rolando M, Marletta A, Macri A, Cerqueti P, Ciurlo G . Fluctuations of intraocular pressure during the day in open-angle glaucoma, normal-tension glaucoma and normal subjects. Ophthalmologica 1998; 212: 115–119.
Wilensky JT, Gieser DK, Dietsche ML, Mori MT, Zeimer R . Individual variability in the diurnal intraocular pressure curve. Ophthalmology 1993; 100: 940–944.
David R, Zangwill L, Briscoe D, Dagan M, Yagev R, Yassur Y . Diurnal intraocular pressure variations: an analysis of 690 diurnal curves. Br J Ophthalmol 1992; 76: 280–283.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is presented at the annual meeting of the American Academy of Ophthalmology, Orlando, FL, October 2002.
Rights and permissions
About this article
Cite this article
Akman, A., Cetinkaya, A., Akova, Y. et al. Comparison of additional intraocular pressure-lowering effects of latanoprost vs brimonidine in primary open-angle glaucoma patients with intraocular pressure uncontrolled by timolol–dorzolamide combination. Eye 19, 145–151 (2005). https://doi.org/10.1038/sj.eye.6701428
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701428
Keywords
This article is cited by
-
Brimonidine prevents neurodegeneration in a mouse model of normal tension glaucoma
Cell Death & Disease (2014)