Abstract
Background:
Between 1979 and 2001, an analysis of cancer survival in young people in England, aged 13 to 24 years, showed overall improvements. However, for some diagnostic groups, little or no increases were observed. The aim of this study was to analyse the regional distribution of cancer survival in teenagers and young adults in England in order to identify patterns and potential for improvements at a regional scale.
Methods:
We examined geographical and temporal patterns in relative survival in cancer patients aged 13–24 years in England during the time period 1979–2001. Cancer cases were grouped according to an internationally recognised morphology-based diagnostic scheme.
Results:
For most diagnostic groups, there was little variation in survival between regions, except for testicular germ cell tumours (P=0.006) and colorectal carcinoma (P=0.002). For certain diagnostic groups, the temporal pattern in survival differed between regions. However, in regions that showed poor survival during the early part of the study period, greatest improvements were observed in groups such as acute lymphoid leukaemia, acute myeloid leukaemia, testicular tumours and melanoma.
Conclusion:
In conclusion, there was a reduction in the differences in survival between regions during the study period.
Similar content being viewed by others
Main
In the United Kingdom, cancer in teenagers and young adults (TYAs) aged 13–24 years is a major cause of both morbidity and mortality in this age range. In 2005, just under 1700 newly diagnosed cases in young people aged 15–24 years were registered in England alone (Office for National Statistics, 2008). Overall and for specific types of tumours, the geographical distribution of cancer incidence in TYAs was reported to show considerable differences between English regions, which may provide important clues for aetiology and potential for disease prevention (Alston et al, 2007). The assessment of regional variations in cancer incidence and survival is essential for efficient service planning.
Between 1979 and 2001, cancer survival in young people aged 13–24 years has improved over time in England (Birch et al, 2008). However, for some diagnostic groups, little or no improvements were seen. In addition, unlike cancers in older adults, most of the cancers predominant in this age range showed no association between survival and socioeconomic deprivation (Coleman et al, 1999; Quinn et al, 2005; Birch et al, 2008). In older adults, regional variations in survival have been reported for cancers diagnosed during 1971–1990, particularly in the earlier years (Coleman et al, 1999; Quinn et al, 2005). No comparable study has been carried out specifically in TYA cancer.
The aim of this study was to characterise the distribution of TYA cancer survival in England by Government Office Region (GOR) over time in order to provide baseline data at a regional scale and identify potential for improvements. Such a study is timely, given the impending implementation of national guidance on management of cancer in young people aimed at improving outcomes (National Collaboration Centre for Cancer, 2005).
Methods
Patients diagnosed with any neoplasm, aged 13–24 years, in England during the period 1979–2001 (followed up to 31 December 2003) were included in this study. National cancer registration data on individual eligible cases were supplied by the National Cancer Intelligence Centre, Office for National Statistics, London. Data items provided included date of birth, diagnosis and follow-up, gender, histological type and primary site of cancer, GOR of residence, vital status and the Townsend deprivation index (TDI) score (Townsend et al, 1998) for census ward of residence of the patient at the time of diagnosis. Cases diagnosed from 1979 to 1995 were allocated 1991 census ward TDIs and those from 1996 to 2001 were allocated 2001 census ward TDIs. The relationship with TDI was analysed by grouping census wards into quintiles, such that the expected incidence for all cancers across England was the same in each quintile. The quintiles were ranked from 1 to 5, wherein 1 represented the most affluent and 5 the most deprived (Alston et al, 2007). The TDI score is thus standardised within each census.
Cases with vital status unknown, that is, patient record not traced at the National Health Service Central Register, were excluded from analysis, as were cases with a survival time of zero, that is, patients who were diagnosed and who died on the same day or postmortem diagnosis. These exclusion criteria were similar to those applied by Coleman et al (1999) in their publication. Cases lost to follow-up, for example, patients who emigrated, were included up to the date at which they were last known to be alive. The number of cases excluded for these reasons represented ∼4% of all eligible cases.
For cases registered from 1979 to 1994, cancer diagnoses were coded according to the International Classification of Diseases for Oncology, first edition (ICD-O1) (World Health Organization, 1976), and the ninth revision of the International Classification of Diseases (ICD 9) (World Health Organization, 1977). For cases registered between 1995 and 2001, diagnoses were coded according to ICD-O, second edition (ICD-O2) (Percy et al, 1990), and ICD tenth revision (ICD 10) (World Health Organization, 1992).
Cancer cases in 13–24-year olds were grouped according to the morphology-based diagnostic scheme described by Birch et al (2002). All diagnostic groups with <500 patients alive at least 1 day after diagnosis were excluded. The cancer groups included comprise acute lymphoid leukaemia (ALL), acute myeloid leukaemia (AML), non-Hodgkin's lymphoma (NHL), Hodgkin's lymphoma (HL), tumours of the central nervous system (CNS), osteosarcoma and Ewing tumour, soft tissue sarcomas (STSs), testicular germ cell tumours (GCTs), melanoma and carcinoma of ovary, cervix, colon and rectum.
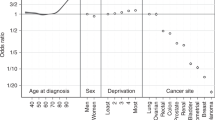
Five-year relative survival in each diagnostic group was calculated by dividing observed survival by expected survival among comparable groups in the general population. The 5-year expected survival was derived from age-, sex-, year- and socioeconomic-specific national mortality rates for England (Coleman et al, 1999). Relative survival by GOR was examined using Poisson regression, as described by Dickman et al (2004). Four time periods (1979–84, 1985–89, 1990–95 and 1996–01) were defined, so that each one of them had an approximately equal number of incident cases. Geographical variations were modelled with random effects and the significance of variability was assessed using a likelihood ratio test statistic, after taking into account sex, age, time period and a quadratic follow-up temporal trend. Residual geographical variability after taking into account a trend in Townsend score quintiles was similarly assessed.
The significance level was set at 5%. Statistical analyses were performed using Stata v. 9.2 (StataCorp, 2005) and the software R (R Development Core Team, 2006).
Results
Survival time was available for 33 274 (96%) out of 34 670 potential eligible patients. The total number of patients belonging to diagnostic groups of insufficient size, and thus excluded from the analysis, was 5204.
Between 1979 and 2001, statistically significant geographical variations in survival were seen for testicular GCTs (P=0.006) and colorectal carcinoma (P=0.002) (Table 1). Geographical variability was marginally significant for NHL (P=0.045) (Table 1). However, the residual geographical variability for the latter was not significant after considering a trend by socioeconomic deprivation (TDI). For all other groups, there was no significant evidence of differences in survival by GOR in the overall time period between 1979 and 2001.
Between 1979 and 2001, 5-year relative survival for patients with ALL increased from 41% to 55% overall (P<0.001) (Figure 1). However, for individual regions, significant increases over time in survival occurred only in North East, Yorkshire and Humber and South West regions . Each of these regions had a lower survival for ALL than did England as a whole in the earliest time period but a higher survival in the latest time period. The highest increase was seen in North East, 30% in 1979–84 and 69% in 1996–2001 (the highest level among regions in this time period).
Five-year relative survival (%) of patients diagnosed with cancer at age 13–24 years in England, between 1979 and 2001, by region and time period. The P-value for time trend is reported in brackets. A, North East; B, North West; D, Yorkshire and Humber; E, East Midlands; F, West Midlands; G, East; H, London; J, South East; K, South West; ALL, acute lymphoid leukaemia; AML, acute myeloid leukaemia; NHL, non-Hodgkin's lymphoma; HL, Hodgkin's lymphoma.  1979–1984,
1979–1984,  1985–1989,
1985–1989,  1990–1995,
1990–1995,  1996–2001.
1996–2001.
The relative survival of patients with AML across England increased from 30% in 1979–84 to 50% in 1996–2001 (P<0.001) (Figure 1). Significant upward temporal trends in AML survival were seen in North West, East Midlands, West Midlands, East, South East and South West regions. East and West Midlands were also the regions in which AML survival showed the steepest increase over time. These two regions showed the lowest survival in the earliest time period. In North West, East and South West regions, patients with AML had a survival of 60% in 1996–2001, the highest in this time period.
Overall, patients with NHL experienced a 55% survival in the time period between 1979 and 1984, increasing to 71% in 1996–2001 (P<0.001) (Figure 1). A significant increase in survival was seen in Yorkshire and Humber, West Midlands, South East and South West regions. For these GORs, the average rate of change in survival over time differed from that of the other GORs (P<0.001). In North East, North West, East Midlands and East regions, as well as in London, relative survival did not increase significantly. These regions, with the exception of London, had survival equal to or greater than the national average in 1979–84, but equal to or lower than the national average in 1996–2001. The average number of patients diagnosed with NHL in the first and last time period was, respectively, 38 and 55 per GOR.
The relative survival of patients with HL increased from 85% in 1979–84 to 93% in 1996–2001 (P<0.001) (Figure 1). However, the temporal pattern differed between regions. For Yorkshire and Humber and East regions, the rate of increase in survival over time was greater than that for the other regions (P<0.001). For North East, North West, London and South West regions, there was no evidence of increase in survival over time, but each of these regions showed equal or higher survival from HL than did England during the earliest period.
Five-year relative survival for CNS tumours in England was 68% in 1979–84, increasing to 72% in the following period and to 74% in 1996–2001 (P<0.001) (Figure 2). Survival in North East and North West regions increased from 65% in 1979–84 to around 80% in 1996–2001. These regions, together with South East and South West, showed on an average, a rate of increase in survival greater than that of the other GORs (P=.01). In contrast 5-year survival of CNS patients in London did not vary significantly over time (P=0.08).
Five-year relative survival (%) of patients diagnosed with cancer at age 13–24 years in England, between 1979 and 2001, by region and time period. The P-value for time trend is reported in brackets. A, North East; B, North West; D, Yorkshire and Humber; E, East Midlands; F, West Midlands; G, East; H, London; J, South East; K, South West; CNS, central nervous system; GCTs, germ cell tumours.  1979–1984,
1979–1984,  1985–1989,
1985–1989,  1990–1995,
1990–1995,  1996–2001.
1996–2001.
Overall, relative survival for patients with testicular GCT increased from 84% to 96% between the first and last time period (P<0.001) (Figure 2). North West, Yorkshire and Humber, East Midlands, South East and South West regions had the most rapid increases over time in survival, but from lower starting points than many other regions.
Survival of patients diagnosed with melanoma between 1979 and 2001 in England increased from 75% in the first time period to 90% in the last time period (P<0.001) (Figure 2).
Regions of the North East, North West, Yorkshire and Humber and West Midlands, in which the 5-year survival rate from melanoma was below the national average in 1979–84, had the greatest increases over time (Figure 2). In contrast, survival in East Midlands, East, London and South West regions did not vary significantly between 1979–84 and 1996–2001. However, for the East, survival was consistently high throughout the four time periods.
Patients diagnosed with osteosarcoma in England between 1979 and 1984 had a 5-year relative survival of 41%, which increased to 49% between 1996 and 2001 (P=0.003) (Figure 3). None of the GORs, with the exception of the North East, showed a significant variation in survival over time. The average number of incident cases diagnosed in the first and last period was, respectively, 36 and 28 per GOR.
Five-year relative survival (%) of patients diagnosed with cancer at age 13–24 years in England, between 1979 and 2001, by region and time period. The P-value for time trend is reported in brackets. A, North East; B, North West; D, Yorkshire and Humber; E, East Midlands; F, West Midlands; G, East; H, London; J, South East; K, South West; STSs, soft tissue sarcomas.  1979–1984,
1979–1984,  1985–1989,
1985–1989,  1990–1995,
1990–1995,  1996–2001.
1996–2001.
Patients diagnosed with Ewing sarcoma in England between 1979 and 1984 had a 5-year relative survival equal to 29%, which increased to 46% between 1996 and 2001 (P=0.001) (Figure 3). Such an increase was mostly led by the North West region, with relative survivals equal to 24% in the first period and 65% in the last period.
Five-year relative survival for STS patients did not vary significantly over time between 1979 and 2001 (P=0.31) (Figure 3). However, West Midlands had a positive trend, increasing from 47% in the first time period to 69% in the last time period, at a rate significantly different from the rest of England (P=0.03).
The relative survival of patients with carcinoma of the ovary, cervix and colorectum increased overall between 1979–84 and 1996–2001 (P=0.02) (Figure 4). However, at the regional level, a significant increase in survival over time only occurred in the North West region for cervical and colorectal carcinoma.
Five-year relative survival (%) of patients diagnosed with carcinoma at age 13–24 years in England, between 1979 and 2001, by region and time period. The P-value for time trend is reported in brackets. A, North East; B, North West; D, Yorkshire and Humber; E, East Midlands; F, West Midlands; G, East; H, London; J, South East; K, South West.  1979–1984,
1979–1984,  1985–1989,
1985–1989,  1990–1995,
1990–1995,  1996–2001.
1996–2001.
Discussion
This study presents an analysis of the geographical and temporal distribution of relative survival from cancers that characterise TYAs in the age range of 13–24 years at the population level, using national data over a 23-year span. Factors including age, gender, time period and socioeconomic deprivation were taken into account. We found significant regional variations in relative survival for testicular GCTs and colorectal carcinoma. For several diagnostic groups under study, trends over time did not follow the same pattern regionally.
Quinn et al (2001) reported differences in survival by region for adult patients (15 years and over) diagnosed between 1986 and 1990. However, the TYA age group was not analysed separately and, furthermore, data were presented by ICD site and not by morphological diagnosis.
In a recent study based on present data, Birch et al (2008) analysed trends in survival by demographic groups and time periods at the national level. Overall, survival among TYAs with cancer has improved during the period 1979–2001 (Birch et al, 2008). This study also showed that for most cancers, there was no association between deprivation and survival but for leukaemias and carcinomas (mainly colorectal and head and neck carcinomas), there was a trend of poorer survival with increasing deprivation. However, in a separate study, we showed significant variations in the incidence of many TYA cancers by region and by deprivation (Alston et al, 2007). The question of possible variations in survival by geographical region therefore arises. Other previous studies of survival from cancer in TYAs deal with cases at the national level (Gatta et al, 2003; Steliarova-Foucher et al, 2004) or in several states in the United States combined (Bleyer et al, 2006). Furthermore, in those studies, different age ranges and/or time periods were considered. No previous studies have addressed survival patterns at the regional level within countries.
For many common adult onset cancers (breast, lung, colon and rectum), there exists an association between lifestyle factors such as tobacco smoking or poor diet and socioeconomic deprivation. The geographical variations in incidence of malignancies that are aetiologically linked to such factors are often the result of different levels of deprivation in different areas (Quinn et al, 2001). Marked differences in survival between 1971 and 1995, according to deprivation category, were observed for many of the major cancers at older ages, but such differences were not present for childhood cancers (Coleman et al, 1999).
In this study, the results show that for some diagnostic groups, variations in survival between regions cannot be entirely attributed to socioeconomic differentials, insofar as the latter are fully reflected by the Townsend score. Although lifestyle factors may have a role in this, other factors such as access to medical healthcare, referral patterns and clinical management should be considered and investigated (Birch et al, 2008).
Improvements in survival from ALL were seen in England overall, but the pattern by time period varied between regions, with significant increases seen in only three regions. The overall 5-year survival of 55% in England in the most recent time period is considerably less than the comparable figure of 83% for children (Stiller, 2007). Acute lymphoid leukaemia in adults has a worse prognosis than childhood ALL and there seems to be biological differences (Moorman et al, 2007). However, there is evidence that adolescents with ALL have a better outcome when treated on a paediatric protocol rather than an adult protocol (Ramanujachar et al, 2007). Some of the differences in survival trends between regions may be accounted for by referral patterns and proportions of TYA cases treated by paediatric and adult haematologists. The implementation of national guidance on management of TYAs with cancer should ensure a uniform approach to treatment with use of the most appropriate protocols.
Considerable improvements in survival over time concerned the group of testicular GCTs (Birch et al, 2008). Our results show that the 5-year relative survival in patients with testicular GCTs shows geographical variability after considering the deprivation index. However, rapid increases in survival between 1979 and 2001 have occurred, particularly in regions with poorer survival originally, so that in the most recent time period, all regions show survivals close to the national average.
Although for individual sites carcinomas are rare in TYAs, collectively, carcinomas form over 16% of all TYA cancers and form the second largest main group after lymphomas (Alston et al, 2007). Birch et al (2008) found a significant association between TDI and survival for some carcinomas, particularly colorectal and head and neck tumours. We observed substantial geographical differences in survival from colorectal carcinoma, which can be attributed only in part to a trend by socioeconomic deprivation. However, in the most recent time period, Figure 4 shows less regional variability in survival, although the numbers of cases in any single region and time period are small. This result raises the question as to what extent improvements in socioeconomic conditions and delivery of existing treatments affected survival during the study period rather than development and delivery of new treatments. Given the strong relationship between survival of patients with colorectal carcinoma and TDI score of residence (Birch et al, 2008), we can speculate that improvements in access to and delivery of existing treatment may have had a role in improving survival. However, because of the limitations of the currently available data, no specific analyses to address this question are possible. Nevertheless, new initiatives through the National Cancer Intelligence Network may make this possible in the future.
In conclusion, we analysed geographical patterns in cancer survival among TYAs on the basis of national data sets covering 23 years and more than 28 000 incident cases. Our results show that for most diagnostic groups, there is little variation in survival between regions. Analyses by time period show a general tendency for reduction in the differences between regions over time, with greatest improvements in those regions that showed poor survival during the early part of the study period. There has been a levelling up of survival rates across the country. The data also indicate that in those groups in which there has been little improvement in recent years (for example, bone and STSs), the problem is national and not because of poor performing regions. In cases in which regional variations are observed, the role of age-appropriate protocols and treatment in specialist units has to be established. Implementation of national guidance on management of young people with cancer in specified regional Principal Treatment Centres will, it is hoped, lead to improvements in outcome (National Collaboration Centre for Cancer, 2005). This study provides data on a regional basis with which treatment outcome in these developing regional specialist TYA cancer units and outcome of clinical trials can be compared. These outcomes will be of interest to specialists in adolescent oncology in other countries that are currently in the process of setting up specialist services for TYAs with cancer (Bleyer et al, 2007).
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alston RD, Rowan S, Eden TOB, Moran A, Birch JM (2007) Cancer incidence patterns by region and socioeconomic deprivation in teenagers and young adults in England. Br J Cancer 96: 1760–1766
Birch JM, Alston RD, Kelsey AM, Quinn MJ, Babb P, McNally RJQ (2002) Classification and incidence of cancers in adolescents and young adults in England 1979–1997. Br J Cancer 87: 1267–1274
Birch JM, Pang D, Alston RD, Rowan S, Geraci M, Moran A, Eden TOB (2008) Survival from cancer in teenagers and young adults in England, 1979–2003. Br J Cancer 99: 830–835
Bleyer A, Budd T, Montello M (2007) Older adolescents and young adults with cancer and clinical trials: lack of participation and progress in North America. In: Bleyer A, Barr RD (eds) Cancer in Adolescents and Young Adults Chapter 5, pp 71–81
Bleyer A, O’Leary M, Barr R, Ries LAG (eds) (2006) Cancer Epidemiology in Older Adolescents and Young Adults 15 to 29 Years of Age, Including SEER Incidence and Survival: 1975–2000. NIH Pub. No. 06–5767 National Cancer Institute: Brethesda, MD
Coleman MP, Babb P, Damiecki P, Grosclaude P, Honjo S, Jones J, Knerer G, Pitard A, Quinn MJ, Sloggett A, De Stavola BL (1999) Cancer Survival Trends in England and Wales, 1971–1995: Deprivation and NHS Region. Series SMPS No 61 The Stationary Office: London
Dickman PW, Sloggett A, Hills M, Hakulinen T (2004) Regression models for relative survival. Stat Med 23: 51–64
Gatta G, Capocaccia R, De Angelis R, Stiller C, Coebergh JW, the EUROCARE Working Group (2003) Cancer survival in European adolescents and young adults. Eur J Cancer 39: 2600–2610
Moorman AV, Harrison CJ, Buck GA, Richards SM, Secker-Walker LM, Martineau M, Vance GH, Cherry AM, Higgins RR, Fielding AK, Foroni L, Paietta E, Tallman MS, Litzow MR, Wiernik PH, Rowe JM, Goldstone AH, Dewald GW, Adult Leukaemia Working Party, Medical Research Council/National Cancer Research Institute (2007) Karyotype is an independent prognostic factor in adult acute lymphoblastic leukemia (ALL): analysis of cytogenetic data from patients treated on the Medical Research Council (MRC) UKALLXII/Eastern Cooperative Oncology Group (ECOG) 2993 trial. Blood 109: 3189–3197
National Collaboration Centre for Cancer (2005) Guidance on Cancer Services, Improving Outcomes in Children and Young People with Cancer. National Institute for Health and Clinical Excellence: London. ISBN: 1–84629–067–8
Office for National Statistics (2008) Cancer Statistics, Registrations. Registrations of Cancer Diagnosed in 2005, England. Series MB1 no 36 Office for National Statistics: London
Percy C, Van Holten V, Muir CS (1990) International Classification of Diseases for Oncology: ICD-O. 2nd edn. World Health Organization: Geneva
Quinn MJ, Babb P, Brock A, Kirby L, Jones J (2001) Cancer Trends in England and Wales 1950–1999. Studies on Medical and Population Subjects No. 66. The Stationery Office: London
Quinn MJ, Wood H, Cooper N, Rowan S (eds) (2005) Cancer Atlas of the United Kingdom and Ireland 1991–2000. Studies on Medical and Population Subjects No. 68. Palgrave Macmillan: London
R Development Core Team (2006) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria. ISBN 3–900051–07–0, http://www.R-project.org
Ramanujachar R, Richards S, Hann I, Goldstone A, Mitchell C, Vora A, Rowe J, Webb D (2007) Adolescents with acute lymphoblastic leukaemia: outcome on UK national paediatric (ALL97) and adult (UKALLXII/E2993) trials. Pediatr Blood Cancer 48: 254–261
StataCorp (2005) Stata Statistical Software: Release 9. StataCorp LP: College Station, TX
Steliarova-Foucher E, Stiller C, Kaatsch P, Berrino F, Coebergh JW, Lacour B, Parkin M (2004) Geographical patterns and time trends of cancer incidence and survival among children and adolescents in Europe since 1970s (the ACCIS project): an epidemiological study. Lancet 364: 2097–2105
Stiller C (ed) (2007) Childhood Cancer in Britain: Incidence, Survival, Mortality. Oxford University Press: Oxford, UK
Townsend P, Phillimore P, Beattie A (1998) Health Deprivation, Inequality and the North. Croom-Helm: London
World Health Organization (1976) ICD-O: International Classification of Diseases for Oncology. World Health Organization: Geneva
World Health Organization (1977) International Statistical Classification of Diseases, Injuries and Causes of Death. 9th revision World Health Organization: Geneva
World Health Organization (1992) International Statistical Classification of Diseases and Related Health Problems. 10th revision World Health Organization: Geneva
Acknowledgements
M Geraci, RD Alston and JM Birch are funded by Cancer Research UK. RS Arora is funded by a grant from the Paediatric Endowment Fund Christie Hospital NHS Foundation Trust and from the Teenage Cancer Trust. This study was partly funded by CLIC Sargent. Tim Eden was Teenage Cancer Trust Professor of Teenage and Young Adult Cancer, University of Manchester during this study, Jillian Birch is Cancer Research UK Professorial Fellow, University of Manchester. Census output is Crown copyright and is reproduced with the permission of the Controller of HMSO and the Queen's Printer for Scotland. Cancer Research UK Survival Group (2006). strel computer program, version 1.2.7 and life tables for cancer survival analysis. Downloaded from www.lshtm.ac.uk/ncdeu/cancersurvival/tools on 10th November 2008. Non-Communicable Disease Epidemiology Unit, London School of Hygiene & Tropical Medicine, UK.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Geraci, M., Eden, T., Alston, R. et al. Geographical and temporal distribution of cancer survival in teenagers and young adults in England. Br J Cancer 101, 1939–1945 (2009). https://doi.org/10.1038/sj.bjc.6605410
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605410