Abstract
Increased expression of tumour-associated trypsin inhibitor (TATI) in tumour tissue and/or serum has been associated with poor survival in various cancer forms. Moreover, a proinvasive function of TATI has been shown in colon cancer cell lines. In this study, we have examined the prognostic significance of tumour-specific TATI expression in colorectal cancer, assessed by immunohistochemistry (IHC) on tissue microarrays (TMAs) with tumour specimens from two independent patient cohorts. Kaplan–Meier analysis and Cox proportional hazards modelling were used to estimate time to recurrence, disease-free survival and overall survival. In both cohorts, a high (>50% of tumour cells) TATI expression was an independent predictor of a significantly shorter overall survival. In cohort II, in multivariate analysis including age, gender, disease stage, differentiation grade, vascular invasion and carcinoembryonal antigen (CEA), high TATI expression was associated with a significantly decreased overall survival (HR=1.82; 95% CI=1.19–2.79) and disease-free survival (HR=1.56; 95% CI=1.05–2.32) in curatively treated patients. Moreover, there was an increased risk for liver metastasis in both cohorts that remained significant in multivariate analysis in cohort II (HR=2.85; 95% CI=1.43–5.66). In conclusion, high TATI expression is associated with liver metastasis and is an independent predictor of poor prognosis in patients with colorectal cancer.
Similar content being viewed by others
Main
Tumour invasion of surrounding tissue requires degradation of the basal membrane and extracellular matrix (Kohn and Liotta, 1995). Matrix metalloproteinases (MMPs) and matrix serine proteases (MSPs) are two groups of proteolytic enzymes that are proposed to be the most important for tumour progression (Stenman, 1990; Mignatti and Rifkin, 1993; Nelson et al, 2000). Trypsin is a potent MSP protease that hydrolyses a variety of proteins and activates other MSPs and MMPs (Koivunen et al, 1991; Yamamoto et al, 2003). Four identical isoforms of trypsinogen have been described in human tissue and these isoforms are homologous (Emi et al, 1986; Tani et al, 1990; Wiegand et al, 1993; Koshikawa et al, 1998). In the gastrointestinal tract, the main function of the trypsin is to break down dietary proteins. It is expressed by many tumours and also plays a significant role in tumour invasion (Koivunen et al, 1991; Moilanen et al, 2003; Paju et al, 2004). Immunohistochemical (IHC) expression of trypsin in colorectal cancer (CRC) correlates with unfavourable clinicopathological characteristics and shortened survival (Yamamoto et al, 2003).
The tumour-associated trypsin inhibitor (TATI), synonymous with serine protease inhibitor Kazal type 1 (SPINK1) and pancreatic secretory trypsin inhibitor (PSTI; Huhtala et al, 1982), balances and inhibits trypsin specifically and may thus reduce tissue destruction (Wiksten et al, 2005). It is also a weak inhibitor of other serine proteinases (Fritz et al, 1967; Huhtala et al, 1982; Turpeinen et al, 1988). In vitro, TATI increases cell migration and plays a role in tissue repair (Stenman, 1990). It has been suggested that expression of TATI and trypsin is balanced in normal tissue, but this balance could be disrupted during tumour progression (Hotakainen et al, 2006).
Tumour-associated trypsin inhibitor expression has been associated with impaired survival in several forms of cancer (Stenman, 2002; Paju et al, 2004; Lee et al, 2007) but not in gastric cancer, where it is believed to have a natural function of protecting the mucosa from proteolytic degradation (Freeman et al, 1990; Playford et al, 1991; Marchbank et al, 1996, 1998; Wiksten et al, 2005). However, in most cancer forms, TATI and trypsin are coexpressed and show similar and adverse associations to disease outcome (Paju et al, 2004; Hotakainen et al, 2006).
Elevated serum TATI has been shown to be a prognostic marker for ovarian cancer (Venesmaa et al, 1994, 1998), kidney cancer (Paju et al, 2001) and bladder cancer (Kelloniemi et al, 2003). In ovarian carcinoma, TATI expression, both in tissue and serum, has been associated with a shorter survival and high tissue expression was the most useful prognostic factor (Huhtala et al, 1982; Paju et al, 2004).
Coexpression of trypsin and TATI has previously been found at both mRNA and protein level in CRC (Solakidi et al, 2003), but we are not aware of any published reports on the association between expression of TATI in tumour tissue and survival in patients with CRC. However, a recent study showed that TATI is associated with autocrine induction and metastasis in colon cancer cells (Gouyer et al, 2008).
The purpose of this study was to analyse the association between IHC expression of TATI in CRC and clinicopathological parameters, its recurrence and survival.
Patients and methods
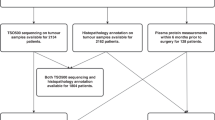
Cohort I
Cohort I includes 118 cases of CRC, 61 (52%) women and 57 (48%) men, diagnosed at the Department of Pathology, Malmö University Hospital, between January 1999 and March 2002. This cohort was designed as an initial screening cohort for tissue biomarkers of potential diagnostic or prognostic relevance. Therefore, the cases were selected to obtain an equal distribution of disease stages I–III, with 35 patients in stage I, 42 patients in stage II, 35 patients in stage III and 6 patients in stage IV. Median age at diagnosis was 75 years (range: 32–88; mean 73), and after a median follow-up of 85 months (0–115) (mean 56), 54 patients (46%) were alive and 64 (54%) were dead. Information on treatment was not available for this cohort. Data on overall survival (OS) were collected from the population register. Approval was obtained from the Ethics committee at the Lund University (cohort I, ref no. 447–07), whereby informed consent was deemed not to be required other than by the opt-out method.
Cohort II
The second cohort, used as a validation cohort, consists of 320 prospectively collected patients undergoing elective surgery for CRC at the Central District Hospital in Västerås, Sweden, between June 2000 and December 2003, 277 (87%) of which were treated surgically with curative intent. Information on cancer recurrence, death and cause of death were obtained by matching with the Regional Oncology Registry and from the hospital records. Median follow-up time was 6 years (4–7) for surviving patients. Recurrent disease was reported for 54 (19%) of curatively treated patients, and 119 (37%) patients died during the study period. Preoperative radiotherapy was given to 84/108 patients with rectal cancer. All patients <75 years with colon cancer stage III (n=36) and 22 of 29 rectal cancer patients as well as some patients with high risk (T4, low differentiation) stage II disease (13/71) received adjuvant chemotherapy. Palliative chemotherapy was given in 23 of 27 patients <75 years with stage IV disease. More than 12 lymph nodes were examined in 224 (70%) of 320 patients and in 96 (73%) of 132 patients with stage II disease. Ethical approval was obtained from the Ethics committee at Uppsala University (cohort II, ref no. 00–001). All patients included in this cohort gave their informed consent for participation in the study.
Tissue microarray (TMA) construction
Tissue microarrays were constructed as described earlier (Kononen et al, 1998). In brief, 2 × 1 mm cores from areas representative of invasive cancer were sampled for each case and mounted in a recipient block using a manual arraying device (MTA-1; Beecher Instruments, Hartland, WI, USA). In addition, a number of samples from normal colonic mucosa, adenomas and lymph node metastases were included in the TMA from cohort II.
Immunohistochemistry
In all, 4 μm sections were dried, deparaffinised, rehydrated, and heat-mediated antigen retrieval was carried out by boiling under pressure in DAKO Target Retrieval Buffer (DAKO, Glostrup, Denmark; pH 9.0). Immunohistochemistry was carried out in the DAKO Techmate 500 system (DAKO) using a monoclonal anti-TATI antibody (6E8) diluted 1 : 500 as described earlier (Osman et al, 1993).
Tumour-associated trypsin inhibitor was expressed in the cytoplasm and the percentage of positive tumour cells in each core was estimated and assigned values of 0, 5 or multiples of 10%. The intensity of the expression was assigned a value of 0, 1, 2 or 3. In cases where both tissue cores were present, both the score from the core with the highest percentage of positive cells/‘best score’ (Tomlins et al, 2008) and mean score were denoted. Samples from adjacent normal mucosa and adenomas were scored in the same fashion. The IHC staining was evaluated independently by two of the authors (AG and KJ) who were blinded to clinical and outcome data. Scoring differences were discussed to reach consensus.
Statistics
The χ2 and Spearman's correlation tests were used for comparison of TATI expression and relevant patient and tumour characteristics. The Kaplan–Meier method and log-rank test were used to estimate disease-free survival (DFS), time to recurrence (TTR) and OS. End points were defined as recommended by Punt et al (2007); OS was measured from the date of surgery to the date of death; the observations were censored at the end of the study period (1 November 2008). Disease-free survival was measured in curatively treated patients from the date of surgery to the date of second cancer, recurrence or death from any cause. Time to recurrence was measured in curatively treated patients from the date of surgery to the date of locoregional recurrence, distant metastases or to the date of death in CRC; the observations were censored at the end of the study period or at the date of death in non-CRC. A Cox proportional hazards model/hazard ratios (HRs) was used for estimation of relative risks in both univariate and multivariate analyses, and adjusted for age, gender, disease stage, differentiation grade and lymphatic or vascular invasion. All statistical tests were two-sided and P-values <0.05 were considered significant. Calculations were carried out with either SPSS15.0 (SPSS Inc., Chicago, IL, USA) or Statistica 7 (Stat Soft Inc., Tulsa, OK, USA).
Results
Tumour-associated trypsin inhibitor expression in normal colonic mucosa, cancer and metastases
Tumour-associated trypsin inhibitor was expressed in the cytoplasm both in the normal mucosa, the primary cancer and metastases (Figure 1). The overall staining distribution (best score) in cancer cells was similar in cohorts I and II (data not shown). There was no obvious heterogeneity in TATI expression between the paired tissue cores from each individual tumour, that is, no difference between mean and best scores (data not shown). Using cohort I as a test cohort to construct a dichotomised variable for defining TATI high and low cases, we compared different thresholds (1, 25, 50 and 75% positive cells) with respect to their impact on survival. High TATI expression was associated with a shorter survival for all cutoffs tested (data not shown), but the most significant separation was observed at 50%. The staining intensity had no impact on survival. By this approach, the proportion of cases with low and high expression was similar in both cohorts with 24 cases (20.3%) in cohort I and 66 cases (19.9%) in cohort II exhibiting high TATI expression. No differences were seen in the expression of TATI best score in different preoperative radiation therapy groups in rectal cancer patients (data not shown).
Correlation between TATI expression and clinicopathological parameters
The distribution of tumours with low and high TATI expression in relation to tumour and patient characteristics is shown in Table 1. In cohort I, high TATI expression was only significantly associated with age (P=0.008). In cohort II, lower expression was seen with advanced tumour (T), lymph node (N) and disease stage, also visualised in Figure 2. There was a significant association between a lower TATI fraction (0–50%) and higher tumour stage (P=018). In cohort II, TATI was expressed in 89 (86%) of 104 samples from benign mucosa and in 12 (18%) of 67 lymph node metastases. When right and left colonic tumours were compared with left colonic cancers, defined as tumours in the splenic flexure to the rectum, a trend for lower expression of TATI best score was seen in left colonic cancers. Tumour-associated trypsin inhibitor best score ⩽50 was seen in 141 of 188 (0.75%) left colonic cancers compared with 100 out of 121 (0.83%) right colonic cancers (P=0.113, χ2-test).
Tumour-associated trypsin inhibitor (TATI) best score for fraction of immunoreactivity in primary tumour tissue from patients with colorectal cancer and its relation to tumour (T) (A), disease (B) and to lymph node (N) stages (C). Boxes indicate mean (small central box) and mean ±1 s.e. (larger box). Whiskers indicate mean ±1.96 times s.e. Kruskal–Wallis test was used for comparison.
Tumour-associated trypsin inhibitor expression in relation to survival and metastasis
In cohort I, tumours with more than 50% TATI-expressing tumour cells had a significantly shorter OS (HR=2.42; 95% CI= 1.38–4.26, P=0.002). This association remained significant in multivariate analysis after adjustment for established clinicopathological parameters (HR=1.80; 95% CI= 0.99–3.27; P=0.05). There was a significant association with the appearance of liver metastases (HR=3.97; 95% CI=0.99–15.88; P=0.05) in univariate, but not in multivariate analysis, including age, gender, disease stage, differentiation grade and vascular invasion (HR= 3.69; 95% CI= 0.87–15.67; P=0.08).
In cohort II, patients with high TATI score had a significantly shorter OS and DFS, compared to those with low fraction, in curatively treated patients (Figure 3). This association remained significant in multivariate analysis, including adjustment for age, gender, disease stage, differentiation grade, vascular invasion and carcinoembryonal antigen (CEA; Table 2).
Furthermore, patients with a high fraction of TATI-positive cells in primary tumour tissue tended to have increased risk of cancer recurrence (Figure 4a) and an increased risk of liver metastasis (Figure 4b), and this was significant also in multivariate analysis (HR=2.85; 95% CI=1.43–5.66).
As mentioned earlier most of the patients (n=40) with metastatic disease at diagnosis had TATI best score <50% (n=34; 85%) (Figure 2b); however, there was a trend towards more synchronous liver metastases in those with TATI >50% (5 of 6; 83%) compared with TATI<50% in primary tumour tissue (16 of 34; 47%; P=0.101).
Discussion
Our results show that tumour-specific TATI expression is associated with shorter survival of patients with CRC. These findings were observed in two independent patient cohorts. These results are in line with recent in vitro data (Gouyer et al, 2008). Furthermore, in both cohorts, there was a significant association between TATI expression and metastasis to the liver and in cohort II; representing a larger number of patients, this association remained significant in multivariate analysis.
An elevated TATI expression has, with few exceptions, been associated with a more aggressive tumour phenotype and poor clinical outcome in several forms of cancer (Paju et al, 2004, 2007; Hotakainen et al, 2006; Lee et al, 2007; Tomlins et al, 2008). Given the frequently observed coexpression of TATI and trypsin in cancer, it can be hypothesised that increased levels of TATI reflect a simultaneous elevation of trypsin and, hence, increased propensity of the tumour cells to invade and spread. However, in prostate cancer, TATI may actually be an independent mediator of aggressive disease (Tomlins et al, 2008). The mechanisms by which TATI is associated with aggressive cancer need to be further explored. Although protease inhibitors could be expected to control the invasion-promoting effects of various proteases, there is increasing evidence showing that overexpression of various protease inhibitors results in enhanced malignancy of cancer cells. For instance, a number of studies have shown that increased serum concentrations of tissue inhibitor of metalloproteinases 1 (TIMP-1), a major inhibitor of metalloproteinases, often is associated with a poor clinical outcome in various cancer forms (Ree et al, 1997; Holten-Andersen et al, 1999; Schrohl et al, 2004; Yukawa et al, 2004). Similarly, another protease inhibitor, the plasminogen activator inhibitor 1 (PAI-1) has been shown to be associated with poor prognosis in breast cancer (Grondahl-Hansen et al, 1993), lung cancer (Pedersen et al, 1994) and CRC (Nielsen et al, 1998). Overexpression of secretory leukocyte protease inhibitor (SLPI), which also inhibits trypsin, increases the malignant properties of lung cancer cell lines (Devoogdt et al, 2003).
So far, the mechanisms by which TATI is associated with tumour aggressiveness are unknown, but because no TATI receptor has been identified and TATI is a very specific trypsin inhibitor (Turpeinen et al, 1988), it is tempting to speculate that TATI exerts its effect through modulation of trypsin activity. Trypsin may affect various cellular functions, for example, proliferation and invasion, by activating protease-activated receptors (PARs) and especially PAR-2 (Soreide, 2008).
The complexity of the interplay and diverging actions of proteases and their inhibitors in human cancer is further illustrated by the fact that experimental targeted therapies with synthetic proteinase inhibitors have not proven effective and have, in some trials, even elicited poorer results and more adverse effects than standard chemotherapy (Kruger et al, 2001; Coussens et al, 2002; Moore et al, 2003).
Furthermore, treatment with the synthetic MMP inhibitor, batimastat, has been shown to make breast cancer and lymphoma cells more prone to form liver metastases in mouse models (Kruger et al, 2001). In addition, batimastat treatment induced the expression of MMPs, metastasis-promoting and angiogenesis factors in the liver (Kruger et al, 2001). This is particularly interesting in the light of our findings of a significant association between TATI expression and metastasis to the liver. A link between TATI and metastatic disease has also been shown in CRC cell lines and downregulation of TATI resulted in a concomitant downregulation of several metastasis-associated genes (Gouyer et al, 2008).
Another explanation for the more malignant phenotype associated with TATI overexpression could be that an increased expression of proteinase inhibitors may help the tumour cells evade the immune response and make them better equipped for survival and distant spread. It has been suggested that the increased expression of proteinases associated with malignant disease may, to a large extent, be because of an immunological host response induced by the tumour (Nelson et al, 2000). For instance, in breast cancer cells, stromelysin-3, a proteinase from the MMPs family, has been found exclusively in stromal cells surrounding neoplastic invasive cells, but not non-invasive cells (Basset et al, 1990).
Tumour-associated trypsin inhibitor is believed to play a protective role in both gastric mucosa (Wiksten et al, 2005) and colonic mucosa (Soreide et al, 2006) and in accordance with these findings, we found that TATI was highly expressed in non-malignant colonic mucosa. It should, however, be pointed out that the non-malignant mucosa studied here had been sampled from areas adjacent to the tumour and, hence, it cannot be ascertained whether this truly reflects TATI levels in normal mucosa from healthy individuals.
In cohort II, there was a significant association between lower TATI expression and a more advanced tumour stage. Such an association has previously been found in a small cohort of bladder cancer (Hotakainen et al, 2006) where high TATI expression tended to be associated with a better prognosis. There was also a trend, however non-significant, towards a lower TATI expression in more advanced disease stages; but the proportion of synchronous liver metastases was higher in cases with TATI >50%.
Further studies are warranted to investigate which cutoffs are the most appropriate for defining high versus low TATI expression. In this study, we first analysed TATI expression in a retrospectively collected cohort and established a dichotomised variable with the best prognostic separation. This cutoff also proved to have a prognostic impact in a second cohort with prospectively collected tumour samples, in which the risk of sampling bias should be reduced. In neither of the cohorts did the staining intensity have any impact on prognosis, only the fraction of positive cells. As the staining intensity is often more easily affected by the variability of sample preparation, particularly the time of fixation in formalin, the fraction of positive cells might be a more reliable parameter with better reproducibility. Both parameters should, however, be taken into account in future studies evaluating TATI expression by IHC, and automated image analysis may be a more objective approach (Brennan et al, 2008; Rexhepaj et al, 2008). Other cutoffs, with or without taking the staining intensity into account, have been used in earlier studies on other cancer forms, (Paju et al, 2004; Tomlins et al, 2008).
It will also be of interest to investigate the utility of serum TATI as a prognostic marker and predictor of liver metastasis in CRC. However, TATI as well as CEA in serum has not proven to correlate with the absence or presence of metastases or monitoring of disease after surgery (Catarino and Conde, 1991; Pasanen et al, 1995).
In conclusion, our results show that tumour-specific overexpression of TATI contributes to a poor prognosis in CRC and seems to promote a tumour phenotype with predilection of liver metastasis in vivo. Thus, therapeutic targeting of TATI could prove to be an efficient strategy in the management of high-risk CRC patients.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Basset P, Bellocq JP, Wolf C, Stoll I, Hutin P, Limacher JM, Podhajcer OL, Chenard MP, Rio MC, Chambon P (1990) A novel metalloproteinase gene specifically expressed in stromal cells of breast carcinomas. Nature 348: 699–704
Brennan DJ, Rexhepaj E, O'Brien SL, McSherry E, O'Connor DP, Fagan A, Culhane AC, Higgins DG, Jirstrom K, Millikan RC, Landberg G, Duffy MJ, Hewitt SM, Gallagher WM (2008) Altered cytoplasmic-to-nuclear ratio of survivin is a prognostic indicator in breast cancer. Clin Cancer Res 14: 2681–2689
Catarino M, Conde R (1991) Tumor-associated trypsin inhibitor (TATI) in patients with colorectal carcinoma. A critical comparison with CEA. Scand J Clin Lab Invest 207: 43–46
Coussens LM, Fingleton B, Matrisian LM (2002) Matrix metalloproteinase inhibitors and cancer: trials and tribulations. Science (NY) 295: 2387–2392
Devoogdt N, Hassanzadeh Ghassabeh G, Zhang J, Brys L, De Baetselier P, Revets H (2003) Secretory leukocyte protease inhibitor promotes the tumorigenic and metastatic potential of cancer cells. Proc Natl Acad Sci USA 100: 5778–5782
Emi M, Nakamura Y, Ogawa M, Yamamoto T, Nishide T, Mori T, Matsubara K (1986) Cloning, characterization and nucleotide sequences of two cDNAs encoding human pancreatic trypsinogens. Gene 41: 305–310
Freeman TC, Playford RJ, Quinn C, Beardshall K, Poulter L, Young J, Calam J (1990) Pancreatic secretory trypsin inhibitor in gastrointestinal mucosa and gastric juice. Gut 31: 1318–1323
Fritz H, Hutzel M, Werle E (1967) (On protease inhibitors, VI. On the identity of the protease inhibitor from rat liver with the trypsin-kallikren-inhibitor (Trasylol)). Hoppe-Seyler's Zeitschrift fur physiologische Chemie 348: 950
Gouyer V, Fontaine D, Dumont P, de Wever O, Fontayne-Devaud H, Leteurtre E, Truant S, Delacour D, Drobecq H, Kerckaert JP, de Launoit Y, Bracke M, Gespach C, Desseyn JL, Huet G (2008) Autocrine induction of invasion and metastasis by tumor-associated trypsin inhibitor in human colon cancer cells. Oncogene 27: 4024–4033
Grondahl-Hansen J, Christensen IJ, Rosenquist C, Brunner N, Mouridsen HT, Dano K, Blichert-Toft M (1993) High levels of urokinase-type plasminogen activator and its inhibitor PAI-1 in cytosolic extracts of breast carcinomas are associated with poor prognosis. Cancer Res 53: 2513–2521
Holten-Andersen MN, Murphy G, Nielsen HJ, Pedersen AN, Christensen IJ, Hoyer-Hansen G, Brunner N, Stephens RW (1999) Quantitation of TIMP-1 in plasma of healthy blood donors and patients with advanced cancer. Br J Cancer 80: 495–503
Hotakainen K, Bjartell A, Sankila A, Jarvinen R, Paju A, Rintala E, Haglund C, Stenman UH (2006) Differential expression of trypsinogen and tumor-associated trypsin inhibitor (TATI) in bladder cancer. Int J Oncol 28: 95–101
Huhtala ML, Pesonen K, Kalkkinen N, Stenman UH (1982) Purification and characterization of a tumor-associated trypsin inhibitor from the urine of a patient with ovarian cancer. J Biol Chem 257: 13713–13716
Kelloniemi E, Rintala E, Finne P, Stenman UH (2003) Tumor-associated trypsin inhibitor as a prognostic factor during follow-up of bladder cancer. Urology 62: 249–253
Kohn EC, Liotta LA (1995) Molecular insights into cancer invasion: strategies for prevention and intervention. Cancer Res 55: 1856–1862
Koivunen E, Ristimaki A, Itkonen O, Osman S, Vuento M, Stenman UH (1991) Tumor-associated trypsin participates in cancer cell-mediated degradation of extracellular matrix. Cancer Res 51: 2107–2112
Kononen J, Bubendorf L, Kallioniemi A, Barlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP (1998) Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med 4: 844–847
Koshikawa N, Hasegawa S, Nagashima Y, Mitsuhashi K, Tsubota Y, Miyata S, Miyagi Y, Yasumitsu H, Miyazaki K (1998) Expression of trypsin by epithelial cells of various tissues, leukocytes, and neurons in human and mouse. Am J Pathol 153: 937–944
Kruger A, Soeltl R, Sopov I, Kopitz C, Arlt M, Magdolen V, Harbeck N, Gansbacher B, Schmitt M (2001) Hydroxamate-type matrix metalloproteinase inhibitor batimastat promotes liver metastasis. Cancer Res 61: 1272–1275
Lee YC, Pan HW, Peng SY, Lai PL, Kuo WS, Ou YH, Hsu HC (2007) Overexpression of tumour-associated trypsin inhibitor (TATI) enhances tumour growth and is associated with portal vein invasion, early recurrence and a stage-independent prognostic factor of hepatocellular carcinoma. Eur J Cancer 43: 736–744
Marchbank T, Chinery R, Hanby AM, Poulsom R, Elia G, Playford RJ (1996) Distribution and expression of pancreatic secretory trypsin inhibitor and its possible role in epithelial restitution. Am J Pathol 148: 715–722
Marchbank T, Freeman TC, Playford RJ (1998) Human pancreatic secretory trypsin inhibitor. Distribution, actions and possible role in mucosal integrity and repair. Digestion 59: 167–174
Mignatti P, Rifkin DB (1993) Biology and biochemistry of proteinases in tumor invasion. Physiol Rev 73: 161–195
Moilanen M, Sorsa T, Stenman M, Nyberg P, Lindy O, Vesterinen J, Paju A, Konttinen YT, Stenman UH, Salo T (2003) Tumor-associated trypsinogen-2 (trypsinogen-2) activates procollagenases (MMP-1, -8, -13) and stromelysin-1 (MMP-3) and degrades type I collagen. Biochemistry 42: 5414–5420
Moore MJ, Hamm J, Dancey J, Eisenberg PD, Dagenais M, Fields A, Hagan K, Greenberg B, Colwell B, Zee B, Tu D, Ottaway J, Humphrey R, Seymour L (2003) Comparison of gemcitabine versus the matrix metalloproteinase inhibitor BAY 12-9566 in patients with advanced or metastatic adenocarcinoma of the pancreas: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 21: 3296–3302
Nelson AR, Fingleton B, Rothenberg ML, Matrisian LM (2000) Matrix metalloproteinases: biologic activity and clinical implications. J Clin Oncol 18: 1135–1149
Nielsen HJ, Pappot H, Christensen IJ, Brunner N, Thorlacius-Ussing O, Moesgaard F, Dano K, Grondahl-Hansen J (1998) Association between plasma concentrations of plasminogen activator inhibitor-1 and survival in patients with colorectal cancer. BMJ (Clin Res Ed) 316: 829–830
Osman S, Turpeinen U, Itkonen O, Stenman UH (1993) Optimization of a time-resolved immunofluorometric assay for tumor-associated trypsin inhibitor (TATI) using the streptavidin-biotin system. J Immunol Methods 161: 97–106
Paju A, Hotakainen K, Cao Y, Laurila T, Gadaleanu V, Hemminki A, Stenman UH, Bjartell A (2007) Increased expression of tumor-associated trypsin inhibitor, TATI, in prostate cancer and in androgen-independent 22Rv1 cells. Eur Urol 52: 1670–1679
Paju A, Jacobsen J, Rasmuson T, Stenman UH, Ljungberg B (2001) Tumor associated trypsin inhibitor as a prognostic factor in renal cell carcinoma. J Urol 165: 959–962
Paju A, Vartiainen J, Haglund C, Itkonen O, von Boguslawski K, Leminen A, Wahlstrom T, Stenman UH (2004) Expression of trypsinogen-1, trypsinogen-2, and tumor-associated trypsin inhibitor in ovarian cancer: prognostic study on tissue and serum. Clin Cancer Res 10: 4761–4768
Pasanen P, Eskelinen M, Kulju A, Penttila I, Janatuinen E, Alhava E (1995) Tumour-associated trypsin inhibitor (TATI) in patients with colorectal cancer: a comparison with CEA, CA 50 and CA 242. Scand J Clin Lab Invest 55: 119–124
Pedersen H, Grondahl-Hansen J, Francis D, Osterlind K, Hansen HH, Dano K, Brunner N (1994) Urokinase and plasminogen activator inhibitor type 1 in pulmonary adenocarcinoma. Cancer Res 54: 120–123
Playford RJ, Batten JJ, Freeman TC, Beardshall K, Vesey DA, Fenn GC, Baron JH, Calam J (1991) Gastric output of pancreatic secretory trypsin inhibitor is increased by misoprostol. Gut 32: 1396–1400
Punt CJ, Buyse M, Köhne CH, Hohenberger P, Labianca R, Schmoll HJ, Påhlman L, Sobrero A, Douillard JY (2007) Endpoints in Adjuvant Treatment Trials: A Systematic Review of the Literature in Colon Cancer and Proposed Definitions for Future Trials. J Natl Cancer Inst 99: 998–1003
Ree AH, Florenes VA, Berg JP, Maelandsmo GM, Nesland JM, Fodstad O (1997) High levels of messenger RNAs for tissue inhibitors of metalloproteinases (TIMP-1 and TIMP-2) in primary breast carcinomas are associated with development of distant metastases. Clin Cancer Res 3: 1623–1628
Rexhepaj E, Brennan DJ, Holloway P, Kay EW, McCann AH, Landberg G, Duffy MJ, Jirstrom K, Gallagher WM (2008) Novel image analysis approach for quantifying expression of nuclear proteins assessed by immunohistochemistry: application to measurement of oestrogen and progesterone receptor levels in breast cancer. Breast Cancer Res 10: R89
Schrohl AS, Holten-Andersen MN, Peters HA, Look MP, Meijer-van Gelder ME, Klijn JG, Brunner N, Foekens JA (2004) Tumor tissue levels of tissue inhibitor of metalloproteinase-1 as a prognostic marker in primary breast cancer. Clin Cancer Res 10: 2289–2298
Solakidi S, Tiniakos DG, Petraki K, Stathopoulos GP, Markaki I, Androulakis G, Sekeris CE (2003) Co-expression of trypsin and tumour-associated trypsin inhibitor (TATI) in colorectal adenocarcinomas. Histol Histopathol 18: 1181–1188
Soreide K (2008) Proteinase-activated receptor 2 (PAR-2) in gastrointestinal and pancreatic pathophysiology, inflammation and neoplasia. Scand J Gastroenterol 43: 902–909
Soreide K, Janssen EA, Korner H, Baak JP (2006) Trypsin in colorectal cancer: molecular biological mechanisms of proliferation, invasion, and metastasis. J Pathol 209: 147–156
Stenman UH (1990) Tumour-associated trypsin inhibitor and tumour-associated trypsin. Scand J Clin Lab Invest 201: 93–101
Stenman UH (2002) Tumor-associated trypsin inhibitor. Clin Chem 48: 1206–1209
Tani T, Kawashima I, Mita K, Takiguchi Y (1990) Nucleotide sequence of the human pancreatic trypsinogen III cDNA. Nucleic Acids Res 18: 1631
Tomlins SA, Rhodes DR, Yu J, Varambally S, Mehra R, Perner S, Demichelis F, Helgeson BE, Laxman B, Morris DS, Cao Q, Cao X, Andren O, Fall K, Johnson L, Wei JT, Shah RB, Al-Ahmadie H, Eastham JA, Eggener SE, Fine SW, Hotakainen K, Stenman UH, Tsodikov A, Gerald WL, Lilja H, Reuter VE, Kantoff PW, Scardino PT, Rubin MA, Bjartell AS, Chinnaiyan AM (2008) The role of SPINK1 in ETS rearrangement-negative prostate cancers. Cancer cell 13: 519–528
Turpeinen U, Koivunen E, Stenman UH (1988) Reaction of a tumour-associated trypsin inhibitor with serine proteinases associated with coagulation and tumour invasion. Biochem J 254: 911–914
Venesmaa P, Lehtovirta P, Stenman UH, Leminen A, Forss M, Ylikorkala O (1994) Tumour-associated trypsin inhibitor (TATI): comparison with CA125 as a preoperative prognostic indicator in advanced ovarian cancer. Br J Cancer 70: 1188–1190
Venesmaa P, Stenman UH, Forss M, Leminen A, Lehtovirta P, Vartiainen J, Paavonen J (1998) Pre-operative serum level of tumour-associated trypsin inhibitor and residual tumour size as prognostic indicators in Stage III epithelial ovarian cancer. Br J Obstet Gynaecol 105: 508–511
Wiegand U, Corbach S, Minn A, Kang J, Muller-Hill B (1993) Cloning of the cDNA encoding human brain trypsinogen and characterization of its product. Gene 136: 167–175
Wiksten JP, Lundin J, Nordling S, Kokkola A, Stenman UH, Haglund C (2005) High tissue expression of tumour-associated trypsin inhibitor (TATI) associates with a more favourable prognosis in gastric cancer. Histopathology 46: 380–388
Yamamoto H, Iku S, Adachi Y, Imsumran A, Taniguchi H, Nosho K, Min Y, Horiuchi S, Yoshida M, Itoh F, Imai K (2003) Association of trypsin expression with tumour progression and matrilysin expression in human colorectal cancer. J Pathol 199: 176–184
Yukawa N, Yoshikawa T, Akaike M, Sugimasa Y, Takemiya S, Yanoma S, Imada T, Noguchi Y (2004) Prognostic impact of tissue inhibitor of matrix metalloproteinase-1 in plasma of patients with colorectal cancer. Anticancer Res 24: 2101–2105
Acknowledgements
We thank Elise Nilsson and Kristina Lövgren for excellent technical assistance. This study was supported by grants from Swegene (AG and KJ), the Knut and Alice Wallenberg Foundation (KJ and FP), the Swedish Cancer Society (BG, AB and KJ), the Swedish Research Council (AB), Gunnar Nilsson's Cancer Foundation (AB and KJ), the Research fund of the County of Västmanland Against Cancer (HB), Lions Cancer Foundation Uppsala (HB) and by the Research funds of Malmö University Hospital (AB and KJ).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Gaber, A., Johansson, M., Stenman, UH. et al. High expression of tumour-associated trypsin inhibitor correlates with liver metastasis and poor prognosis in colorectal cancer. Br J Cancer 100, 1540–1548 (2009). https://doi.org/10.1038/sj.bjc.6605047
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605047
Keywords
This article is cited by
-
Serine protease inhibitor Kazal type 1 (SPINK1) promotes proliferation, migration, invasion and radiation resistance in rectal cancer patients receiving concurrent chemoradiotherapy: a potential target for precision medicine
Human Cell (2022)
-
Nitrogen-doped carbon quantum dots fabricated from cellulolytic enzyme lignin and its application to the determination of cytochrome c and trypsin
Analytical and Bioanalytical Chemistry (2021)
-
Significant association and synergistic adverse prognostic effect of podocalyxin-like protein and epidermal growth factor receptor expression in colorectal cancer
Journal of Translational Medicine (2016)
-
Monitoring the treatment outcome in endometrial cancer patients by CEA and TATI
Tumor Biology (2016)
-
SPINK1 promotes colorectal cancer progression by downregulating Metallothioneins expression
Oncogenesis (2015)