Abstract
In a case–control study using a large UK primary care database, we found that non-steroidal anti-inflammatory drugs had no protective effect against biliary carcinomas (cholangiocarcinoma and gall bladder cancer). Increased risks were observed for cigarette smoking, diabetes, gallstone disease and obesity.
Similar content being viewed by others
Main
Cholangiocarcinoma has a 5-year survival rate of only 20% (Nathan et al, 2007). It is becoming more common in both the UK and the USA. At the same time, the incidence of the other cancer of the biliary epithelium (gall bladder cancer) has declined (West et al, 2006). Risk factors for cholangiocarcinoma include primary sclerosing cholangitis, gallstone disease (Ekbom et al, 1993), HCV infection (Donato et al, 2001), diabetes and obesity (Welzel et al, 2007). Gall bladder cancer has been previously linked with gallstone disease (Serra et al, 1996) and cigarette smoking (Yagyu et al, 2008). It has been suggested that cyclooxygenase (COX) inhibition might have potential for chemoprevention in cholangiocarcinoma as COX-2 expression inhibits apoptosis in cholangiocarcinoma cells (Sirica et al, 2001). We set out to examine the role of the above risk factors in a large UK primary care-based population and, for the first time, to assess whether non-steroidal anti-inflammatory drugs (NSAIDs) protect against cholangiocarcinoma and gall bladder cancer.
Materials and methods
The General Practice Research Database (GPRD) is a large longitudinal primary care database containing the primary care records of more than 8 million patients in the UK. The GPRD data are audited to ensure that at least 95% of medical events and prescriptions are satisfactorily recorded (Walley and Mantgani, 1997) and have been shown to provide results consistent with other UK data sources (Hollowell, 1997).
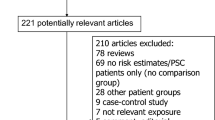
We identified people in the GPRD between 1987 and March 2002 with a recorded diagnosis of cholangiocarcinoma or gall bladder cancer using the Oxford Medical Information System and Read Clinical Classification codes. Cases were categorised into three groups: definite cholangiocarcinoma, definite gall bladder cancer, and a group containing patients who had both types of cancer coded or had codes that could not distinguish between them. The index date for cases was taken as the date of first diagnosis of biliary cancer. A total of 10 controls were matched to each case by GP practice, sex and age (within 5 years of the case). We excluded controls with less than 1 year of exposure data prior to case diagnosis.
Risk factors of interest were history of liver disease (including cirrhosis, hepatitis, primary sclerosing cholangitis, gallstone-related disease) or diabetes, prior NSAID use and lifestyle factors (smoking, alcohol and body mass index (BMI)). Any diagnoses occurring later than 6 months prior to the index date were excluded. Non-steroidal anti-inflammatory drug use was defined as any prescription of a drug listed under section 10.1.1 of the British National Formulary (No. 54). Analyses were repeated with exposure being classified by use at different time points preceding case diagnosis. We also repeated the analysis by excluding prescriptions for aspirin to ascertain the effect of non-aspirin NSAID use. Smoking status and alcohol intake were recorded at 1 year prior to the date of case diagnosis (or closest record prior to this). For alcohol intake, ‘problem drinkers’ were defined as those with a GPRD code indicating alcohol misuse at any time prior to diagnosis. Body mass index was calculated as weight in kg/height in m2. A separate category was created for the smoking, alcohol or BMI variables related to participants who had missing data.
Data were analysed using conditional logistic regression, with results presented as odds ratios (ORs) with 95% confidence intervals (CIs). Results were adjusted a priori for smoking, alcohol and BMI, with NSAID use also adjusted for gallstone disease diagnosis. Analyses were performed using the entire case group, and then separately for cholangiocarcinoma and gall bladder cancer cases. Stata version 10.0 was used for all analyses.
Results
Selection of cases and controls
We identified 611 cases, 372 cholangiocarcinomas, 184 gall bladder cancers and 55 unspecified biliary cancers. In total, 5760 controls were matched to the cases. The median duration of exposure data available prior to the date of case diagnosis was 4.8 years for cases (range 1.0–12.4 years) and 4.4 years for controls (range 1.0–12.5 years). The percentage of male cases was greater for cholangiocarcinoma (48.4%) than for gall bladder cancer (26.1%), whilst the mean age at diagnosis was similar for the two cancer types (71.3 (s.d. 12.0) years vs 72.0 (s.d. 11.1) years).
Chronic liver disease and diabetes
Only small numbers of viral hepatitis (n=3), cirrhosis (n=2) and PSC (n=1) occurred among cholangiocarcinoma cases and none occurred among cases of gall bladder cancer. Only gallstone disease occurred with sufficient frequency to allow appropriate comparison of cases and controls, which was associated with a more than three-fold risk of gall bladder cancer and almost two-fold risk of cholangiocarcinoma (Table 1). The prevalence of diabetes was 8.5% in cases, which was significantly higher than the 5.9% in controls (OR=1.39; 95% CI, 1.01–1.90).
NSAID use
A previous NSAID prescription was received by approximately 50% of both cases and controls, with no significant difference between the groups overall (OR=0.95; 95% CI, 0.80–1.13). In the interval 24–36 months preceding case diagnosis, there was significantly more NSAID use among cholangiocarcinoma cases (OR=1.34); however, in all other time intervals and among gall bladder cases ORs were close to 1 (Table 1). When we repeated this analysis for non-aspirin NSAIDs the findings did not change materially, with a slightly increased risk for cholangiocarcinoma in the 24–36-month period preceding diagnosis (OR=1.32; 95% CI, 1.00–1.75) and ORs closer to 1 in all other instances (data not shown).
BMI, cigarette smoking and alcohol
We found that obese patients (BMI⩾30 kg/m2) had 1.5 times the risk of both cholangiocarcinoma and gall bladder cancer when compared with those with BMI <25 kg/m2 (Table 1). An increased risk was also observed among cigarette smokers, which was significant both among the entire series of cases (OR=1.48) and for the individual cancer types. We found neither current alcohol use nor problem alcohol drinking to be associated with either cancer (Table 1).
Discussion
This is the first epidemiological study to examine the potential for chemoprevention of cholangiocarcinoma by the use of NSAIDs. Cyclooxygenase-2 is overexpressed in cholangiocarcinoma cells (Wu et al, 2002), is involved in apoptosis in these cells (Sirica et al, 2001), and its inhibition by Celecoxib has been shown in vivo to induce apoptosis in them (Wu et al, 2003). Despite this, no benefit from NSAIDS was found among our study group. Protective effects of NSAIDs on other GI tumors have been shown earlier using the same data set and methods similar to those we have used (Langman et al, 2000). A post hoc power calculation showed that our study had 90% power to detect a 25% reduction in risk with previous NSAID use; hence, our negative result was not because of lack of statistical power. One weakness of our study with respect to NSAIDs is that owing to their limited use in the UK there were not enough data to permit us to examine COX-2 inhibitors separately from other NSAIDs. This does not invalidate our results for NSAIDs, but leaves open the possibility that a more selective COX-2 inhibition may have a chemoprotective effect.
Our study confirms a number of earlier-described associations with other risk factors. We have been able to not only confirm the long-recognised association of gallstone disease (OR 2.34), but also reproduce significant associations with smoking (OR 1.48) and obesity (OR 1.58 for comparison of BMI<25 and BMI⩾30). We also found an association with diabetes of a magnitude similar to that reported in a recent publication from the SEER study (Welzel et al, 2007). We did not, however, in contrast to previous research (Shaib et al, 2007), find an association with alcohol intake. Exposure to PSC, cirrhosis or viral hepatitis was very rare within our study, hence greatly limiting our power to examine these factors.
Our results are not susceptible to selection bias as our study is population-based, using all available cases and appropriately selected controls from the same population. Nor, given the prospective recording of exposure data, is it prone to ascertainment bias beyond that because of the increased medical attention to which cases will inevitably be exposed in the run-up to and after their diagnosis. We have attempted to minimise this bias that might affect some of our risk estimates (such as those with diabetes and PSC) by excluding exposures later than 6 months before diagnosis from our analysis. One limitation of our study is that unlike in earlier studies, we are unable to say whether cholangiocarcinoma is intra- or extra-hepatic, nor to access histological or radiological records to validate the diagnosis. We think it unlikely that UK general practitioners would make a diagnosis of cholangiocarcinoma, and so we believe that the diagnoses are as secure as those in UK secondary care. Much of the quoted literature, however, refers specifically to intra-hepatic cholangiocarcinoma; therefore, if the risk factors for carcinogenesis vary by site within the biliary epithelium, this might explain why viral hepatitis and cirrhosis (if they affect intrahepatic more than extrahepatic ducts) occur less frequently in our study when compared with others (Donato et al, 2001).
In summary, this large population-based case–control study of biliary carcinomas has shown no protective effect from NSAIDs. It has, though, confirmed the increased risk of diabetes mellitus and gallstone disease, which earlier studies have found for cholangiocarcinoma, and has provided population-based estimates of the magnitudes of these associations. It has also highlighted the role of PSC, viral hepatitis and cirrhosis, but shows that although cholangiocarcinoma risk may be high in people with these risk factors, they explain little of the disease occurrence.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Donato F, Gelatti U, Tagger A, Favret M, Ribero ML, Callea F, Martelli C, Savio A, Trevisi P, Nardi G (2001) Intrahepatic cholangiocarcinoma and hepatitis C and B virus infection, alcohol intake, and hepatolithiasis: a case–control study in Italy. Cancer Causes Control 12: 959–964
Ekbom A, Hsieh CC, Yuen J, Trichopoulos D, McLaughlin JK, Lan SJ, Adami HO (1993) Risk of extrahepatic bileduct cancer after cholecystectomy. Lancet 342: 1262–1265
Hollowell J (1997) The General Practice Research Database: quality of morbidity data. Popul Trends 87: 36–40
Langman MJ, Cheng KK, Gilman EA, Lancashire RJ (2000) Effect of anti-inflammatory drugs on overall risk of common cancer: case–control study in general practice research database. BMJ 320: 1642–1646
Nathan H, Pawlik TM, Wolfgang CL, Choti MA, Cameron JL, Schulick RD (2007) Trends in survival after surgery for cholangiocarcinoma: a 30-year population-based SEER database analysis. J Gastrointest Surg 11: 1488–1496; discussion 1496–1497
Serra I, Calvo A, Baez S, Yamamoto M, Endoh K, Aranda W (1996) Risk factors for gallbladder cancer – an international collaborative case–control study. Cancer 78: 1515–1516
Shaib YH, El-Serag HB, Nooka AK, Thomas M, Brown TD, Patt YZ, Hassan MM (2007) Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: a hospital-based case–control study. Am J Gastroenterol 102: 1016–1021
Sirica AE, Lai GH, Zhang Z (2001) Biliary cancer growth factor pathways, cyclo-oxygenase-2 and potential therapeutic strategies. J Gastroenterol Hepatol 16: 363–372
Walley T, Mantgani A (1997) The UK General Practice Research Database. Lancet 350: 1097–1099
Welzel TM, Graubard BI, El-Serag HB, Shaib YH, Hsing AW, Davila JA, McGlynn KA (2007) Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: a population-based case–control study. Clin Gastroenterol Hepatol 5: 1221–1228
West J, Wood H, Logan RF, Quinn M, Aithal GP (2006) Trends in the incidence of primary liver and biliary tract cancers in England and Wales 1971–2001. Br J Cancer 94: 1751–1758
Wu GS, Wang JH, Liu ZR, Zou SQ (2002) Expression of cyclooxygenase-1 and -2 in extra-hepatic cholangiocarcinoma. Hepatobiliary Pancreat Dis Int 1: 429–433
Wu GS, Zou SQ, Liu ZR, Tang ZH, Wang JH (2003) Celecoxib inhibits proliferation and induces apoptosis via prostaglandin E2 pathway in human cholangiocarcinoma cell lines. World J Gastroenterol 9: 1302–1306
Yagyu K, Kikuchi S, Obata Y, Lin YS, Ishibashi T, Kurosawa M, Inaba Y, Tamakoshi A (2008) Cigarette smoking, alcohol drinking and the risk of gallbladder cancer death: a prospective cohort study in Japan. Int J Cancer 122: 924–929
Acknowledgements
JW is funded by a National Institute for Health Research Clinician Scientist Fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Grainge, M., West, J., Solaymani-Dodaran, M. et al. The antecedents of biliary cancer: a primary care case–control study in the United Kingdom. Br J Cancer 100, 178–180 (2009). https://doi.org/10.1038/sj.bjc.6604765
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604765
Keywords
This article is cited by
-
Immunology and immunotherapy of cholangiocarcinoma
Nature Reviews Gastroenterology & Hepatology (2023)
-
Evidence-based clinical practice guidelines for cholelithiasis 2021
Journal of Gastroenterology (2023)
-
Clinical Ontologies Improve Case Finding of Primary Biliary Cholangitis in UK Primary and Secondary Care
Digestive Diseases and Sciences (2020)
-
Cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA)
Nature Reviews Gastroenterology & Hepatology (2016)
-
Targeted Therapy in Biliary Tract Cancers
Current Treatment Options in Oncology (2015)