Abstract
Adult body mass index (BMI) has been associated with ovarian cancer risk, but few studies have examined body size earlier in life. We prospectively examined associations of body fatness at ages 5 and 10, BMI at age 18, height, and birthweight with risk of epithelial ovarian cancer in the Nurses' Health Study (NHS: 110 311 women, 735 cases) and Nurses' Health Study II (NHSII: 113 059 women, 137 cases). Cox proportional hazards regression was used to estimate relative risks (RRs) and 95% confidence intervals (CIs). There was a weak inverse association between average body fatness at ages 5 and 10 and risk in the NHS (RR for heaviest vs most lean=0.81, 95% CI: 0.53–1.24, P for trend=0.04) and a nonsignificant positive association in the NHSII (RR=2.09, 95% CI: 0.98–4.48, P for trend=0.10), possibly due to differences in age and menopausal status. Height was positively associated with risk in both cohorts (RR for ⩾1.75 vs <1.6 m=1.43, 95% CI: 1.05–1.96, P for trend=0.001). Body mass index at the age of 18 years and birthweight were not associated with risk. Further research should examine the biological mechanisms underlying the observed associations.
Similar content being viewed by others
Main
Overweight and obesity have been associated with risk of cancer in women (Calle and Kaaks, 2004), but the findings for ovarian cancer are inconclusive. Some epidemiological studies have observed weak to moderate positive associations between adult body mass index (BMI) and ovarian cancer risk; others have found no association (Olsen et al, 2007). One potential explanation is that the timing of overweight and obesity during the lifecourse may be important. Although most studies have examined ovarian cancer risk in relation to recent BMI, studies examining BMI earlier in life, during late adolescence or young adulthood, have observed stronger positive associations (Fairfield et al, 2002; Engeland et al, 2003; Lubin et al, 2003; Anderson et al, 2004). Body fatness during childhood and early adolescence has been associated with breast cancer risk, independent of adult BMI (Berkey et al, 1999; Baer et al, 2005), suggesting that adiposity at young ages may affect risk of hormone-related cancers. Furthermore, there is evidence that height, a marker of early childhood growth and nutrition, is associated with ovarian cancer risk (Rodriguez et al, 2002; Engeland et al, 2003; Schouten et al, 2003, 2008), indicating that early life may be a critical time period for ovarian cancer initiation.
Therefore, we prospectively examined the associations of body size in early life – including body fatness at ages 5 and 10 years, BMI at the age of 18 years, birthweight, and height – with risk of epithelial ovarian cancer among participants in two large cohort studies, the Nurses' Health Study (NHS) and the NHSII.
Materials and methods
Study design and population
The NHS began in 1976 and the NHSII in 1989, when 121 700 and 116 609 US female registered nurses, respectively, completed a mailed questionnaire about their lifestyle factors, health behaviours, and medical histories. Follow-up questionnaires have been sent to participants every 2 years since enrolment. Incident cases of epithelial ovarian cancer were reported on the biennial questionnaires through 2004 (NHS) and 2005 (NHSII). A gynaecologic pathologist reviewed the pathology reports and medical records to confirm the diagnosis and identify histological type, subtype, morphology, and stage (Tworoger et al, 2008).
Assessment of body size in early life and other covariates
Participants recalled their body fatness (also called ‘somatotype’) at ages 5 and 10 years using a nine-level figure drawing, where level 1 represents the most lean and level 9 represents the most overweight (Figure 1) (Stunkard et al, 1983). Among participants in the Third Harvard Growth Study, Pearsons correlations between recalled somatotype and measured BMI were 0.60 for the age of 5 years and 0.70 for the age of 10 years (Must et al, 1993). We averaged each participant's reported somatotypes at ages 5 and 10 years to obtain an estimate of childhood body fatness. The levels 5 and above were combined in the analysis because of small numbers of participants in these categories.
Women reported their weight at the age of 18 years and their current height at enrolment; these were used to calculate BMI at the age of 18 years in kg m−2. In a sample of NHSII participants, the Spearmans correlation between recalled and recorded weight at the age of 18 years was 0.87, and for BMI at the age of 18 years was 0.84 (Troy et al, 1995). Categories for BMI at the age of 18 years and height were chosen based on their distributions and previously used cutpoints.
Participants recalled their birthweight as <5.5, 5.5–6.9, 7.0–8.4, 8.5–9.9, and ⩾10 pounds. The two highest categories (8.5 pounds and higher) were combined in the analysis to increase power. In a NHSII validation study (Troy et al, 1996), the correlation between self-reported birthweight and that obtained from state birth records was 0.74.
Age and other covariates were assessed on the questionnaires throughout the study.
Statistical analysis
Participants contributed person-time from baseline (the questionnaire year that the exposure of interest was assessed) until the date of ovarian cancer diagnosis, report of other cancer (except nonmelanoma skin cancer), death, or 31 May 2004 (NHS) or 31 May 2005 (NHSII), whichever occurred sooner. We excluded women reporting a previous diagnosis of cancer except nonmelanoma skin cancer and those with a history of bilateral oophorectomy or pelvic irradiation. For analyses focusing on each individual body size measure, we excluded women who were missing data for that measure. The years of assessment, numbers of eligible participants and cases, and total numbers of person-years available for each analysis are shown in Table 1.
Cox proportional hazards models stratified by age in months and 2-year questionnaire cycle were used to estimate relative risks (RRs) and 95% confidence intervals (CIs), adjusting for ovarian cancer risk factors. Tests for linear trend were conducted by including each body size measure in a model either as an ordinal variable (childhood body fatness, birthweight) or as a continuous variable with values equal to the category medians (BMI at the age of 18 years, height).
We first conducted the analyses within the NHS and NHSII separately. We then evaluated heterogeneity in the estimates by cohort (DerSimonian and Laird, 1986). We used interaction terms and stratified analyses to assess effect modification by menopausal status, age, and common ovarian cancer risk factors. Separate models were run for invasive cases alone and by histological type (serous/poorly-differentiated, endometrioid, mucinous).
Results
Most adult characteristics were not associated with early life body size (Table 2). In both cohorts, greater body fatness during childhood and BMI at the age of 18 years were associated with earlier menarche and higher current BMI, and taller height was associated with later menarche. In the NHS, women with greater childhood body fatness and taller women were slightly younger at baseline, and women who were heavier in childhood and at the age of 18 years were slightly less likely to use postmenopausal hormones. In the NHSII, women with greater childhood body fatness, greater BMI at the age of 18 years, and taller height were less likely to be parous, and those with greater BMI at the age of 18 years also had shorter duration of oral contraceptive use.
In the NHS, greater body fatness at ages 5 and 10 years were associated with decreased risk of ovarian cancer (Table 3), although the association was only significant for the age of 10 years (RR for level ⩾5 vs level 1=0.69, 95% CI: 0.48–0.99, P for trend=0.01). Averaging ages 5 and 10 years, the RR for childhood body fatness level ⩾5 compared to level 1 was 0.81 (95% CI: 0.53–1.24, P for trend=0.04). In contrast, there was some suggestion of a positive association for average childhood body fatness in the NHSII (RR for level ⩾5 vs level 1=2.09, 95% CI: 0.98–4.48), although this was not statistically significant (P for trend=0.10) (Table 3). The associations for body fatness at ages 5 and 10 years individually and average childhood body fatness were significantly different by cohort (P for heterogeneity=0.03, 0.01, and 0.01, respectively). Body mass index at the age of 18 years was not significantly associated with risk in either cohort.
One major difference between the NHS and NHSII cohorts is the menopausal status of participants when childhood body size was assessed (NHS: 32% premenopausal in 1988, NHSII: 99% premenopausal in 1989). To explore whether this could explain the observed difference in the association of childhood body fatness with risk, we combined the data from both cohorts and stratified by menopausal status in the cycle before diagnosis (Table 4). There was some suggestion of a weak positive association between childhood body fatness and risk of ovarian cancer in premenopausal women (pooled RR for level ⩾5 vs level 1=1.38, 95% CI: 0.70–2.71, P for trend=0.92) and a weak inverse association in postmenopausal women (comparable RR=0.85, 95% CI: 0.54–1.31, P for trend=0.09), although neither these nor the interaction with menopausal status (P=0.37) were statistically significant. Results for BMI at the age of 18 years were similar in premenopausal women, but there was no evidence of an inverse association in postmenopausal women (P for interaction=0.11).
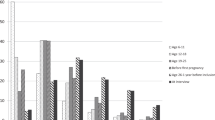
Alternatively, the observed variation in the associations for childhood body fatness could be explained by age differences between participants in the two cohorts (NHS: mean age=54.3 in 1988, NHSII: mean age=34.3 in 1989); therefore, we conducted a preliminary analysis combining both cohorts and stratifying by age, while adjusting for menopausal status. There were nonsignificant positive associations between childhood body fatness and ovarian cancer risk in women less than the age of 50 years (pooled RR for level ⩾5 vs level 1=1.77, 95% CI: 0.85–3.69, P for trend=0.39) and in women between the ages 50 and 59 years (comparable RR=1.30, 95% CI: 0.64–2.65, P for trend=0.34), whereas the association was inverse in women at the age of 60 years and older (comparable RR=0.67, 95% CI: 0.39–1.16, P for trend=0.01). The interaction between childhood body fatness and age was statistically significant (P=0.001). When we jointly stratified by age and menopausal status, the positive association between childhood body fatness and ovarian cancer risk appeared stronger in premenopausal women under the age of 45 years (pooled RR for childhood body fatness level ⩾5 vs level 1=2.51, 95% CI: 0.94–6.73) than in those at the age of 45 years and older (comparable RR=0.83, 95% CI: 0.30–2.28). Conversely, the inverse association in postmenopausal women was stronger among those at the age of 60 years and older (pooled RR for childhood body fatness level ⩾5 vs level 1=0.67, 95% CI: 0.39–1.16) than in those younger than the age of 60 years (comparable RR=1.63, 95% CI: 0.73–3.66).
Additional adjustment for current BMI as a continuous variable had virtually no impact on the childhood body fatness associations in the NHS or for postmenopausal women overall (data not shown). However, the positive association for childhood body fatness in the NHSII and in premenopausal women was attenuated when including current BMI (RR for childhood body fatness level ⩾5 vs level 1 in premenopausal women=1.23, 95% CI: 0.61–2.47, P for trend=0.73). Adjustment for age at menarche had no substantial impact on the associations (data not shown).
Height was positively associated with ovarian cancer risk in both cohorts (pooled RR for ⩾1.75 vs <1.6 m=1.43, 95% CI: 1.05–1.96, P for trend=0.001), and the test for heterogeneity was not significant (P=0.22); however, the association appeared stronger in the NHSII (comparable RR=2.35, 95% CI: 1.19–4.63, P for trend=0.01) than in the NHS (comparable RR=1.27, 95% CI: 0.88–1.82, P for trend=0.01) (Table 5). The positive association was slightly stronger among premenopausal than postmenopausal women, although there were no significant interactions with menopausal status or age (data not shown). Birthweight was not significantly associated with risk of ovarian cancer in either cohort.
The observed associations for body size in early life were similar for invasive cases alone and by histological type, although these analyses were limited by small case numbers. No significant interactions were observed between any of the body size measures and parity, oral contraceptive use, postmenopausal hormone use, or family history of breast or ovarian cancer (data not shown).
Discussion
Results from this study indicate that body size in early life may be related to the risk of epithelial ovarian cancer. Body fatness during childhood was associated with ovarian cancer risk, although the association differed by cohort; greater body fatness at ages 5 and 10 years was associated with a slightly lower risk among NHS women, but a suggestion of an increased risk among NHSII women. These differences could be explained by differences in the menopausal status or age of participants. Body mass index at the age of 18 years and birthweight were not associated with risk; however, height was positively associated with risk.
To our knowledge, this is the first study to investigate the association of childhood fatness with ovarian cancer risk. Previous studies have examined the relation between overweight and obesity in adulthood and ovarian cancer risk or mortality, with mixed results (Olsen et al, 2007). One possible reason for these inconsistencies pertains to the timing of body size assessment. Several studies have observed stronger associations for BMI in adolescence or young adulthood than for recent BMI (Engeland et al, 2003; Anderson et al, 2004). The results from our study indicate that body size at even younger ages may be an important predictor of ovarian cancer risk.
A second potential explanation is that the relation between body size at young ages and ovarian cancer risk may differ by menopausal status or age. In a pooled analysis of 12 cohorts, BMI at baseline was not associated with risk overall or among postmenopausal women, but there was a positive association in premenopausal women (Schouten et al, 2008). Our findings also suggest that the positive association for childhood body fatness may be limited to premenopausal women, particularly younger premenopausal women.
However, our findings of different associations for childhood body fatness with ovarian cancer risk by cohort could be partially due to a cohort effect. Greater childhood body fatness among women in the NHS may have been determined by different factors than in the NHSII. Chance could also explain our results, given that the observed associations for childhood body fatness were modest and the trends were only marginally significant. However, strong associations between childhood body fatness and risk of breast cancer have been observed in previous studies, suggesting that it may predict the risk of hormone-related cancers in women. Further, previous studies have observed significant associations of both adolescent and adult BMI with ovarian cancer risk, lending plausibility to our findings.
The associations of body size in childhood with ovarian cancer risk could be mediated through endogenous hormones (Risch, 1998; Lukanova and Kaaks, 2005), although epidemiological data on the relation of endogenous hormones with ovarian cancer risk are sparse and inconsistent (Eliassen and Hankinson, 2008). Obesity during adolescence has been associated with polycystic ovary syndrome (PCOS), which is characterised by elevated levels of luteinising hormone (LH) and possibly increased risk of ovarian cancer (Schildkraut et al, 1996). Paradoxically, although, adiposity in premenopausal women without PCOS (Cramer et al, 2002) and postmenopausal women (Malacara et al, 2001) has been related to lower LH levels. Obesity in pre-adolescent and adolescent girls is associated with hyperinsulinemia and increased production of androgens (Stoll, 1998), which may be related to ovarian cancer risk (Risch, 1998). Also, lower levels of progesterone could increase risk (Risch, 1998). Obesity in adolescence is associated with increased risk of ovulatory infertility in adulthood (Stoll, 1998), which leads to decreased progesterone levels, and infertility has been associated with a modest increase in ovarian cancer risk (Tworoger et al, 2007a). Clearly, more research is needed to clarify the biological mechanisms underlying these associations.
The observed positive association between height and ovarian cancer risk is consistent with results from previous studies in several populations (Rodriguez et al, 2002; Engeland et al, 2003; Schouten et al, 2003, 2008). Interestingly, the positive association for height has been restricted to or stronger among younger or premenopausal women (Kuper et al, 2002; Lukanova et al, 2002; Engeland et al, 2003; Schouten et al, 2008), consistent with our findings. It is also possible that the difference in the observed association for height in the NHS and the NHSII could be due to a cohort effect.
Despite consistency across epidemiological studies, the biological mechanisms explaining the observed associations for height are unclear. Adult height may be a marker for genetic factors or of energy intake, caloric restriction, or exposure to sex and growth hormones in early life (Schouten et al, 2003). Height consistently has been associated with risk of other cancers (Gunnell et al, 2001), and the growth hormone/insulin-like growth factor (IGF) axis is a potential pathway (Gunnell, 2000). However, epidemiological studies of circulating levels of IGF and ovarian cancer risk are inconclusive (Tworoger et al, 2007b), and thus other mechanisms may be involved.
There are almost no epidemiological data on the relation of birthweight to risk of ovarian cancer. In a small retrospective medical record review, birthweight was not associated with mortality from ovarian cancer, but greater weight gain in the first year of life was associated with increased mortality (Barker et al, 1995). The investigators hypothesised that patterns of gonadotropin release are established in utero and during infancy, and that this could influence ovarian cancer pathogenesis later in life. A population-based case–control study found no overall association between birthweight and ovarian cancer risk, although among women younger than the age of 55 years, there was a decreased risk of ovarian cancer for those who weighed <5.5 pounds at birth compared to those who weighed 5.5–9 pounds (Rossing et al, 2008). Our findings do not support an association of birthweight with ovarian cancer risk, although this should be confirmed in other populations.
Our study has several limitations. Although we combined data from two large cohort studies, we had limited power to examine interactions or variation by histological type. Another limitation is the reliance on recall of body size in early life. Important strengths of our study include its large sample size, its prospective design, the confirmation of ovarian cancer cases, and the detailed information on menopausal status and ovarian cancer risk factors.
In summary, this study suggests that body fatness during childhood and adult height may be related to ovarian cancer risk, and that these associations may vary by menopausal status or age. This is the first study to examine the associations of body fatness during childhood with ovarian cancer risk, and it is one of the largest, most comprehensive studies of the other body size measures to date. Further research should confirm these findings in other populations as well as examine the underlying biological mechanisms.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Anderson JP, Ross JA, Folsom AR (2004) Anthropometric variables, physical activity, and incidence of ovarian cancer: The Iowa Women's Health Study. Cancer 100: 1515–1521
Baer HJ, Colditz GA, Rosner B, Michels KB, Rich-Edwards JW, Hunter DJ, Willett WC (2005) Body fatness during childhood and adolescence and incidence of breast cancer in premenopausal women: a prospective cohort study. Breast Cancer Res 7: R314–R325
Barker DJ, Winter PD, Osmond C, Phillips DI, Sultan HY (1995) Weight gain in infancy and cancer of the ovary. Lancet 345: 1087–1088
Berkey CS, Frazier AL, Gardner JD, Colditz GA (1999) Adolescence and breast carcinoma risk. Cancer 85: 2400–2409
Calle EE, Kaaks R (2004) Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 4: 579–591
Cramer DW, Barbieri RL, Fraer AR, Harlow BL (2002) Determinants of early follicular phase gonadotrophin and estradiol concentrations in women of late reproductive age. Hum Reprod 17: 221–227
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188
Eliassen AH, Hankinson SE (2008) Endogenous hormone levels and risk of breast, endometrial and ovarian cancers: prospective studies. Adv Exp Med Biol 630: 148–165
Engeland A, Tretli S, Bjorge T (2003) Height, body mass index, and ovarian cancer: a follow-up of 1.1 million Norwegian women. J Natl Cancer Inst 95: 1244–1248
Fairfield KM, Willett WC, Rosner BA, Manson JE, Speizer FE, Hankinson SE (2002) Obesity, weight gain, and ovarian cancer. Obstet Gynecol 100: 288–296
Gunnell D (2000) Height, insulin-like growth factors and cancer risk. Growth Horm IGF Res 10 (Suppl A): S39–S40
Gunnell D, Okasha M, Smith GD, Oliver SE, Sandhu J, Holly JM (2001) Height, leg length, and cancer risk: a systematic review. Epidemiol Rev 23: 313–342
Kuper H, Cramer DW, Titus-Ernstoff L (2002) Risk of ovarian cancer in the United States in relation to anthropometric measures: does the association depend on menopausal status? Cancer Causes Control 13: 455–463
Lubin F, Chetrit A, Freedman LS, Alfandary E, Fishler Y, Nitzan H, Zultan A, Modan B (2003) Body mass index at age 18 years and during adult life and ovarian cancer risk. Am J Epidemiol 157: 113–120
Lukanova A, Kaaks R (2005) Endogenous hormones and ovarian cancer: epidemiology and current hypotheses. Cancer Epidemiol Biomarkers Prev 14: 98–107
Lukanova A, Toniolo P, Lundin E, Micheli A, Akhmedkhanov A, Muti P, Zeleniuch-Jacquotte A, Biessy C, Lenner P, Krogh V, Berrino F, Hallmans G, Riboli E, Kaaks R (2002) Body mass index in relation to ovarian cancer: a multi-centre nested case–control study. Int J Cancer 99: 603–608
Malacara JM, Fajardo ME, Nava LE (2001) Gonadotropins at menopause: the influence of obesity, insulin resistance, and estrogens. Steroids 66: 559–567
Must A, Willett WC, Dietz WH (1993) Remote recall of childhood height, weight, and body build by elderly subjects. Am J Epidemiol 138: 56–64
Olsen CM, Green AC, Whiteman DC, Sadeghi S, Kolahdooz F, Webb PM (2007) Obesity and the risk of epithelial ovarian cancer: a systematic review and meta-analysis. Eur J Cancer 43: 690–709
Risch HA (1998) Hormonal etiology of epithelial ovarian cancer, with a hypothesis concerning the role of androgens and progesterone. J Natl Cancer Inst 90: 1774–1786
Rodriguez C, Calle EE, Fakhrabadi-Shokoohi D, Jacobs EJ, Thun MJ (2002) Body mass index, height, and the risk of ovarian cancer mortality in a prospective cohort of postmenopausal women. Cancer Epidemiol Biomarkers Prev 11: 822–828
Rossing MA, Cushing-Haugen KL, Doherty JA, Wicklund KG (2008) Characteristics related to the maternal intrauterine environment and risk of epithelial ovarian cancer. Ann Epidemiol 18: 411–415
Schildkraut JM, Schwingl PJ, Bastos E, Evanoff A, Hughes C (1996) Epithelial ovarian cancer risk among women with polycystic ovary syndrome. Obstet Gynecol 88: 554–559
Schouten LJ, Goldbohm RA, van den Brandt PA (2003) Height, weight, weight change, and ovarian cancer risk in the Netherlands cohort study on diet and cancer. Am J Epidemiol 157: 424–433
Schouten LJ, Rivera C, Hunter DJ, Spiegelman D, Adami HO, Arslan A, Beeson WL, van den Brandt PA, Buring JE, Folsom AR, Fraser GE, Freudenheim JL, Goldbohm RA, Hankinson SE, Lacey Jr JV, Leitzmann M, Lukanova A, Marshall JR, Miller AB, Patel AV, Rodriguez C, Rohan TE, Ross JA, Wolk A, Zhang SM, Smith-Warner SA (2008) Height, body mass index, and ovarian cancer: a pooled analysis of 12 cohort studies. Cancer Epidemiol Biomarkers Prev 17: 902–912
Stoll BA (1998) Teenage obesity in relation to breast cancer risk. Int J Obes Relat Metab Disord 22: 1035–1040
Stunkard AJ, Sorensen T, Schulsinger F (1983) Use of the Danish Adoption Register for the study of obesity and thinness. In The genetics of neurological and psychiatric disorders, Kety SS, Rowland LP, Sidman SW & Mathysee SW (eds) pp 115–120. Raven Press: New York City
Troy LM, Hunter DJ, Manson JE, Colditz GA, Stampfer MJ, Willett WC (1995) The validity of recalled weight among younger women. Int J Obes Relat Metab Disord 19: 570–572
Troy LM, Michels KB, Hunter DJ, Spiegelman D, Manson JE, Colditz GA, Stampfer MJ, Willett WC (1996) Self-reported birthweight and history of having been breastfed among younger women: an assessment of validity. Int J Epidemiol 25: 122–127
Tworoger SS, Fairfield KM, Colditz GA, Rosner BA, Hankinson SE (2007a) Association of oral contraceptive use, other contraceptive methods, and infertility with ovarian cancer risk. Am J Epidemiol 166: 894–901
Tworoger SS, Gertig DM, Gates MA, Hecht JL, Hankinson SE (2008) Caffeine, alcohol, smoking, and the risk of incident epithelial ovarian cancer. Cancer 112: 1169–1177
Tworoger SS, Lee IM, Buring JE, Pollak MN, Hankinson SE (2007b) Insulin-like growth factors and ovarian cancer risk: a nested case-control study in three cohorts. Cancer Epidemiol Biomarkers Prev 16: 1691–1695
Acknowledgements
This study was supported by National Institutes of Health grants P01 CA87969, CA105009, CA50385, and P50 CA105009.We thank Drs Kim Danforth and Robert Barbieri for their input.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Baer, H., Hankinson, S. & Tworoger, S. Body size in early life and risk of epithelial ovarian cancer: results from the Nurses' Health Studies. Br J Cancer 99, 1916–1922 (2008). https://doi.org/10.1038/sj.bjc.6604742
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604742
Keywords
This article is cited by
-
Early-life body mass index and risks of breast, endometrial, and ovarian cancers: a dose–response meta-analysis of prospective studies
British Journal of Cancer (2022)
-
Anthropometric characteristics and ovarian cancer risk and survival
Cancer Causes & Control (2018)
-
The Nightingale study: rationale, study design and baseline characteristics of a prospective cohort study on shift work and breast cancer risk among nurses
BMC Cancer (2014)
-
Genetic variability in IGF-1 and IGFBP-3 and body size in early life
BMC Public Health (2012)
-
Is body size associated with ovarian cancer in southern Chinese women?
Cancer Causes & Control (2012)