Abstract
Antibiotic use in 759 non-Hodgkin's lymphoma (NHL) patients and 589 controls was compared. Neither total antibiotic use (odds ratio=0.7, 95% confidence interval=0.5–1.2), nor antibiotic use by site, was associated with total NHL, or NHL subtypes. There were no trends with frequency or age at first use (P trend=0.23 and 0.26, respectively).
Similar content being viewed by others
Main
The human immunodeficiency virus (HIV) epidemic during the 1980s was paralleled by a 3–4% annual increase in the incidence of non-Hodgkin's lymphoma (NHL) (Hartge et al, 1994). However, NHL incidence had been increasing since before the 1950s (Zheng et al, 1992), with some levelling off in recent years (Eltom et al, 2002; Morton et al, 2006). The dramatic rise in antibiotic use since the 1940s has led some scientists to hypothesise that antibiotics may increase the risk of developing NHL. In vitro evidence suggests that certain antibiotics are cytotoxic (Robbana-Barnat et al, 1997; Summan and Cribb, 2002) or genotoxic (Snyder and Green, 2001), and some may have immunomodulatory effects (Van et al, 1996). Moreover, chronic infections treated with antibiotics, such as tuberculosis, have been associated with NHL (Swerdlow, 2003). While case–control studies of self-reported antibiotic use have found a 30–90% increased risk of NHL (Bernstein and Ross, 1992; Kato et al, 2003; Chang et al, 2005), no associations were observed in case–control studies utilising pharmacy (Beiderbeck et al, 2003) or medical record data (Doody et al, 1996). We investigated the association between NHL and antibiotics in a large multicentre case–control study (1998–2000) within the United States.
Materials and methods
Study methods have been described in detail elsewhere (Chatterjee et al, 2004; Engels et al, 2004; Hartge et al, 2005). Briefly, 1322 newly diagnosed NHL cases were identified from four geographical regions covered by the National Cancer Institute's population-based Surveillance, Epidemiology, and End Results (SEER) cancer registries. All cases residing in Iowa and Seattle, and all African-American cases and a random sample of Caucasian cases residing in Detroit and Los Angeles, aged 20–74 years, with a first primary diagnosis of NHL were eligible. Cases were histologically confirmed and coded according to the International Classification of Diseases-Oncology, 2nd Edition (Percy et al, 1990). NHL cases with known HIV infection were excluded.
Eligible controls were aged 20–74 years, resided in one of the four geographical regions (Iowa, Seattle, Detroit, or Los Angeles) and had no known history of HIV infection or NHL. Controls younger than age 65 were identified using a one-step random digit dialing approach (Casady and Lepowski, 1993). Controls aged 65 years or older were identified from Medicare eligibility files. Controls were frequency matched to the distribution of cases by age (5-year age groups), race, gender, and geographic area.
Human subject review boards at the National Cancer Institute and all participating institutions approved the study. All subjects provided written informed consent.
To accommodate a large number of questions the study population was divided into two groups, each receiving a different version of the computer-assisted personal interview (CAPI). Our analyses are focused on the group, including all African-American and one half of all other participants chosen at random, who completed the CAPI consisting of a detailed medical history questionnaire.
Subjects were asked to recall if they had ever taken antibiotics, in the past 1 year, for infections by organ site and procedure. Information was also obtained about antibiotics used ⩾5 days for conditions/procedures not listed in the questionnaire. These data were combined to create an indicator of having ever used antibiotics. For each positive response information was gathered about the number of times antibiotics were used and the age at first use.
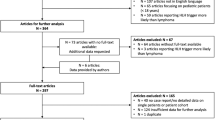
Of the 1332 NHL patients assigned to receive the medical history version of the CAPI, 1017 (76.4%) were contacted. Of these, 175 refused to participate and 83 did not participate for other reasons including serious illness, cognitive impairment or failure to respond to multiple contacts. In total, 759 NHL cases (74.6% of cases approached, 57.0% of eligible cases) participated.
Of the 1419 controls randomly assigned to complete the medical history CAPI, 1196 (84.3%) were contacted. Of these, 525 refused and 82 did not participate for other reasons including serious illness, cognitive impairment, and failure to respond to multiple contacts. Therefore, 589 controls (49.2% of potential controls approached, 41.5% of eligible controls) participated.
Unconditional logistic regression analyses in STATA 10.0 (Stata Corp., College Station, TX, USA) were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between NHL and history of antibiotic use, frequency of use and age at first use of antibiotics (in tertiles). Tertile cut points were based on the distributions among the controls. Tests for linear trend across categories were calculated; reported P-values are two-sided. Additional analyses were performed for the two most common NHL subtypes, diffuse large B-cell lymphoma (DLBCL) and follicular lymphoma, using polytomous logistic regression. Analyses were adjusted for age, gender, race, study site, and education.
Results
Cases were similar to controls with respect to age (P=0.68), gender (P=0.38), and education (P=0.74) but were less likely to be African-American (P=0.03) (Table 1).
Overall, antibiotic use was not associated with an increased risk of NHL or the DLBCL or follicular subtypes. In addition, no significant trends were observed with increasing frequency, or increasing age at first use, of antibiotics, Table 2. No significant associations were observed when we stratified the analyses by age, centre, or education (data not shown).
More specifically, there were no significant associations between NHL overall, or NHL subtypes, and use of antibiotics to treat infections of the upper respiratory tract, eye, ear, gallbladder, urinary tract, bowel, brain, prostate, or skin, or antibiotics used to treat pneumonia, tuberculosis or acne, or antibiotics used before or after dental surgery (data not shown). In addition, no significant trends were observed between NHL and increasing frequency of use, or age at first use, of antibiotics for these conditions (data not shown). However, antibiotic use for genital infections was inversely associated with NHL (OR=0.59, 95% CI=0.39–0.90).
Discussion
Using data collected as part of a large, population-based, case–control study, we found that antibiotic use was not associated with an increased risk of NHL overall, or of the two major subtypes, DLBCL, or follicular lymphoma (FL). An inverse association between antibiotics used to treat genital infections and NHL was observed.
A nested case–control study within the PHARMO database of drug dispensing records in the Netherlands also reported no significant association between ever use of antibiotics and NHL (OR=0.81, 95% CI=0.51–1.26) (Beiderbeck et al, 2003). Another study, from two Kaiser Permanente medical care programmes, found no association between use of chloramphenicol and NHL, but this study lacked information on other antibiotics (Doody et al, 1996).
In contrast, most interview-based case–control studies have reported that antibiotics are associated with a 30–40% increased risk of NHL (Bernstein and Ross, 1992; Chang et al, 2005) and Kato et al (2003), found systemic use of penicillin to be associated with NHL (OR=1.6, 95% CI=1.1–2.2). These investigators have postulated that their findings could be due to a direct carcinogenic effect of antibiotics, differential recall bias or the possibility that frequent antibiotic use could be a surrogate marker for chronic infections or a compromised immune system (Kato et al, 2003; Chang et al, 2005).
Recall bias is a concern in case–control studies. Poor correlation between self-reported medication use and prescription records has been reported (van den Brandt et al, 1991; West et al, 1995). In an attempt to improve recall of self-reported antibiotic usage, we used a method, described by Klungel et al (2000) in which participants are asked to recall their use of medications for a range of conditions. A similar methodological approach was used in the case–control study by Kato et al (2003); however, our study was larger and used a more comprehensive assessment of antibiotic use. In addition, subjects were asked to recall medication usage more than 1 year prior to diagnosis to reduce the possibility of reverse causality. Information was not collected about antibiotic type as it would be difficult to elucidate lifetime use of specific antibiotics from a case–control study; thus, we were unable to determine if specific antibiotic types were associated with NHL. Using diagnostic information from four SEER cancer registries, stratified analyses showed no significant associations between antibiotic use and the two main subtypes of NHL: DLBCL and follicular lymphoma. Although our participation rates for controls were not optimal and could potentially introduce bias, stratification by factors that differed between participants and non-participants (including age, centre, and education) resulted in no significant associations with NHL, suggesting that major biases are unlikely.
An inverse association was observed between antibiotic use for genital infections and NHL. However, the lack of a biologically plausible explanation for this association suggests that it may have resulted by chance since multiple testing was not controlled for in the stratified analyses.
In summary, our results suggest that antibiotic use does not increase NHL risk. Antibiotics are a diverse group of drugs with different mechanisms of action and biological effects (Van et al, 1996). Difficulty of assessing use of specific antibiotics in questionnaire-based case–control studies, as well as lack of biological plausibility for a causative association between non-specific antibiotic use and NHL, suggests that future assessments of this hypothesis should be conducted using cohort studies, with documentation of specific antibiotic use from medical records, or large pharmaceutical data sets.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Beiderbeck AB, Holly EA, Sturkenboom MC, Coebergh JW, Stricker BH, Leufkens HG (2003) Prescription medications associated with a decreased risk of non-Hodgkin's lymphoma. Am J Epidemiol 157: 510–516
Bernstein L, Ross RK (1992) Prior medication use and health history as risk factors for non-Hodgkin's lymphoma: preliminary results from a case–control study in Los Angeles County. Cancer Res 52: 5510s–5515s
Casady R, Lepowski J (1993) Stratified telephone survey designs. Surv Methodol 19: 103–113
Chang ET, Smedby KE, Hjalgrim H, Schollkopf C, Porwit-MacDonald A, Sundstrom C, Tani E, d'Amore F, Melbye M, Adami HO, Glimelius B (2005) Medication use and risk of non-Hodgkin's lymphoma. Am J Epidemiol 162: 965–974
Chatterjee N, Hartge P, Cerhan JR, Cozen W, Davis S, Ishibe N, Colt J, Goldin L, Severson RK (2004) Risk of non-Hodgkin's lymphoma and family history of lymphatic, hematologic, and other cancers. Cancer Epidemiol Biomarkers Prev 13: 1415–1421
Doody MM, Linet MS, Glass AG, Curtis RE, Pottern LM, Rush BB, Boice Jr JD, Fraumeni Jr JF, Friedman GD (1996) Risks of non-Hodgkin's lymphoma, multiple myeloma, and leukemia associated with common medications. Epidemiology 7: 131–139
Eltom MA, Jemal A, Mbulaiteye SM, Devesa SS, Biggar RJ (2002) Trends in Kaposi's sarcoma and non-Hodgkin's lymphoma incidence in the United States from 1973 through 1998. J Natl Cancer Inst 94: 1204–1210
Engels EA, Chatterjee N, Cerhan JR, Davis S, Cozen W, Severson RK, Whitby D, Colt JS, Hartge P (2004) Hepatitis C virus infection and non-Hodgkin lymphoma: results of the NCI-SEER multi-center case–control study. Int J Cancer 111: 76–80
Hartge P, Colt JS, Severson RK, Cerhan JR, Cozen W, Camann D, Zahm SH, Davis S (2005) Residential herbicide use and risk of non-Hodgkin lymphoma. Cancer Epidemiol Biomarkers Prev 14: 934–937
Hartge P, Devesa SS, Fraumeni Jr JF (1994) Hodgkin's and non-Hodgkin's lymphoma. In Cancer surveys: trends in cancer incidence and mortality, Doll R, Fraumeni Jr JF, Muir CS (eds) pp 423–453. Plainview, NY: Cold Spring Harbor Laboratory Press
Kato I, Koenig KL, Baptiste MS, Lillquist PP, Frizzera G, Burke JS, Watanabe H, Shore RE (2003) History of antibiotic use and risk of non-Hodgkin's lymphoma (NHL). Int J Cancer 107: 99–105
Klungel OH, de BA, Paes AH, Herings RM, Seidell JC, Bakker A (2000) Influence of question structure on the recall of self-reported drug use. J Clin Epidemiol 53: 273–277
Morton LM, Wang SS, Devesa SS, Hartge P, Weisenburger DD, Linet MS (2006) Lymphoma incidence patterns by WHO subtype in the United States, 1992–2001. Blood 107: 265–276
Percy C, Van Holten V, Muir C (1990) International Classification of Diseases for Oncology, 2nd edn. Geneva: World Health Organization. Ref Type: Report
Robbana-Barnat S, Decloitre F, Frayssinet C, Seigneurin JM, Toucas L, Lafarge-Frayssinet C (1997) Use of human lymphoblastoid cells to detect the toxic effect of chloramphenicol and metabolites possibly involved in aplastic anemia in man. Drug Chem Toxicol 20: 239–253
Snyder RD, Green JW (2001) A review of the genotoxicity of marketed pharmaceuticals. Mutat Res 488: 151–169
Summan M, Cribb AE (2002) Novel non-labile covalent binding of sulfamethoxazole reactive metabolites to cultured human lymphoid cells. Chem Biol Interact 142: 155–173
Swerdlow AJ (2003) Epidemiology of Hodgkin's disease and non-Hodgkin's lymphoma. Eur J Nucl Med Mol Imaging 30(Suppl 1): S3–S12
van den Brandt PA, Petri H, Dorant E, Goldbohm RA, Van de CS (1991) Comparison of questionnaire information and pharmacy data on drug use. Pharm Weekbl Sci 13: 91–96
Van VB, Vanholder R, De PP, Vogelaers D, Ringoir S (1996) Immunomodulating effects of antibiotics: literature review. Infection 24: 275–291
West SL, Savitz DA, Koch G, Strom BL, Guess HA, Hartzema A (1995) Recall accuracy for prescription medications: self-report compared with database information. Am J Epidemiol 142: 1103–1112
Zheng T, Mayne ST, Boyle P, Holford TR, Liu WL, Flannery J (1992) Epidemiology of non-Hodgkin lymphoma in Connecticut. 1935–1988. Cancer 70: 840–849
Acknowledgements
We acknowledge the effort of the study coordinators and interviewers and also of Lonn Irish, Michael Stagner, and Peter Hui of the Information Management Systems, Silver Spring, MD, and Geoffrey Tobias, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, MD, USA, for help in preparing the manuscript. This research was supported by the Intramural Research Program of the NIH, National Cancer Institute, with Public Health Service (PHS) contracts N01-PC-65064, N01-PC-67008, N01-PC-67009, N01-PC-67010, and N02-PC-71105. The Research and Development Office, Northern Ireland funded Dr Lesley Anderson to participate in the Cancer Prevention Fellowship Program, Office of Preventative Oncology, Division of Cancer Prevention, National Cancer Institute through the Ireland-Northern Ireland-USA Consortium.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Anderson, L., Gridley, G., Engels, E. et al. Antibiotic use and risk of non-Hodgkin's lymphoma: a population-based case–control study. Br J Cancer 98, 161–164 (2008). https://doi.org/10.1038/sj.bjc.6604127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604127