Abstract
The aim of the study was to determine the impact of the absolute number and ratio of positive lymph nodes on the survival in node-positive endometrioid uterine cancer. Data were obtained from the National Cancer Institute Registry from 1988 to 2001. Analyses were performed using Kaplan–Meier and Cox proportional hazard methods. A total of 1222 women were diagnosed with stage IIIC-IV node-positive endometrioid corpus cancer. The 5-year disease-specific survival of women with 1, 2–5, and >5 positive nodes were 68.1, 55.1, and 46.1%, respectively (P<0.001). Increasing lymph node ratio, expressed as a percentage of positive nodes to total nodes identified (⩽10, >10–⩽50, and >50%), was associated with a decrease in survival from 77.3 to 60.7 to 40.9%, respectively (P<0.001). The absolute number of positive nodes and the lymph node ratio remained significant after adjusting for stage (IIIC vs IV) and the extent of lymphadenectomy (⩽20 vs >20 nodes). On multivariate analysis, the absolute number of positive nodes and lymph node ratio were significant independent prognostic factors for survival. Increasing absolute number of positive nodes and lymph node ratio are associated with a poorer survival in women with node-positive uterine cancers. The stratification of node-positive uterine cancer for prognostic and treatment purposes warrants further investigation.
Similar content being viewed by others
Main
Endometrial carcinoma is the most common gynaecological malignancy in the United States with an expected 7350 deaths associated with this disease in 2006 (Jemal et al, 2006). Although approximately 80% of patients are diagnosed with early-stage (I–II) disease and have an excellent prognosis, women with advanced-stage (III–IV) cancers have significantly poorer outcome. Metastatic involvement of retroperitoneal lymph nodes is one of the most important prognostic factors (Morrow et al, 1991). Of the patients with node-positive disease, the estimated 5-year disease-specific survival ranges from 10 to 75% (Potish et al, 1985; Larson et al, 1987; Lurain et al, 1991; Morrow et al, 1991; Rose et al, 1992; Greven et al, 1993; Schorge et al, 1996; Nelson et al, 1999; Mariani et al, 2002; Watari et al, 2005; Chan et al, 2006; Randall et al, 2006). The wide range of outcomes suggests that there exists considerable heterogeneity in these node-positive patients based on various clinicopathological prognostic factors. Furthermore, over 50% of stage III–IV disease patients fail standard treatments with either whole abdominal radiation or chemotherapy and experience significant toxicities (Bruner et al, 2006; Randall et al, 2006). Studies focused on defining these prognostic factors may permit better substage stratification and determine novel treatment strategies. For example, multi-modality therapies should be designed for high-risk patients to improve survival and individualised tailored therapies are preferred in low-risk patients to prevent toxicities associated with over-treatment.
The association between the extent of lymph node involvement and survival has been demonstrated in most solid tumours including lung, breast, colon, rectal, bladder, cervical, and vulva cancers (van der Velden et al, 1995; Moore and Stehman, 1996; Tepper et al, 2001; Herr et al, 2002; Weir et al, 2002; Gajra et al, 2003; Joseph et al, 2003; Le Voyer et al, 2003). Furthermore, the number of nodal metastases in breast cancer is not only used as a prognostic tool but it also guides adjuvant treatment (NCCN, 2006). However, the current staging system for uterine cancer under International Federation of Gynecology and Obstetrics (FIGO) does not account for the extent of nodal disease. Prior studies have shown that patients with stage IIIC uterine cancer limited only to the pelvic nodes have significantly better prognosis than for other subgroups of stage IIIC disease, suggesting that stratification may be appropriate (Morrow et al, 1991; Nelson et al, 1999; Mariani et al, 2002; Watari et al, 2005).
In this present study, we determined the prognostic significance of the absolute number and ratio of positive lymph nodes in endometrioid uterine cancer. Furthermore, we identified other clinicopathological prognostic factors important in node-positive corpus cancer.
Patients and methods
Demographic, clinicopathological, treatment, and survival information of women diagnosed with endometrioid corpus cancer during the period from 1 January 1988 to 31 December 2001 was extracted with permission from the Surveillance, Epidemiology and End Results (SEER) programme of the United States National Cancer Institute (Surveillance, 2005). This data represent approximately 14% of the US population and is reported from 12 population-based registries including San Francisco-Oakland, Connecticut, metropolitan Detroit, Hawaii, Iowa, New Mexico, Seattle (Puget Sound), Utah, metropolitan Atlanta, Alaska, San Jose-Monterey, and Los Angeles.
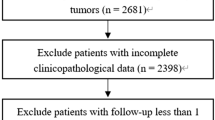
Of the 40 880 women diagnosed with endometrioid uterine cancer, 1222 patients had stage IIIC–IV disease with at least one positive pelvic and/or paraaortic lymph node. All patients underwent surgical staging including lymphadenectomy. Information regarding patient age, stage, tumour grade, number of positive lymph nodes, extent of lymph node dissection (defined as the total number of lymph nodes recovered), and use of adjuvant radiation therapy was extracted. Patients were divided into three nodal groups (1, 2–5, and >5 positive nodes). The lymph node ratio, expressed as the percentage of positive nodes to total nodes identified, was stratified into three groups (⩽10, >10–⩽50, and >50%).
Statistical analysis was performed using the Intercooled STATA 8.0 program (College Station, TX). Survival analysis was performed using the Kaplan–Meier method. The outcome of interest was death from endometrial cancer. Time to death was censored in women who died from causes other than uterine cancer. The Cox proportional hazards model was used to identify independent predictors of survival. A forward stepwise model was used to determine which prognostic variable was more important for prediction of outcome. Two-tailed tests at P-values less than 0.05 were considered significant.
Results
Patient characteristics of 1222 women diagnosed with stage IIIC–IV node-positive endometrioid uterine cancer are shown in Table 1. The median age at diagnosis was 64 years (range: 28–93 years). 639 (52.3%) were stage IIIC, 24 (2.0%) were stage IVA, and 559 (45.7%) were stage IVB. The median number of lymph nodes removed was 11 (range: 1–90). The median number of positive lymph nodes was 2 (range: 1–52) and the median lymph node ratio was 23.2% (range: 1.8–100%). The 5-year disease-specific survivals of patients with stage IIIC and IV were 70.3 and 47.8%, respectively (P<0.001). A more extensive lymphadenectomy (P<0.001), lower grade tumours (P<0.001), and use of radiotherapy (P<0.001) were associated with an improved survival (Table 2).
When all patients were divided into three groups based on the number of positive lymph nodes (1, 2–5, and >5 positive nodes), the 5-year disease-specific survival decreased from 68.1 to 55.1 to 46.1%, respectively (P<0.001; Figure 1). Adjusted for stage of disease, the association between absolute number (1, 2–5, and >5) of positive nodes and survival rates were 77.1, 60.9, and 69.1%, respectively (P=0.003) in patients with stage IIIC disease and 50.9, 49.8, and 38.9%, respectively (P=0.099) in stage IV cancers (Figure 2A and C). The prognostic significance of the absolute number of positive nodes was also examined based on the extent of lymphadenectomy. In those with ⩽20 nodes identified, the absolute number (1, 2–5, and >5) of positive nodes was associated with a decrease in survival from 65.1 to 50 to 29.7%, respectively (P<0.001). In addition, women with >20 nodes identified had an associated decrease in survival from 82.6 to 71.9 to 59.7%, respectively (P=0.047; Figure 3A and C) for the three positive nodal groups.
Increasing lymph node ratio (⩽10, >10–⩽50, and >50%) was associated with a decrease in 5-year disease-specific survival from 77.3 to 60.7 to 40.9%, respectively (P<0.001; Figure 1). For patients with stage IIIC disease, survival decreased from 78.6 to 66.5 to 65.3%, corresponding to the three lymph node ratio groups (P=0.025), and this finding was consistent in stage IV cancers with associated survival rates of 73.8 to 53.3 to 30.1%, respectively (P<0.001; Table 2 and Figure 2B and D). We also divided the study group based on the extent of lymphadenectomy and found that the group with ⩽20 nodes resected had associated survivals of 73.5, 60.1, and 39.5%, for the three corresponding lymph node ratio groups, respectively (P<0.001). Similarly, those with >20 nodes resected had survival rates of 80.6, 62.9, and 57.6% (P=0.052; Figure 3B and D). The impact of the absolute number and ratio of positive nodes by stage, grade of disease, radiation therapy, and extent of lymphadenectomy on survival is summarised in Table 2.
On multivariate analysis, the absolute number of positive lymph nodes (P=0.005) and the lymph node ratio (P=0.003) were independent prognostic factors for survival adjusting for age, stage, grade of disease, year of diagnosis, adjuvant radiation, and extent of lymphadenectomy (Table 3). Hazard ratios were higher for patients with more than 5 positive nodes relative to those with 2–5 positive or 1 positive node (HR=1.63 vs 1.28 vs 1.0, respectively). Moreover, the hazard ratio was significantly higher for each percent increase in lymph node ratio (HR=1.05 for a 10% increase in lymph node ratio). Correlation between these variables was relatively small (r=0.2), thus each contributed independently to the prediction of the hazard rate. In forward stepwise regression, lymph node ratio entered the model before absolute number of positive nodes suggesting an overall greater prognostic ability. However, when the analysis is restricted to patients with less extensive lymphadenectomy (⩽10 nodes), only the absolute number of positive nodes contributed significantly to prediction of survival (P=0.005 for absolute number of positive nodes; P=0.186 for lymph node ratio).
Discussion
Advanced stage uterine cancer continues to be a significant cause of death among gynaecological cancers in the United States (Jemal et al, 2006). Prior studies have found that stage IIIC node-positive endometrial cancers comprise of only 2–6% of all cases (Creasman et al, 1987; Lurain et al, 1991; Morrow et al, 1991; Greven et al, 1993; Schorge et al, 1996; Faught et al, 1998). Given that it is difficult for institutions to collect a large series of women with node-positive uterine cancer, this subgroup of patients has not been well studied. In addition, the prognostic factors in these high-risk patients have not been extensively characterised. In this current series of 1222 women with node-positive endometrioid uterine cancer, we determined the prognostic significance of the absolute number and ratio of positive nodes. In addition, this is one of the first papers that compared the prognostic significance of lymph node ratio to absolute number of positive nodes in patients with endometrial cancer.
Since women with node-positive endometrioid uterine cancer have a wide range of survival from 10 to 75% (Potish et al, 1985; Larson et al, 1987; Lurain et al, 1991; Morrow et al, 1991; Rose et al, 1992; Greven et al, 1993; Schorge et al, 1996; Faught et al, 1998; Nelson et al, 1999; Mariani et al, 2002; Watari et al, 2005; Chan et al, 2006; Randall et al, 2006), several investigators have suggested substaging these patients (Nelson et al, 1999; Mariani et al, 2002; Watari et al, 2005). In this current report, our findings support the concept of stratifying node-positive cancers into substages based on nodal burden. The 5-year disease-specific survival of this heterogeneous cohort of node-positive patients in our study ranges from approximately 40 to 77%.
The prognostic significance of the absolute number and/or ratio of positive nodes has been reported in other solid tumours (van der Velden et al, 1995; Moore and Stehman, 1996; Tepper et al, 2001; Bando et al, 2002; Herr et al, 2002; Weir et al, 2002; Gajra et al, 2003; Joseph et al, 2003; Le Voyer et al, 2003; Berger et al, 2005; Sierzega et al, 2006). In breast cancer, the nodal ratio has been shown to be an important predictor of loco-regional recurrence and survival both from initial diagnosis and following recurrence (Nieto et al, 2002; Grills et al, 2003; Woodward et al, 2006). Several studies compared the prognostic value of nodal ratios to the absolute number of positive nodes and found that lymph node ratio had a stronger prognostic value in breast cancer (Vinh-Hung et al, 2004; Woodward et al, 2006).
Small retrospective studies from single institutions have evaluated the significance of the absolute number and ratio of positive nodes in uterine cancers. Mariani et al (2001) studied 60 patients with endometrial cancer with pelvic nodal metastases. These authors found that patients who recurred or died of disease had a higher percentage of positive lymph nodes at presentation. Similarly, Tang et al, (1998) evaluated 40 patients with pelvic and/or paraaortic nodal metastases and found a 5-year disease-specific survival of 0 vs 55% in those with ⩾25 vs <25% lymph node ratio. Yasunaga et al, (2003) have also shown that a high metastatic ratio is associated with a lower survival. Patients with lymph node ratios of <10, 10–50, and >50% had 5-year survival rates of 82.5, 43.8, and 0%, respectively (Yasunaga et al, 2003). However, these studies were limited by the small sample sizes and inclusion of high-risk cell types such as serous and clear cell cancers. More importantly, there may exist a potential selection bias due to reporting from tertiary care academic centres caring for high-risk patients. Thus, these small study cohorts may not be representative of the general population. Furthermore, these studies did not compare the prognostic importance of nodal ratio to the absolute number of positive nodes, likely due to the limitations in sample size.
On multivariate analysis of the 1222 node-positive patients in this current study, the absolute number (P=0.005) and lymph node ratio (P=0.003) remained as independent prognostic factors after adjusting for age, stage, grade of disease, and extent of lymph node dissection. The correlation between the categorical variables, absolute number and ratio of positive nodes, was relatively small and thus both variables were independent predictors for survival. Analysed as a continuous variable, lymph node ratio entered the proportional hazard model before absolute number of positive nodes in stepwise regression suggesting that the lymph node ratio may better characterise prognostic subgroups than the number of positive nodes. In addition, Kaplan–Meier analyses provide further support showing a larger separation of curves depicted in the overall study group (Figure 1) and substages of IIIC vs IV cancers (Figure 2).
Compared to the absolute number of positive lymph nodes, the lymph node ratio may be a better predictor of tumour burden and aggressive biological behaviour of the tumour, particularly in those who had a more extensive lymphadenectomy. As such, the survival differences within these subgroups by lymph node ratio were more pronounced. However, in patients with a limited number of lymph nodes recovered, the absolute number of positive nodes appears to be a better predictor. It is important to note that the number of nodes recovered may reflect a more extensive dissection, comprehensiveness of pathological evaluation, variations in number of nodes of each patient, and difficulties in performing lymphadenectomies due to medical comorbidities (Yasunaga et al, 2003).
The majority of stage III–IV uterine cancer patients fail standard chemotherapy or whole abdominal radiation (Randall et al, 2006). It would be important to identify the patients at particularly high risk of recurrence in whom a combination of chemotherapy and radiation therapy may be beneficial, while sparing lower-risk patients from the toxicity of excessive therapy (Bruner et al, 2006). Extrapolating from breast cancer treatment recommendations, it may be possible that tailored therapy can be selected based on stratifying patients with node-positive uterine cancer into various risk groups. For example, local irradiation may be adequate for those with low numbers of lymph nodes involved, particularly if a thorough lymphadenectomy was performed. In contrast, higher-risk patients with a larger nodal tumour burden may warrant more extensive treatment including systemic chemotherapy combined with site-specific irradiation. In fact, a current Gynecologic Oncologic Group trial is investigating the role of multi-modality therapy in advanced uterine cancer to define the optimal chemotherapy combined with radiation (Homesley et al, 2000).
The finding that the overall number of lymph nodes removed at surgery correlates with survival has been previously reported (Kilgore et al, 1995; Blythe et al, 1997; McMeekin et al, 2001; Chan et al, 2006; Lutman et al, 2006; Mariani et al, 2006). In early-stage disease, it is not clear whether this benefit is due directly to cytoreductive effects of surgery or from more accurate staging. In this current study of node-positive patients, we found that a more extended dissection remained as an important predictor for survival after controlling for the absolute number and ratio of positive nodes. The improvement in survival associated with extent of lymph node resection and possible mechanisms have been previously reported (Chan et al, 2006). Lastly, it is possible that lymph node dissection may be a surrogate for the quality comprehensive care rather than the cause that resulted in the better outcome of these patients.
Our study has several recognisable limitations. There is a lack of information on surgeon sub-specialty, comprehensive surgical staging, central pathology review, adjuvant hormonal and chemotherapy, time to recurrence, subsequent surgical and medical therapies, and surgical morbidity. Additionally, there was limited data on the specific laterality and location of nodal resection. Moreover, our data do not have detailed information regarding the depth of myometrial invasion, peritoneal cytology, extent of nodal debulking, and extent of extrauterine involvement associated with the node-positive cancer. It is conceivable that the extent of extrauterine involvement may be strongly correlated with the lymph node burden and thus confound our findings.
The strengths of this study include the fact that this is one of the largest studies evaluating the impact of nodal burden and lymphadenectomy on the survival of node-positive endometrioid uterine cancer. In addition, all patients with high-risk cell types such as papillary serous, clear cell, and sarcomas were excluded from the analyses. The wide geographical distribution of patients including 12 US regions also decreases the potential selection and surveillance biases that are associated with single-institution analyses (Surveillance, 2005). Furthermore, the results from this population-based study can be generalised to the entire US population. The quality control measures of the SEER programme allow the registry to maintain the highest level of certification of data quality and completeness reported by the Northern American Association of Central Cancer Registries.
In summary, improving risk assessments in advanced endometrial cancers beyond the current FIGO staging definition is of particular interest as the treatment of high-risk uterine cancers evolves. The sub-classification of node-positive cancers based on the absolute number and ratio of positive nodes may assist the physician to better define prognosis and more importantly, stratify patients into various risk groups in the design of future clinical trials. If confirmed in a prospective clinical trial, these findings may ultimately modify the current staging system and lead to individualised tailored therapies in patients with node-positive uterine cancer.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bando E, Yonemura Y, Taniguchi K, Fushida S, Fujimura T, Miwa K (2002) Outcome of ratio of lymph node metastasis in gastric carcinoma. Ann Surg Oncol 9: 775–784
Berger AC, Sigurdson ER, LeVoyer T, Hanlon A, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG (2005) Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol 23: 8706–8712
Blythe JG, Edwards E, Heimbecker P (1997) Paraaortic lymph node biopsy: a twenty-year study. Am J Obstet Gynecol 176: 1157–1162;discussion 1162–5
Bruner DW, Barsevick A, Tian C, Randall M, Mannel R, Cohn DE, Sorosky J, Spirtos NM (2006) Randomized trial results of quality of life comparing whole abdominal irradiation and combination chemotherapy in advanced endometrial carcinoma: a gynecologic oncology group study. Qual Life Res 16: 89–100
Chan JK, Cheung MK, Huh WK, Osann K, Husain A, Teng NN, Kapp DS (2006) Therapeutic role of lymph node resection in endometrioid corpus cancer: a study of 12 333 patients. Cancer 107: 1823–1830
Creasman WT, Morrow CP, Bundy BN, Homesley HD, Graham JE, Heller PB (1987) Surgical pathologic spread patterns of endometrial cancer. A gynecologic oncology group study. Cancer 60: 2035–2041
Faught W, Faught F, Fung MFK, Krepart GV, Lotocki RJ, Heywood MS, Genest P (1998) Microscopic surgical stage IIIc endometrioid adenocarcinoma of the endometrium: implications for bimodal adjuvant therapy. Int J Gynecol Cancer 8: 41–45
Gajra A, Newman N, Gamble GP, Kohman LJ, Graziano SL (2003) Effect of number of lymph nodes sampled on outcome in patients with stage I non-small-cell lung cancer. J Clin Oncol 21: 1029–1034
Greven KM, Lanciano RM, Corn B, Case D, Randall ME (1993) Pathologic stage III endometrial carcinoma. Prognostic factors and patterns of recurrence. Cancer 71: 3697–3702
Grills IS, Kestin LL, Goldstein N, Mitchell C, Martinez A, Ingold J, Vicini FA (2003) Risk factors for regional nodal failure after breast-conserving therapy: regional nodal irradiation reduces rate of axillary failure in patients with four or more positive lymph nodes. Int J Radiat Oncol Biol Phys 56: 658–670
Herr HW, Bochner BH, Dalbagni G, Donat SM, Reuter VE, Bajorin DF (2002) Impact of the number of lymph nodes retrieved on outcome in patients with muscle invasive bladder cancer. J Urol 167: 1295–1298
Homesley HD et al. (2000) GOG Protocol no #184. A randomized Phase III study of tumor volume directed pelvic plus or minus para-aortic irradiation followed by cisplatin doxorubicin or cisplatin doxorubicin paclitaxel for advanced endometrial carcinoma
Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun MJ (2006) Cancer statistics, 2006. CA Cancer J Clin 56: 106–130
Joseph NE, Sigurdson ER, Hanlon AL, Wang H, Mayer RJ, MacDonald JS, Catalano PJ, Haller DG (2003) Accuracy of determining nodal negativity in colorectal cancer on the basis of the number of nodes retrieved on resection. Ann Surg Oncol 10: 213–218
Kilgore LC, Partridge EE, Alvarez RD, Austin JM, Shingleton HM, Noojin III F, Conner W (1995) Adenocarcinoma of the endometrium: survival comparisons of patients with and without pelvic node sampling. Gynecol Oncol 56: 29–33
Larson DM, Copeland LJ, Gallager HS, Wharton JT, Gershenson DM, Edwards CL, Malone Jr JM, Rutledge FN (1987) Prognostic factors in stage II endometrial carcinoma. Cancer 60: 1358–1361
Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, Haller DG (2003) Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol 21: 2912–2919
Lurain JR, Rice BL, Rademaker AW, Poggensee LE, Schink JC, Miller DS (1991) Prognostic factors associated with recurrence in clinical stage I adenocarcinoma of the endometrium. Obstet Gynecol 78: 63–69
Lutman CV, Havrilesky LJ, Cragun JM, Secord AA, Calingaert B, Berchuck A, Clarke-Pearson DL, Soper JT (2006) Pelvic lymph node count is an important prognostic variable for FIGO stage I and II endometrial carcinoma with high-risk histology. Gynecol Oncol 102: 92–97
Mariani A, Dowdy SC, Cliby WA, Haddock MG, Keeney GL, Lesnick TG, Podratz KC (2006) Efficacy of systematic lymphadenectomy and adjuvant radiotherapy in node-positive endometrial cancer patients. Gynecol Oncol 101: 200–208
Mariani A, Webb MJ, Keeney GL, Haddock MG, Aletti G, Podratz KC (2002) Stage IIIC endometrioid corpus cancer includes distinct subgroups. Gynecol Oncol 87: 112–117
Mariani A, Webb MJ, Rao SK, Lesnick TG, Podratz KC (2001) Significance of pathologic patterns of pelvic lymph node metastases in endometrial cancer. Gynecol Oncol 80: 113–120
McMeekin DS, Lashbrook D, Gold M, Scribner DR, Kamelle S, Tillmanns TD, Mannel R (2001) Nodal distribution and its significance in FIGO stage IIIc endometrial cancer. Gynecol Oncol 82: 375–379
Moore DH, Stehman FB (1996) What is the appropriate management of early stage cervical cancer (International Federation of Gynecology and Obstetrics stages I and IIA), surgical assessment of lymph nodes, and role of therapeutic resection of lymph nodes involved with cancer? J Natl Cancer Inst Monogr 43–46
Morrow CP, Bundy BN, Kurman RJ, Creasman WT, Heller P, Homesley HD, Graham JE (1991) Relationship between surgical-pathological risk factors and outcome in clinical stage I and II carcinoma of the endometrium: a gynecologic oncology group study. Gynecol Oncol 40: 55–65
Nelson G, Randall M, Sutton G, Moore D, Hurteau J, Look K (1999) FIGO stage IIIC endometrial carcinoma with metastases confined to pelvic lymph nodes: analysis of treatment outcomes, prognostic variables, and failure patterns following adjuvant radiation therapy. Gynecol Oncol 75: 211–214
Nieto Y, Nawaz S, Jones RB, Shpall EJ, Cagnoni PJ, McSweeney PA, Baron A, Razook C, Matthes S, Bearman SI (2002) Prognostic model for relapse after high-dose chemotherapy with autologous stem-cell transplantation for stage IV oligometastatic breast cancer. J Clin Oncol 20: 707–718
NCCN (2006) NCCN Clinical Practice Guidelines in Oncology Breast Cancer. V.2.2006
Potish RA, Twiggs LB, Adcock LL, Savage JE, Levitt SH, Prem KA (1985) Paraaortic lymph node radiotherapy in cancer of the uterine corpus. Obstet Gynecol 65: 251–256
Randall ME, Filiaci VL, Muss H, Spirtos NM, Mannel RS, Fowler J, Thigpen JT, Benda JA (2006) Randomized phase III trial of whole-abdominal irradiation vs doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: a gynecologic oncology group study. J Clin Oncol 24: 36–44
Rose PG, Cha SD, Tak WK, Fitzgerald T, Reale F, Hunter RE (1992) Radiation therapy for surgically proven para-aortic node metastasis in endometrial carcinoma. Int J Radiat Oncol Biol Phys 24: 229–233
Schorge JO, Molpus KL, Goodman A, Nikrui N, Fuller Jr AF (1996) The effect of postsurgical therapy on stage III endometrial carcinoma. Gynecol Oncol 63: 34–39
Sierzega M, Popiela T, Kulig J, Nowak K (2006) The ratio of metastatic/resected lymph nodes is an independent prognostic factor in patients with node-positive pancreatic head cancer. Pancreas 33: 240–245
Surveillance, Epidemiology End Results (SEER) Program (2005) (www.seer.cancer.gov) SEER*Stat Database: incidence SEER 9 Regs Public-Use, Nov 2004 Sub (1973–2002), National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch
Tang X, Tanemura K, Ye W, Ohmi K, Tsunematsu R, Yamada T, Katsumata N, Sonoda T (1998) Clinicopathological factors predicting retroperitoneal lymph node metastasis and survival in endometrial cancer. Jpn J Clin Oncol 28: 673–678
Tepper JE, O'Connell MJ, Niedzwiecki D, Hollis D, Compton C, Benson III AB, Cummings B, Gunderson L, Macdonald JS, Mayer RJ (2001) Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 19: 157–163
van der Velden J, van Lindert AC, Lammes FB, ten Kate FJ, Sie-Go DM, Oosting H, Heintz AP (1995) Extracapsular growth of lymph node metastases in squamous cell carcinoma of the vulva. The impact on recurrence and survival. Cancer 75: 2885–2890
Vinh-Hung V, Verschraegen C, Promish DI, Cserni G, Van de Steene J, Tai P, Vlastos G, Voordeckers M, Storme G, Royce M (2004) Ratios of involved nodes in early breast cancer. Breast Cancer Res 6: R680–R688
Watari H, Todo Y, Takeda M, Ebina Y, Yamamoto R, Sakuragi N (2005) Lymph-vascular space invasion and number of positive para-aortic node groups predict survival in node-positive patients with endometrial cancer. Gynecol Oncol 96: 651–657
Weir L, Speers C, D'Yachkova Y, Olivotto IA (2002) Prognostic significance of the number of axillary lymph nodes removed in patients with node-negative breast cancer. J Clin Oncol 20: 1793–1799
Woodward WA, Vinh-Hung V, Ueno NT, Cheng YC, Royce M, Tai P, Vlastos G, Wallace AM, Hortobagyi GN, Nieto Y (2006) Prognostic value of nodal ratios in node-positive breast cancer. J Clin Oncol 24: 2910–2916
Yasunaga M, Yamasaki F, Tokunaga O, Iwasaka T (2003) Endometrial carcinomas with lymph node involvement: novel histopathologic factors for predicting prognosis. Int J Gynecol Pathol 22: 341–346
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Chan, J., Kapp, D., Cheung, M. et al. The impact of the absolute number and ratio of positive lymph nodes on survival of endometrioid uterine cancer patients. Br J Cancer 97, 605–611 (2007). https://doi.org/10.1038/sj.bjc.6603898
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603898
Keywords
This article is cited by
-
Significance of lymph node ratio on survival of women with borderline ovarian tumors
Archives of Gynecology and Obstetrics (2020)
-
Stage IIIC endometrial cancer: the need for novel subgrouping according to the ratio of metastatic lymph nodes
Archives of Gynecology and Obstetrics (2015)
-
Combining the negative lymph nodes count with the ratio of positive and removed lymph nodes can better predict the postoperative survival in cervical cancer patients
Cancer Cell International (2013)
-
The role of uterine manipulators in endometrial cancer recurrence after laparoscopic or robotic procedures
Archives of Gynecology and Obstetrics (2013)
-
Prognostic discrimination of subgrouping node-positive endometrioid uterine cancer: location vs nodal extent
British Journal of Cancer (2011)