Abstract
Malignant glioma is characterised by extensive neovascularisation, principally influenced by vascular endothelial growth factor (VEGF). ZD6474 is a potent inhibitor of VEGF-R2 tyrosine kinase activity, but with additional inhibitory effects on other growth factors. In this study, we have investigated the effects of ZD6474 with regard to tumour growth, neovascularisation, proliferation and apoptosis in the intracerebral rat glioma model, BT4C. ZD6474 (50 and 100 mg kg−1) was given as a daily oral gavage. Animals were killed on day 19 and tumour volume was measured. Sections were stained for factor VIII, Ki-67 and for apoptosis. The ability of ZD6474 to inhibit cell growth directly was examined in vitro, using the glioma cell line BT4C and the transformed rat brain endothelial cell line RBE4. Cell growth was analysed with fluorometric microculture cytotoxicity assay to quantify the cytotoxic effects. ZD6474 significantly decreased tumour volume compared to controls. Microvascular density increased after treatment with ZD6474, and tumour cell proliferation index was reduced. There was also an increase in tumour cell apoptosis. In vitro, the growth of both cell lines was significantly reduced. The results reported justify further experimental investigations concerning the effects of ZD6474 in malignant glioma alone or in combination with other modalities.
Similar content being viewed by others
Main
Despite extensive treatment efforts, the prognosis for patients suffering from malignant glioma is poor. The search for new treatment modalities as well as improving the efficacy of conventional chemotherapy and radiotherapy is therefore of utmost importance. Malignant glioma is morphologically characterised by extensive pathological neovascularisation, and microvascular density (MVD) is a negative prognostic marker in both low-grade and high-grade glioma (Leon et al, 1996; Abdulrauf et al, 1998). The neovascularisation is controlled by several different growth regulatory factors of which vascular endothelial growth factor (VEGF) is one of the most important (Yamada et al, 1997). Today there are five members in the VEGF family, named A–E. All members signal through three specific receptor tyrosine kinases. VEGFR-1 and -2 are selectively expressed on endothelial cells and VEGFR-3 mostly on lymphatic endothelium, but also on tumour blood vessels (Aprelikova et al, 1992; Dvorak, 2002). Vascular endothelial growth factor-A is recognised as the single most important angiogenesis factor with effects on endothelial cell proliferation, protease expression and migration (Machein and Plate, 2000; Ferrara et al, 2003). Other growth factors are also of obvious importance, including epidermal growth factor (EGF). Epidermal growth factor and its receptor EGFR contribute to a number of processes important for cancer development and progression, including cell proliferation, apoptosis, angiogenesis and metastatic spread (Ciardiello and Tortora, 2001). Epidermal growth factor receptor is rarely present in normal glial cells, but is expressed in human gliomas. The overexpression of EGFR mRNA, caused by amplification of the erbB-1 gene, has been observed in approximately 40–50% of human glioblastomas (Dunn et al, 2000). A truncated and constitutively activated form of EGFR, EGFRvIII, is also frequently seen in glioma and is able to increase VEGF expression in glioma cells (Feldkamp et al, 1999). ZD6474, a low molecular weight receptor tyrosine kinase inhibitor (Hennequin et al, 2002), inhibits the VEGFR-2 tyrosine kinase with additional effects on VEGFR-3 and EGFR (Wedge et al, 2002; Ciardiello et al, 2003). In this study, we evaluated the effects of ZD6474 on tumour growth in the intracerebral BT4C glioma model.
Material and methods
Animal model
The previously characterised syngenic intracerebral BT4C rat glioma model was used for the in vivo experiments in this study (Bergenheim et al, 1994; Johansson et al, 2000) (Figure 1). BT4C rat glioma cells growing in log phase were suspended in Dulbecco's modification of Eagle's MEM (DMEM) (Gibco, Paisley, Scotland) supplied with 5% BD IX rat serum to a concentration of 20 000 cells in 5 μl. Inbred BD IX rats were anaesthetised with a 1 : 1 mixture of Hypnorm® (fluanisone 10 mg ml−1 and fentanyl citrate 0.315 mg ml−1) and Dormicum® (midazolam 5 mg ml−1) 0.5 ml (100 g)−1 administered as a single i.p. injection. Xylocain® 10 mg ml−1 was used for local anaesthesia in the skin of the scalp before incision. With a 22G microsyringe (Unimetrics, Shorewood, IL, USA) fitted to the micromanipulator of a stereotactic frame, 5 μl of the cell suspension was implanted 3.5 mm to the right of bregma at a depth of 4.5 mm (males) and 3.5 mm (females) into the right caudate nucleus under stereotactic conditions. Special care was taken to prevent cellular reflux through the insertion canal and the burr hole in the skull was covered with bone wax. During the implantation procedure, cells were kept on ice and viability was monitored by intermittent tryphan blue staining. After implantation animals were housed in a controlled environment with 12 h light/dark cycles and provided with food and water ad libitum. Animals were supervised by an experienced animal keeper who continuously evaluated their overall clinical condition.
Regarding animal welfare, consideration was taken not to expose the animals to unmotivated suffering. The experiments were carried out in strict accordance with the UKCCCR guidelines (Workman et al, 1998). The experiment was approved by the local ethics committee for animal research in accordance with the Swedish Animal Welfare Act 1988:534 as last amended by SFS 2002:550, which are adopted in consequence of EC Directive 86/609/EEC (see www.sweden.gov.se/content/1/c6/02/58/44/51574064.pdf).
For this experiment, 21 animals were used and randomised into three groups with seven animals in each group. The doses chosen is based on published data where it is reported that ZD6474 15–100 mg kg day−1 given once daily p.o. to rats for up to 5 weeks was well tolerated, with only small effects on body weight and no adverse effects on clinical condition (Wedge et al, 2002). There are no published data on experiments made in intracerebral rat models and in this experiment we chose the doses 50 and 100 mg kg−1. These dose levels are within the range recommended by the manufacturers. The control group received 1 ml vehicle, 1% Tween-80 (Merck-Schuchardt, Hohenbrunn, Germany) and the other two groups were treated with ZD6474 50 and 100 mg kg−1, respectively. ZD6474 and vehicle were given as a daily oral gavage with disposable animal feeding needles with silicon tip (Scanbur BK AB, Sollentuna, Sweden), starting day 6 after tumour implantation. Animals were weighed twice a week and killed by decapitation on day 19, before they showed neurological symptoms. Blood samples were collected for analysis. The brains were carefully dissected out, placed in phosphate-buffered formalin over night and thereafter fixed in 70% ethanol until paraffin embedded. The total treatment time for the control group and the group receiving ZD6474 50 mg kg−1 was 13 days. Owing to poor tolerability in the group that received ZD6474 100 mg kg−1, the administration of ZD6474 was ended 1 day earlier. The total treatment time for this group was therefore 12 days. Two animals from the group receiving 100 mg kg−1 died before the rest of the animals were killed, one at day 18 and one at day 19.
ZD6474
ZD6474 was kindly provided from Astra Zeneca, Alderly Park, UK. For details and chemical structure, see Hennequin et al (2002). For in vivo experiments, ZD6474 was dissolved according to the manufacturer's instructions in 1% Tween-80 (Merck-Schuchardt, Hohenbrunn, Germany) to a concentration of 20 mg ml−1. To obtain a uniform suspension, an equal volume of glass beads were added to the mixture and the suspension was then milled over night at room temperature and used within 1 week. For in vitro studies, ZD6474 was dissolved in 100% DMSO (Sigma, Stockholm, Sweden) to a concentration of 10 mM. The stock solution was then diluted in cell culture media to achieve different working concentrations.
Tumour volume
Tumours were sectioned and stained with haematoxylin–eosin. Tumour volume was then measured using a computerised image analysis system. The system used consists of a stereomicroscope (Stemi 2000-C, Carl Zeiss, Jena, Germany) with a high-resolution digital camera (AxioCam, Carl Zeiss, Oberkochen, Germany) under control of KS400 3.0 software (Carl Zeiss, Hallbergmoos, Germany) in a PC computer. Images were analysed using KS400 software. Tumour height and width were measured at largest coronar section. Tumour volume was calculated using the formula for the ellipsoid (r1 × r2 × r3 × π × 4/3), where the radius in the sagittal plane was approximated to be the same as the coronal radius (Bergenheim et al, 1994).
Histological analysis of tumours
Ki-67 staining and proliferation index
Proliferation index was assessed after immunohistochemical staining for Ki-67 (Scholzen and Gerdes, 2000). Sections chosen for immunohistochemical staining were immersed in citrate buffer (pH 6.0) and irradiated in microwave oven for four cycles of 5 min. Endogenous peroxidase was blocked with 10% H2O2 in methanol for 15 min, followed by blocking with normal horse serum for 20 min. As primary antibody, a monoclonal anti-rat Ki-67, at 1 : 25 (MIB-5, clone M7248, DAKO A/S, Glostrup, Denmark) was incubated for 1 h at 37°C. After washing in PBS, sections were incubated with biotinylated secondary horse anti-mouse antibody for 30 min. Enzyme conjugate was subsequently added for 30 min. Staining reaction was developed in 3,3′-diaminobenzidine (DAB) (Sigma, Stockholm, Sweden) and mounted using gelatine–glycerol. Cells were manually counted in a standard light microscope (Axiophot, Carl Zeiss, Oberkochen, Germany) and at least 600 nuclei per tumour section were counted. Proliferation index was calculated as the fraction of Ki-67-positive nuclei.
Apoptosis
To visualise apoptosis, the Roche in situ cell death detection kit, based on the TUNEL technique (Roche Diagnostics Scandinavia AB, Bromma, Sweden), was used. Formalin-fixed, paraffin-embedded tissue sections were treated with proteinase K for 15 min at 37°C and blocked for endogenous peroxidase with 3% H2O2 in methanol for 10 min. Sections were then incubated for 60 min at 37°C in TUNEL reaction mixture, followed by a 30 min incubation with converter-POD (peroxidase). Finally, the staining reaction was developed in DAB (Sigma, Stockholm, Sweden) and sections were mounted using gelatine–glycerol. Cells were manually counted in standard light microscope (Axiophot, Carl Zeiss, Oberkochen, Germany) avoiding necrotic tumour areas. At least 600 nuclei per tumour section were counted. Apoptosis index was calculated as the fraction of positive stained nuclei.
Factor VIII staining and MVD
Vessels in the BT4C brain tumours were immunohistochemically stained for factor VIII and quantified manually using a method originally presented by Weidner (1993). Sections chosen for immunohistochemical staining were permeabilised in 0.1% protease at 37°C for 10 min. After blocking with normal goat sera, sections were incubated for 1 h at room temperature with a primary polyclonal rabbit anti-human factor VIII antibody (DAKO A/S, Glostrup, Denmark) diluted 1 : 400. After washing in PBS, sections were incubated with biotinylated secondary goat anti-rabbit antibody diluted 1 : 200. Endogenous peroxidase was blocked with 10% H2O2 in methanol for 15 min. Enzyme conjugate was then added for 30 min. The staining reaction was developed in DAB (Sigma, Stockholm, Sweden) and mounted using gelatine–glycerol. Assessment of MVD was performed by manual counting in selected areas with the highest vascular density (hot spots). Each tumour was scanned at low magnification and four hot spots were chosen. All stained objects (blood vessels with and without visible lumina) within a × 200 high-power field were counted using a standard light microscope (Axiophot, Carl Zeiss, Oberkochen, Germany). Each hot spot was counted twice and the arithmetical mean in each section was used to calculate the mean MVD for each tumour, which was used for further statistical analysis. Microvascular density was expressed as number of vessels/ × 200 high-power field (Johansson et al, 1999).
In vitro experiments
The nitrosourea induced rat glioma cell line BT4C, kindly provided by professor R Bjerkvig (Bergen, Norway), and the immortalised rat brain endothelial cell line RBE4 (Regina et al, 1998), kindly provided by Dr PO Couraud (Neurotech SA, Evry, France), were used for in vitro studies. For BT4C assays, cells were grown in cultures as monolayer in DMEM (Gibco, Paisley, Scotland), supplemented with 5% fetal calf serum. Cells were harvested and plated in a volume of 100 μl at 500 cells well−1 in microtitre plates. ZD6474 (0–15 μ M) was then added to the media. RBE4 cells were grown on calf-skin collagen-coated (Sigma, Stockholm, Sweden) surfaces and maintained in Ham's F10 (Gibco, Paisley, Scotland), supplemented with 5% fetal calf serum. Cells were harvested and plated in a volume of 100 μl at 1000 cells well−1 in microtitre plates. ZD6474 (0–10 μ M) was then added to the media. Cells were cultured until cell growth was exponential before ZD6474 was added to the media. Plates were incubated at 37°C for 6 days, and the medium was changed after 3 days. To quantify the cytotoxic effects of ZD6474, fluoroscein diacetate (FDA) was used in a fluorometric microculture cytotoxicity assay (FMCA) (Larsson et al, 1992). Cells were washed with PBS. PBS (100 μl) containing 10 mg l−1 FDA was added to each well and plates were incubated in 37° for 50 min, followed by fluorescence determination using 485 and 538 nm for excitation and emission, respectively.
Statistics
Values are expressed as median and range. Groups were compared using the Mann–Whitney U-test. For curve estimation, quadratic regression was used. For this purpose, the software SPSS 11.0 for Windows was used.
Results
Inhibition of tumour growth
In the BT4C rat model, oral administration of ZD6474 50 mg kg−1 once daily for 13 days significantly decreased tumour volume from 53 mm3 (range 17–82) to 18 mm3 (range 16–33) when compared to controls (P<0. 05) (Figure 2). The higher dose, ZD6474 100 mg kg−1 did not provide additional growth inhibitory effect, where tumour volume was 19 mm3 (range 7–29) (P<0.05 compared to controls), with reservation for the fact that the treatment time here was 1 day less.
Treatment with ZD6474 50 mg kg−1 resulted in significant inhibition of tumour growth from 53 (range 17–82) mm3 to 18 (range 16–33) mm3 compared with tumours in the control group (P=0.032). Treatment with ZD6474 100 mg kg−1 resulted in tumour volume 19 (range 7–29) mm3 (P=0.028 compared to controls). Two cases were excluded due to ‘no tumour take’.
Histopathological analysis of tumours
Treatment with ZD6474 50 mg kg−1 reduced the Ki-67 labelling index significantly. The proliferation index in the control group was 0.22 (range 0.15–0.28) compared to 0.14 (range 0.04–0.20) (P<0.05) and 0.15 (range 0.06–0.19) (P=NS, compared to controls) in the group treated with ZD6474 50 mg kg−1 and 100 mg kg−1, respectively (Figure 3). The apoptotic index was increased in the treated groups, with a value in the control group of 0.01 (range 0.01–0.02) compared to 0.03 (range 0.01–0.05) in the group treated with ZD6474 50 mg kg−1 (P<0.05), and 0.02 (range 0.01–0.03) (P<0.05 compared to controls), in the group treated with ZD6474 100 mg kg−1 (Figure 4). The MVD increased from 94 (range 79–117) to 111 (range 104–126) vessels per high-power field (P<0.05) in animals treated with ZD6474 50 mg kg−1 compared to controls (Figure 5). In the group treated with ZD6474 100 mg kg−1, the MVD was 112 (range 80–122) vessels per high-power field (P=NS compared to controls).
Proliferation index was measured by immunohistochemical staining for Ki-67. Treatment with ZD6474 resulted in reduced proliferation index from 0.22 (range 0.15–0.28) in the control group to 0.14 (range 0.04–0.2) (P=0.046) and 0.15 (range 0.06–0.19) (P=0.1 compared to controls) in the group treated with ZD6474 50 mg kg−1 and 100 mg kg−1, respectively.
Apoptosis index increased in treated groups. In the control group, apoptosis index was 0.01 (range 0.01–0.02). The group treated with ZD6474 50 mg kg−1 had an apoptosis index at 0.03 (range 0.01–0.05) (P=0.022), and in the group treated with 100 mg kg−1, the apoptosis index was 0.02 (range 0.01–0.03) (P=0.022 compared to controls).
Assessment of mean vessel count was performed after immunohistochemical staining for factor VIII. Treatment with ZD6474 50 mg kg−1 resulted in increased mean vessel count from 94 (range 79–117) to 111 (range 104–126) vessels per high-power field (P=0.032). The higher dose ZD6474 100 mg kg−1 resulted in a mean vessel count of 112 (range 80–122) vessels per high-power field (P=0.36 compared to controls).
Tolerability
In BD IX rats, once-daily oral administration of ZD6474 50 mg kg−1 for 13 days appeared well tolerated with no visible clinical signs. ZD6474 100 mg kg−1 for 12 days made animals lethargic and they lost significant weight (Figure 6). These animals developed diarrhoea (in some cases blood stained), and autopsy showed marked gastric stocking, signalling delayed gastric emptying. Haematological toxicity was not observed in the experiment. In the group receiving ZD6474 100 mg kg−1, the haematocrit and the haemoglobin level were slightly elevated, most likely due to dehydration. In all animals, leucocyte and trombocyte counts were unaffected.
Curves of relative weight among the different groups over time. There was no significant difference in weight between animals in the control group compared to the low-dose group. Animals in the group receiving ZD6474 100 mg kg−1 lost significantly in weight. As reported in Material and Methods, two animals in the high-dose group died before the experiment was ended (TS=treatment start, Sacrif=sacrifice).
In vitro results
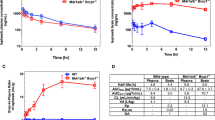
The ability of ZD6474 to inhibit cell growth directly was examined in vitro. ZD6474 significantly and dose dependently inhibited the growth of both BT4C and RBE4. IC50 values for inhibition of BT4C was 2.4 μ M (Figure 7), and for RBE4 2.3 μ M (Figure 8).
Discussion
In this study, we have demonstrated that the VEGFR tyrosine kinase inhibitor ZD6474 significantly inhibits the growth of an intracerebral rat glioma. This finding is novel and, at least to our knowledge, it is the first time growth inhibition of an orthotopic tumour has been reported after ZD6474 treatment. Increased apoptosis and decreased proliferation of tumour cells in treated animals was a finding consistent with the observed growth inhibition in ZD6474-treated animals. In vitro, decreased growth of tumour cells as well as of rat brain endothelial cells was observed, which further validates the in vivo effects.
Previously, it has been shown that ZD6474 inhibits VEGF signalling and tumour growth in a panel of subcutaneous experimental mouse tumours of different origin (Wedge et al, 2002). Growth reductions of 70–100% after ZD6474 50 mg kg−1 treatment were reported after 14–28 days of treatment. In our syngenic rat glioma model, growth was significantly inhibited and a tumour volume reduction of 66% was observed after 13 days of treatment with ZD6474 50 mg kg−1. The growth reduction observed in our orthotopic glioma model is therefore in accordance with previous reports in other tumour models. However, it must be emphasised that dose levels are not easily translated between different species, and to our knowledge there are no other reports on ZD6474 treatment in rat tumour models. The treatment effects in our intracerebral model also suggest that ZD6474 crosses the blood–tumour barrier and reaches target cells in clinically relevant concentrations. Recently, it has been shown that ZD6474 also has a significant activity in subcutaneous CNS tumour mouse xenografts (Rich et al, 2003). Another preliminary report indicates that ZD6474 is inhibiting tumour growth in a mouse model of brain metastasis (Leenders et al, 2003). These observations together with the present findings suggest that ZD6474 may be an interesting agent for further investigation in experimental and clinical neuro-oncology.
In the present study, increased apoptosis and decreased proliferation of tumour cells are distinct findings after ZD6474 treatment. The experience from other experimental antiangiogenic treatments is somewhat different. The fragment inhibitors angiostatin and endostatin are both considered to be mainly angiogenesis inhibitors without effects on proliferation of tumour cells (Sim, 1998). It is known that treatment with these angiogenesis inhibitors results in a characteristic pattern with increased tumour cell apoptosis and unaffected tumour cell proliferation (O'Reilly et al, 1996; 1997). The observation that ZD6474 also decreases tumour cell proliferation suggests that the inhibition of tumour growth is a result of more than inhibition of angiogenesis alone. This hypothesis is supported by our in vitro data where growth of rat brain endothelial cells and tumour cells both were inhibited at similar drug concentrations. Increased apoptosis after exposure to ZD6474 in vitro has been reported for different human cell lines (Ciardiello et al, 2003). However, in a human lung cancer xenograft (Calu-6), Wedge et al (2002) did not observe any change in apoptotic frequency after ZD6474 treatment. In their study, a marked increase in tumour necrosis was reported, suggesting that the antiangiogenic effects are more prominent in this model compared to ours. The literature on the effects of ZD6474 on cell kinetics is so far limited and to our knowledge our study is the first to report an increase in tumour cell apoptosis in vivo after ZD6474 treatment.
Proliferation of rat brain endothelial cells was dose-dependently decreased after ZD6474 treatment in vitro in our study. This has earlier been reported for human umbilical vein endothelial cells (HUVEC) (Wedge et al, 2002) and the effects of ZD6474 on endothelial cells are so far undisputed. However, in our study, RBE4 cells appear to be more resistant to ZD6474 treatment with an IC50 more than 30-fold higher than for VEGF-stimulated HUVEC cells, as reported by Wedge et al, 2002. The explanation for this difference may be that the endothelial cells in the present study were grown in serum-containing media and not stimulated by VEGF alone. Another explanation may be that brain-derived endothelial cells are more resistant to ZD6474 treatment compared to HUVEC cells derived from human umbilical cord.
The effects of ZD6474 on rat brain endothelial cells in vitro could not be translated to a decrease in MVD in vivo in the present study. Instead, we observed a slight increase in MVD after treatment with ZD6474 in the BT4C rat glioma model. This result was somewhat unsuspected since it may be assumed that successful antiangiogenic treatment reduces the number of tumour blood vessels. Moreover, vessel density in intradermally transplanted A549 human lung cancer xenografts decreased after ZD6474 treatment (Wedge et al, 2002). In a recent report, acute changes in tumour perfusion and permeability were observed in vivo, after treatment with ZD6474, using dynamic contrast-enhanced MRI (Checkley et al, 2003). Together with the in vitro data on rat brain endothelial cells and previous reports, it appears obvious that ZD6474 has the ability to reduce endothelial cell growth in vivo. The lack of correlation of treatment effect to a decrease in MVD in the present study may be discussed in several ways. From a biological point of view, vascularisation differs widely between tumour types and models. Microvascular density is also a time-dependent measure and the impact of MVD as a surrogate marker for antiangiogenic therapy response may therefore be discussed. In a review by Hlatky et al (2002), MVD as an indicator for antiangiogenic treatment efficacy is questioned. It is stated that MVD may fluctuate during antiangiogenic treatment and it may be assumed that an effective antiangiogenic treatment initially may decrease vessel density and later during the course of treatment a stable state or even an increase in MVD may be predicted as tumour cells drop out. Effects on the vascular component are not independent from effects on the tumour cell compartment and MVD may mainly reflect the ratio of the vascular and tumour cell components. From a methodological point of view, the assessment of MVD is difficult and differences in methodological approaches may also reflect the discrepancy between the present study and the previous report by Wedge et al (2002). Therefore, the observed MVD increase in this study does not rule out the possibility that the tumour growth inhibitory effect seen is at least partly due to antiangiogenic effects.
The importance of growth factor stimulation in the progression of malignant glioma is unambiguous. Among angiogenesis factors, VEGF is commonly believed to be the most important positive regulator of angiogenesis in malignant glioma (Machein and Plate, 2000; Mentlein and Held-Feindt, 2003). Hypoxic tumour cells express VEGF and thereby stimulate tumour angiogenesis, one of the hallmarks of high-grade glioma (Plate et al, 1992). In the BT4C rat glioma, VEGF is strongly expressed in the invasive tumour border (Lindgren et al, 1997). Epidermal growth factor receptor and its main ligands EGF and transforming growth factor alpha (TGFα) are commonly overexpressed in malignant glioma (Dunn et al, 2000). The rationale to target the VEGF and EGF axis therefore seems obvious in malignant glioma. ZD6474 is designed as an inhibitor of VEGFR-2, but has recently been demonstrated to display additional inhibitory effects on EGFR (Wedge et al, 2002; Ciardiello et al, 2003). Our in vitro data show that the inhibitory effects of ZD6474 on tumour cells did not differ from the effects on endothelial cells in vitro, and that proliferation of tumour cells in vivo was decreased. This might suggest that the BT4C tumour growth inhibition at least partly involves direct antiproliferative effects, possibly through EGFR inhibition. Further analysis of the expression of growth factors and their receptors from the tumour is required to establish the precise inhibitory mechanisms in this specific tumour model.
The use of tyrosine kinase inhibitors in the clinical setting has so far displayed beneficial effects in a subpopulation of patients with solid tumours. Imatinib (STI571), a receptor tyrosine kinase inhibitor with effects on the bcr-abl tyrosine kinase, platelet-derived growth factor receptor (PDGFR) and c-KIT is now standard treatment in patients with chronic myeloid leukaemia and the rare gastrointestinal stromal tumours (GIST) (Druker et al, 2001; Demetri et al, 2002). The EGFR tyrosine kinase inhibitor gefitinib (ZD1839) displays activity in several tumours and significant responses and survival benefit in previously treated lung cancer patients are reported (Johnson, 2003). Several other receptor tyrosine kinase inhibitors are under development and in early clinical testing (Bonomi, 2003). However, so far no major contribution has been made from receptor tyrosine kinase inhibitors, besides imatinib for the rare GIST patients, in the treatment of solid tumours. One possible explanation is that the plethora of growth factors active in cancer makes the tumour growth unaffected when only one of the signalling pathways is blocked. The possibility to block transduction of two different pathways stimulating different cell compartments makes ZD6474 interesting for further evaluation in malignant glioma.
To summarise, ZD6474 exerts significant antitumour effects in an intracerebral glioma model with effects on both endothelial and tumour cells. Thus, treatment with ZD6474 could be a novel approach for simultaneous inhibition of both the endothelial cell and the tumour cell components of malignant glioma. The promising experimental results merit ZD6474 for further evaluation in the treatment of malignant glioma.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abdulrauf SI, Edvardsen K, Ho KL, Yang XY, Rock JP, Rosenblum ML (1998) Vascular endothelial growth factor expression and vascular density as prognostic markers of survival in patients with low-grade astrocytoma. J Neurosurg 88: 513–520
Aprelikova O, Pajusola K, Partanen J, Armstrong E, Alitalo R, Bailey SK, McMahon J, Wasmuth J, Huebner K, Alitalo K (1992) FLT4, a novel class III receptor tyrosine kinase in chromosome 5q33-qter. Cancer Res 52: 746–748
Bergenheim A, Elfversson J, Gunnarsson P-O, Edman K, Hartman M, Henriksson R (1994) Cytotoxic effect and uptake of estramustine in a rat glioma model. Int J Oncol 5: 293–299
Bonomi P (2003) Clinical studies with non-iressa EGFR tyrosine kinase inhibitors. Lung Cancer 41 (Suppl 1): S43–S48, doi: 10.1016/S0169-5002(03)00141-7
Checkley D, Tessier JJ, Kendrew J, Waterton JC, Wedge SR (2003) Use of dynamic contrast-enhanced MRI to evaluate acute treatment with ZD6474, a VEGF signalling inhibitor, in PC-3 prostate tumours. Br J Cancer 89: 1889–1895, doi:10.1038/sj.bjc.6601386
Ciardiello F, Caputo R, Damiano V, Troiani T, Vitagliano D, Carlomagno F, Veneziani BM, Fontanini G, Bianco AR, Tortora G (2003) Antitumor effects of ZD6474, a small molecule vascular endothelial growth factor receptor tyrosine kinase inhibitor, with additional activity against epidermal growth factor receptor tyrosine kinase. Clin Cancer Res 9: 1546–1556
Ciardiello F, Tortora G (2001) A novel approach in the treatment of cancer: targeting the epidermal growth factor receptor. Clin Cancer Res 7: 2958–2970
Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S, Janicek M, Fletcher JA, Silverman SG, Silberman SL, Capdeville R, Kiese B, Peng B, Dimitrijevic S, Druker BJ, Corless C, Fletcher CD, Joensuu H (2002) Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med 347: 472–480, doi:10.1056/NEJMoa020461
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM, Lydon NB, Kantarjian H, Capdeville R, Ohno-Jones S, Sawyers CL (2001) Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 344: 1031–1037, doi: 10.1056/NEJM200104053441401
Dunn IF, Heese O, Black PM (2000) Growth factors in glioma angiogenesis: FGFs, PDGF, EGF, and TGFs. J Neurooncol 50: 121–137, doi:10.1023/A:1006436624862
Dvorak HF (2002) Vascular permeability factor/vascular endothelial growth factor: a critical cytokine in tumor angiogenesis and a potential target for diagnosis and therapy. J Clin Oncol 20: 4368–4380, doi:10.1200/JCO.2002.10.088
Feldkamp MM, Lau N, Rak J, Kerbel RS, Guha A (1999) Normoxic and hypoxic regulation of vascular endothelial growth factor (VEGF) by astrocytoma cells is mediated by Ras. Int J Cancer 81: 118–124, doi:10.1002/(SICI)10970215(19990331)81:1<118::AID-IJC20>3.0.CO;2–5
Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9: 669–676, doi:10.1038/nm0603-669
Hennequin LF, Stokes ES, Thomas AP, Johnstone C, Ple PA, Ogilvie DJ, Dukes M, Wedge SR, Kendrew J, Curwen JO (2002) Novel 4-anilinoquinazolines with C-7 basic side chains: design and structure activity relationship of a series of potent, orally active, VEGF receptor tyrosine kinase inhibitors. J Med Chem 45: 1300–1312, doi:10.1021/jm011022e
Hlatky L, Hahnfeldt P, Folkman J (2002) Clinical application of antiangiogenic therapy: microvessel density, what it does and doesn't tell us. J Natl Cancer Inst 94: 883–893
Johansson M, Bergenheim AT, Widmark A, Henriksson R (1999) Effects of radiotherapy and estramustine on the microvasculature in malignant glioma. Br J Cancer 80: 142–148, doi:10.1023/A:1006436624862
Johansson M, Henriksson R, Bergenheim AT, Koskinen LO (2000) Interleukin-2 and histamine in combination inhibit tumour growth and angiogenesis in malignant glioma. Br J Cancer 83: 826–832, doi:10.1054/bjoc.2000.1354
Johnson DH (2003) Gefitinib (Iressa) trials in non-small cell lung cancer. Lung Cancer 41 (Suppl 1): S23–S28, doi:10.1016/S0169-5002(03)00136-3
Larsson R, Kristensen J, Sandberg C, Nygren P (1992) Laboratory determination of chemotherapeutic drug resistance in tumor cells from patients with leukemia, using a fluorometric microculture cytotoxicity assay (FMCA). Int J Cancer 50: 177–185
Leenders W, Kusters B, Verrijp K, Maass C, Heerschap A, Ruiter D, Ryan A (2003) Waal de R implications of anti-angiogenic treatment with ZD6474, a potent and selective VEGF receptor tyrosine kinase inhibitor, for tumor behavior in a mouse model of brain metastasis. Proceedings from AACR 2003, Abstract no.: 37
Leon SP, Folkerth RD, Black PM (1996) Microvessel density is a prognostic indicator for patients with astroglial brain tumors. Cancer 77: 362–372, doi:10.1002/(SICI)1097-0142(19960115)77:2<362::AID-CNCR20>3.0.CO;2-Z
Lindgren M, Johansson M, Sandstrom J, Jonsson Y, Bergenheim AT, Henriksson R (1997) VEGF and tPA co-expressed in malignant glioma. Acta Oncol 36: 615–618
Machein MR, Plate KH (2000) VEGF in brain tumors. J Neurooncol 50: 109–120, doi:10.1023/A:1006416003964
Mentlein R, Held-Feindt J (2003) Angiogenesis factors in gliomas: a new key to tumour therapy? Naturwissenschaften 90: 385–394, doi:10.1007/s00114-003-0449-9
O'Reilly MS, Boehm T, Shing Y, Fukai N, Vasios G, Lane WS, Flynn E, Birkhead JR, Olsen BR, Folkman J (1997) Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell 88: 277–285, doi:10.1016/S00928674(00)81848-6
O'Reilly MS, Holmgren L, Chen C, Folkman J (1996) Angiostatin induces and sustains dormancy of human primary tumors in mice. Nat Med 2: 689–692
Plate KH, Breier G, Weich HA, Risau W (1992) Vascular endothelial growth factor is a potential tumour angiogenesis factor in human gliomas in vivo. Nature 359: 845–848, doi:10.1038/359845a0
Regina A, Koman A, Piciotti M, El Hafny B, Center MS, Bergmann R, Couraud PO, Roux F (1998) Mrp1 multidrug resistance-associated protein and P-glycoprotein expression in rat brain microvessel endothelial cells. J Neurochem 71: 705–715
Rich JN, Keir ST, Wheeler C, Reardon DA, Bigner DD, Friedman HS 2003 ZD6474, a vascular endothelial growth factor recepor 2 (VEGFR-2) inhibitor, inhibits central nervous system tumor growth following oral administration. Proceedings from AACR, (Abstract no. 48)
Scholzen T, Gerdes J (2000) The Ki-67 protein: from the known and the unknown. J Cell Physiol 182: 311–322, doi:10.1002/(SICI)10974652(200003)182:3<311∷AID-JCP1>3.0.CO;2–9
Sim BK (1998) Angiostatin and endostatin: endothelial cell-specific endogenous inhibitors of angiogenesis and tumor growth. Angiogenesis 2: 37–48, doi:10.1023/A:1009050309715
Wedge SR, Ogilvie DJ, Dukes M, Kendrew J, Chester R, Jackson JA, Boffey SJ, Valentine PJ, Curwen JO, Musgrove HL, Graham GA, Hughes GD, Thomas AP, Stokes ES, Curry B, Richmond GH, Wadsworth PF, Bigley AL, Hennequin LF (2002) ZD6474 inhibits vascular endothelial growth factor signaling, angiogenesis, and tumor growth following oral administration. Cancer Res 62: 4645–4655
Weidner N (1993) Tumor angiogenesis: review of current applications in tumor prognostication. Semin Diagn Pathol 10: 302–313
Workman P, Twentyman P, Balkwill F, Balmain A, Chaplin D, Double J, Embleton J, Newell D, Raymond R, Stables J, Stephens T, Wallace J (1998) United Kingdom Co-ordinating Committee on Cancer Research (UKCCCR) guidelines for the welfare of animals in experimental neoplasia (Second Edition). Br J Cancer 77: 1–10
Yamada Y, Nezu J, Shimane M, Hirata Y (1997) Molecular cloning of a novel vascular endothelial growth factor, VEGF-D. Genomics 42: 483–488, doi:10.1006/geno.1997.4774
Acknowledgements
This work was supported by grants from the Swedish Society Against Cancer and Lion's Cancer Research Foundation, Umeå University, Sweden. Kerstin Bergh and Sigrid Kilter are acknowledged for skilful technical assistance and Britt-Inger Gladzki for taking great care of the animals. We also thank Björn Tavelin for statistical help and advice. We appreciate the comments on the manuscript by Dr Anderson Ryan, Astra Zeneca, UK. Preliminary parts of this study were presented at the ‘15th International Conference on Brain Tumour Research and Therapy’ in Sorrento, Italy, May 2003.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Sandström, M., Johansson, M., Andersson, U. et al. The tyrosine kinase inhibitor ZD6474 inhibits tumour growth in an intracerebral rat glioma model. Br J Cancer 91, 1174–1180 (2004). https://doi.org/10.1038/sj.bjc.6602108
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602108
Keywords
This article is cited by
-
MRI-Based Characterization of Vascular Disruption by 5,6-Dimethylxanthenone-Acetic Acid in Gliomas
Journal of Cerebral Blood Flow & Metabolism (2009)
-
Mechanisms of Disease: temozolomide and glioblastoma—look to the future
Nature Clinical Practice Oncology (2008)
-
Effects of the VEGFR inhibitor ZD6474 in combination with radiotherapy and temozolomide in an orthotopic glioma model
Journal of Neuro-Oncology (2008)