Abstract
A score based on the combination of the systemic inflammatory response and albumin hazards ratio (HR) 1.70, 95% CI 1.23 – 2.35, P=0.001) was comparable in prognostic value to that based on stage and performance status (HR 1.48, 95% CI 1.12 – 1.95, P=0.006) in patients with inoperable non-small-cell lung cancer. The former is simple to measure and well standardised.
Similar content being viewed by others
Main
Non-small-cell lung cancer is the most common cause of cancer death in North America and Western Europe. Most patients present with advanced inoperable disease and consequently the prognosis of these patients is extremely poor. Conventionally, the selection of patients for active or supportive treatment has been based on clinicopathological criteria, including age, stage, performance status, weight-loss or hypoalbuminaemia (Numico et al, 2001). However, the assessment of both performance status and the presence of weight loss may be subjective. For example, significant differences in the assessment of performance status have been reported between oncologists, nurses and patients, oncologists being the most optimistic in their assessment and patients the least (Ando et al, 2001).
Recent studies have shown that the presence and the magnitude of a systemic inflammatory response, as evidenced by increased circulating concentrations of C-reactive protein, is a prognostic factor independent of age, stage, performance status, weight-loss and hypoalbuminaemia in patients with advanced cancer including non-small-cell lung cancer (NSCLC) (Martin et al, 1999; O'Gorman et al, 2000; Mahmoud and Rivera, 2002; Scott et al, 2002).
The aim of the present study was to assess the value of combining C-reactive protein and recognised prognostic factors as stage, performance status and hypoalbuminaemia to form new prognostic scores for patients with inoperable NSCLC.
Materials and methods
Study design
Patients presenting with inoperable NSCLC (stages III and IV) to a single multidisciplinary oncology clinic in Glasgow Royal Infirmary between January 1997 and October 2002 were included in the study. Information was abstracted from the case notes by a specially trained research nurse (LMF). Data for 1997–1999 were collected retrospectively and that for 2000–2002 prospectively. All patients had cytologically or histologically confirmed disease and were staged on the basis of clinical findings, chest X-ray, and where appropriate, bronchoscopy, liver ultrasound, isotope bone scan and computerised tomography of the thorax, according to the American Thoracic Society TNM classification (Mountain, 1991).
Clinical stage, tumour type and performance status (Eastern Cooperative Oncology Group, ECOG) were recorded at the time of diagnosis. A blood sample was also obtained for measurement of haemoglobin, white cell count, albumin and C-reactive protein concentrations. Patients were considered to have undergone active treatment if they received chemotherapy (mainly cisplatin based) and/or radical radiotherapy. Patients receiving palliative radiotherapy and/or palliative care (symptom control) were considered to have had supportive treatment.
The study was approved by the Research Ethics Committee of Glasgow Royal Infirmary.
Methods
Blood parameters
Routine laboratory measurements of haemoglobin, white cell count, albumin and C-reactive protein concentration were carried out. The coefficient of variation for these methods, over the range of measurement, was less than 5% as established by routine quality control procedures.
Statistics
Data are presented as median and range. Grouping of the variables age, tumour type, performance status (ECOG), haemoglobin, white cell count and albumin was carried out using standard thresholds (Paesmans et al, 1997; Herndon et al, 1999). C-reactive protein concentrations were also grouped (⩽10/>10 mg l−l) as previously described (O'Gorman et al, 2000). Prognostic scores were constructed by assigning one point for each of the following criteria: stage IV, ECOG 2–4, albumin <35 g l−l and C-reactive protein >10 mg l−l. Cumulative scores were obtained by combining C-reactive protein with each of the other variables.
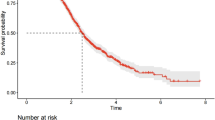
Univariate survival analysis was performed using the Kaplan–Meier method. Multivariate survival analysis and calculation of hazard ratios (HR) were performed using the Cox regression analysis with prognostic scores as covariates. Deaths up to 31 January 2003 were included in the analysis. Analysis was performed using SPSS software (SPSS Inc., Chicago, IL, USA).
Results
The characteristics of patients with inoperable NSCLC (n=161) are shown in Table 1. The majority were male, over the age of 60 years, had stage IV disease and had good performance status. Approximately, 20% had hypoalbuminaemia and 80% had an elevated C-reactive protein concentration. One-third of patients received active treatment (64% received cisplatin-based chemotherapy); the remaining patients received supportive treatment.
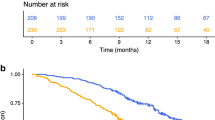
In all, 118 (73%) of patients died during the follow-up period. On univariate survival analysis, stage (P<0.05), tumour type (P<0.01), performance status (P<0.001), white cell count (P<0.01), albumin (P<0.001) and C-reactive protein (P<0.01) were significant predictors of survival. On multivariate survival analysis all these variables, with the exception of white cell count, remained independent significant predictors of survival. There was a significant correlation between C-reactive protein and albumin concentrations (rs=−0.443, P<0.001).
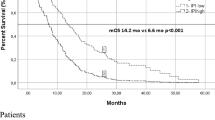
On univariate analysis, the relationship between the prognostic scores based on the combinations of C-reactive protein with stage, performance status and albumin, respectively, and the median survival is shown in Table 2. All these prognostic scores had HR in the range 1.7–2.0 which was comparable with that for the score based on the combination of stage and performance status.
On multivariate analysis, when the three scores based on the combinations of the systemic inflammatory response and stage, performance status and albumin were compared with the combination of stage and performance status, only the score based on the combination of the systemic inflammatory response and albumin (HR 1.70, 95% CI 1.23–2.35, P=0.001) and the score based on stage and performance status (HR 1.48, 95% CI 1.12–1.95, P=0.006) retained independent significance.
Discussion
In the present study, both the established indicators of the presence of a systemic inflammatory response, white cell count and C-reactive protein, were predictive of survival in patients with inoperable NSCLC. This is consistent with previous studies, which have shown that a raised white cell count (Paesmans et al, 1997) and C-reactive protein concentrations (Scott et al, 2002), have prognostic value, independent of stage, in patients with inoperable NSCLC.
When C-reactive protein concentrations were combined with stage, performance status and albumin to form new prognostic scores, these combined scores improved the prediction of survival based on stage, performance status or albumin alone. Indeed, in each of the cumulative scores, the presence of an elevated C-reactive protein was associated with a halving of survival. Furthermore, when these three combinations were compared to the conventional combination of stage and performance status, the combination of the systemic inflammatory response and albumin and the conventional clinical combination stage and performance status were found to have comparable prognostic value. To our knowledge, this is the first study to present a cumulative prognostic score based on C-reactive protein and albumin in patients with advanced NSCLC.
In the present study, there was a significant difference in survival between those receiving active treatment and those receiving palliative care. However, this is not surprising since those selected for active treatment tend to be the fitter patients. Indeed, in the present study, 50% of patients with good performance status (ECOG 1–2) and 14% of those with poor performance status (ECOG 3–4) received active treatment. Treatment was not included in the prognostic model since the selection of patients for active treatment is based primarily on performance status.
These results are consistent with the evidence that chronic activation of the systemic inflammatory response is detrimental to the outcome of patients with NSCLC, being associated with an increase in weight loss (Staal van den Brekel et al, 1995; Scott et al, 1996) and fatigue (Scott et al, 2003), loss of lean tissue (McMillan et al, 1998; Simons et al, 1999), decreased performance status and survival (Martin et al, 1999; Scott et al, 2002).
The mechanism by which a systemic inflammatory response is evoked in patients with NSCLC is not clear. One possibility is that since many patients have coexisting pulmonary infection, the resultant increase in white blood cells would lead to increased proinflammatory cytokine release and a subsequent increase in circulating C-reactive protein concentrations. However, in this study, although the white cell count was significantly correlated with C-reactive protein concentrations, the magnitude of the relationship was small (r2 less than 15%). This would suggest that infection was not the main stimulus to the increased C-reactive protein concentrations.
An alternative explanation would be that proinflammatory cytokines are produced by the tumour. Indeed, there is evidence that proinflammatory cytokines are produced locally by tumours in patients with NSCLC (Arias-Diaz et al, 1994). In particular, interleukin-6 is recognised as a primary mediator of increased C-reactive protein concentrations in these patients (Yanagawa et al, 1995; Scott et al, 1996). However, whether interleukin-6 is produced directly by lung cancer cells remains unclear.
In conclusion, the results of the present study suggest that a cumulative score based on C-reactive protein and albumin may have prognostic value similar to that provided by more conventional measures. However, the cumulative score based on C-reactive protein and albumin has the advantage that of being simple to measure, routinely available and well standardised. Further large-scale prospective studies are required to confirm these findings and establish its value as a guide to the selection of patients for treatment.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ando M, Ando Y, Hasegawa Y, Shimokata K, Minami H, Wakai K, Ohno Y, Sakai S (2001) Prognostic value of performance status assessed by patients themselves, nurses, and oncologists in advanced non-small cell lung cancer. Br J Cancer 85: 1634–1639
Arias-Diaz J, Vara E, Torres-Melero J, Garcia C, Baki W, Ramirez-Armengol JA, Balibrea JL (1994) Nitrite/nitrate and cytokine levels in bronchoalveolar lavage fluid of lung cancer patients. Cancer 74: 1546–1551
Herndon II JE, Fleishman S, Kornblith AB, Kosty M, Green MR, Holland J (1999) Is quality of life predictive of the survival of patients with advanced nonsmall cell lung carcinoma? Cancer 85: 333–340
Mahmoud FA, Rivera NI (2002) The role of C-reactive protein as a prognostic indicator in advanced cancer. Curr Oncol Rep 4: 250–255
Martin F, Santolaria F, Batista N, Milena A, Gonzalez-Reimers E, Brito MJ, Oramas J (1999) Cytokine levels (IL-6 and IFN-gamma) acute phase response and nutritional status as prognostic factors in lung cancer. Cytokine 11: 80–86
McMillan DC, Scott HR, Watson WS, Preston T, Milroy R, McArdle CS (1998) Longitudinal study of body cell mass depletion and the inflammatory response in cancer patients. Nutr Cancer 31: 101–105
Mountain CF (1991) A new international staging system for lung cancer. Chest 89(Suppl 4): 225s–233s
Numico G, Russi E, Merlano M (2001) Best supportive care in non-small cell lung cancer: is there a role for radiotherapy and chemotherapy? Lung Cancer 32: 213–226
O'Gorman P, McMillan DC, McArdle CS (2000) Prognostic factors in advanced gastrointestinal cancer patients with weight loss. Nutr Cancer 37: 36–40
Paesmans M, Sculier JP, Libert P, Bureau G, Dabouis G, Thiriaux J, Michel J, Van Cutsem O, Sergysels R, Mommen P, Klastersky J (1997) Response to chemotherapy has predictive value for further survival of patients with advanced non-small cell lung cancer: 10 years experience of the European Lung Cancer Working Party. Eur J Cancer 33: 2326–2332
Scott HR, McMillan DC, Crilly A, McArdle CS, Milroy R (1996) The relationship between weight loss and interleukin 6 in non-small-cell lung cancer. Br J Cancer 73: 1560–1562
Scott HR, McMillan DC, Brown DJF, Forrest LM, McArdle CS, Milroy R (2003) A prospective study of the impact of weight loss and the systemic inflammatory response on quality of life in patients with inoperable non-small cell lung cancer. Lung Cancer 40: 295–299
Scott HR, McMillan DC, Forrest LM, Brown DJF, McArdle CS, Milroy R (2002) The systemic inflammatory response, weight loss, performance status and survival in patients with inoperable non-small cell lung cancer. Br J Cancer 87: 264–267
Simons JP, Schols AM, Buurman WA, Wouters EF (1999) Weight loss and low body cell mass in males with lung cancer: relationship with systemic inflammation, acute-phase response, resting energy expenditure, and catabolic and anabolic hormones. Clin Sci (Lond) 97: 215–223
Staal-van den Brekel AJ, Dentener MA, Schols AM, Buurman WA, Wouters EF (1995) Increased resting energy expenditure and weight loss are related to a systemic inflammatory response in lung cancer patients. J Clin Oncol 13: 2600–2605
Yanagawa H, Sone S, Takahashi Y, Haku T, Yano S, Shinohara T, Ogura T (1995) Serum levels of interleukin-6 in patients with lung cancer. Br J Cancer 71: 1095–1098
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Forrest, L., McMillan, D., McArdle, C. et al. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer 89, 1028–1030 (2003). https://doi.org/10.1038/sj.bjc.6601242
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601242
Keywords
This article is cited by
-
Prognostic potential of nutritional risk screening and assessment tools in predicting survival of patients with pancreatic neoplasms: a systematic review
Nutrition Journal (2024)
-
Novel tumor marker index using carcinoembryonic antigen and carbohydrate antigen 19-9 is a significant prognostic factor for resectable colorectal cancer
Scientific Reports (2024)
-
Glasgow prognostic score for assessing the efficacy of whole-brain radiation therapy in cases of recursive partitioning analysis class 2 and class 3 multiple brain metastases: a retrospective study
Acta Neurologica Belgica (2024)
-
Biomarker analysis for patients with pancreatic cancer treated with nanoliposomal irinotecan plus 5-fluorouracil/leucovorin
BMC Cancer (2023)
-
The effect of zingiber officinale on prooxidant-antioxidant balance and glycemic control in diabetic patients with ESRD undergoing hemodialysis: a double-blind randomized control trial
BMC Complementary Medicine and Therapies (2023)