Abstract
It is generally considered that most cancers arise following the accumulation of several genetic events and that as a consequence its incidence increases with age. We report a cytogenetic subgroup of acute myeloid leukaemia whose incidence is independent of age. This observation indicates that acute myeloid leukaemia can develop via multiple pathways, and underlines the importance of cytogenetics in understanding this disease.
Similar content being viewed by others
Main
Cytogenetically-defined subtypes of acute myeloid leukaemia (AML) have distinct pathological and clinical features. In addition, many chromosomal abnormalities are important indicators of prognosis and are used to determine treatment strategies (Wheatley et al, 1999). Although, the link between cytogenetics and aetiology in AML remains uncertain some supporting evidence does exist. The main two cytogenetic subtypes seen in therapy-related leukaemia – 11q23 abnormalities and loss of 5q/7q – are closely associated with prior therapy with DNA topoisomerase II inhibitors and alkylating agents, respectively (Felix, 1998). Unfortunately, the results from the few studies investigating a link between smoking, alcohol, organic chemicals, pesticides and cytogenetic subgroups have been less convincing and are often contradictory (Crane et al, 1989; Sandler et al, 1993; Crane et al, 1996).
We, and others, have reported distinct age distribution profiles for AML patients with certain chromosomal abnormalities (IWCL4, 1984; Keating et al, 1987; Mauritzson et al, 1999; Moorman et al, 2001). Age is an important factor to be considered when investigating the aetiology of a disease as it can provide clues to its pathogenesis. The exponential increase in cancer incidence with age was fundamental to the development of the multi-stage theory of carcinogenesis because the probability of accumulating the full set of mutations required to effect malignant transformation increases with time (Armitage and Doll, 1954). In order to examine more closely the relationship between age and cytogenetics we have estimated the age-specific incidences rates of the principal cytogenetic subgroups seen in AML.
Patients and methods
This study was based on cases with de novo AML recruited to a population-based case–control study of acute leukaemia (Kane et al, 1999). Briefly, the study ascertained adults (16–69 years old) diagnosed with acute leukaemia over a 5-year period in two regions of England. The Northern region consisted of the former Yorkshire Regional Health Authority and the counties of Lancashire and Cumbria. The Southern region was defined as the then regional health authorities of the South West and Wessex. Case ascertainment started in April 1991 and ended in March 1996 in the Northern region and in December 1996 in the Southern region. The current analysis has been restricted to patients with a pathologically confirmed diagnosis of de novo AML.
Diagnostic cytogenetic data were collected from regional laboratories and classified as previously described (Moorman et al, 2001). Cytogenetic analysis was considered successful if an abnormal clone or 10 normal metaphases were observed, otherwise it was classified as failed. Successful cases were classified hierarchically according to the type of the primary chromosomal abnormality into one of four karyotype groups: (1) translocations (including inversions and insertions); (2) deletions (including monosomies); (3) trisomies (including duplications); and (4) no abnormality detected (NAD). In addition, those cases with a chromosomal abnormality were also classified hierarchically according to the presence of the five most frequently observed specific aberrations: t(15;17)(q22;q12), t(8;21)(q22;q22), inv(16)(p13q22), del(5q)/−5/del(7q)/−7 and +8. Other abnormalities occurred too infrequently to be considered separately and were therefore grouped together under the ‘other’ heading.
The population resident within the study area was assumed to be stable during the study period and was estimated using 1991 UK census data, obtained from Manchester Information and Associated Services at the University of Manchester. Using age-specific population figures, the number of person-years in each region was calculated and summed to give the number of person-years in each age group. The study population was estimated at 7.8 million people, giving a total of 42.5 million person-years. Age-specific incidence rates were estimated (per million) by dividing the number of cases in each cytogenetic group by the number of person-years at risk. As AML is a rare disease the number of cases were not subtracted from the total.
Results
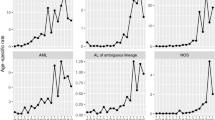
Of the 779 cases diagnosed with de novo AML 593 (76%) had a cytogenetic result, while 34 (4%) failed and 152 (20%) were not tested. Overall, the incidence of de novo AML increased with age – rising from <10 per million among those aged 16–29 years to >40 per million among those aged 60–69 years (Table 1). This pattern was observed for some but not all the cytogenetic subgroups investigated (Table 1, Figure 1). For example, the age-specific incidence rates for the deletion and normal karyotype groups as well as the 5q/7q group rose sharply with increasing age especially among the older two age groups. Although the incidence rates for the remaining three subgroups – trisomy, +8 and ‘other’ – also increased with age the rise was not as sharp and was confined to the oldest age group. The most notable exceptions to this pattern were the translocation karyotype group and the three specific translocations – t(15;17), t(8;21) and inv(16), whose incidence rates remained static across the different age groups.
Discussion
Our findings suggest that while the overall incidence of AML increases with age, the incidence of ‘translocation-positive’ AML does not increase with age. A recent study which showed that the incidence rate of acute promyelocytic leukaemia (which is synonymous with t(15;17)) is constant with age supports these findings (Vickers et al, 2000). It is generally assumed that cancer incidence increases with age because of the time required to accumulate the requisite number of mutations to effect malignant transformation. Armitage and Doll (1954) estimated that six or seven mutations would be required to produce the age distributions observed in their study. The age distribution of ‘translocation-positive’ AML clearly does not fit this model as its incidence is roughly constant between the ages of 16 and 69. Although we cannot calculate the actual number of mutations required to produce ‘translocation-positive’ AML from such an observation, it is reasonable to conclude that only one ‘rate-limiting’ step is required. Moreover, we can infer that there are at least two separate aetiological pathways which can give rise to AML. Therefore, studies investigating the causes AML should, where possible, assess the impact of cytogenetics on their findings.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Armitage P, Doll R (1954) The age distribution of cancer and a multi-stage theory of carcinogenesis. Br J Cancer 8: 1–12
Crane MM, Keating MJ, Trujillo JM, Labarthe DR, Frankowski RF (1989) Environmental exposures in cytogenetically defined subsets of acute nonlymphocytic leukemia. JAMA 262: 634–639
Crane MM, Strom SS, Halabi S, Berman EL, Fueger JJ, Spitz MR, Keating MJ (1996) Correlation between selected environmental exposures and karyotype in acute myelocytic leukemia. Cancer Epidemiol Biomarkers Prev 5: 639–644
Felix CA (1998) Secondary leukemias induced by topoisomerase-targeted drugs. Biochim Biophys Acta – Gene Structure and Expression 1400: 233–255
IWCL4 (1984) The Fourth International Workshop on Chromosomes in Leukemia: A prospective study of acute nonlymphocytic leukemia. Cancer Genet Cytogenet 11: 249–360
Kane EV, Roman E, Cartwright RA, Parker J, Morgan GJ (1999) Tobacco and the risk of acute leukaemia in adults. Br J Cancer 81: 1228–1233
Keating MJ, Cork A, Broch Y, Smith T, Waltes RS, McCredie KB, Trujillo J, Freireich EJ (1987) Towards a clinically relevant cytogenetic classification of acute myelogeonous leukaemia. Leuk Res 11: 119–133
Mauritzson N, Johansson B, Albin M, Billstrom R, Ahlgren T, Mikoczy Z, Nilsson PG, Hagmar L, Mitelman F (1999) A single center population based consecutive series of 1500 cytogenetically investigated adult hematological malignancies: karyotypic features in relation to morphology, age and gender. Eur J Haematol 62: 95–102
Moorman AV, Roman E, Kane EV, Dovey GJ, Cartwright RA, Morgan GJ (2001) Karyotype and age in acute myeloid leukaemia: Are they linked? Cancer Genet Cytogenet 126: 155–161
Sandler DP, Shore DL, Anderson JR, Davey FR, Arthur D, Mayer RJ, Silver RT, Weiss RB, Moore JO, Schiffer CA, Wurster-Hill DH, McIntyre OR, Bloomfield CD (1993) Cigarette smoking and risk of acute leukemia: associations with morphology and cytogenetic abnormalities in bone marrow. J Natl Cancer Inst 85: 1994–2003
Vickers M, Jackson G, Taylor P (2000) The incidence of acute promyelocytic leukemia appears constant over most of a human lifespan, implying only one rate limiting mutation. Leukemia 14: 722–726
Wheatley K, Burnett AK, Goldstone AH, Gray RG, Hann IM, Harrison CJ, Rees JKH, Stevens RF, Walker H (1999) A simple, robust, validated and highly predictive index for the determination of risk-directed therapy in acute myeloid leukaemia derived from the MRC AML 10 trial. Br J Haematol 107: 69–79
Acknowledgements
This work was supported by a research grant from the Leukaemia Research Fund. We thank the following for providing cytogenetic data: South West Regional Cytogenetics Centre, Bristol (Mrs C Kitchen); Cytogenetics Department, St James University Hospital, Leeds (Mrs H Dickinson); Oncology Cytogenetics Service, Christie Hospital, Manchester (Mr N Telford); Northern Genetics Service, Royal Victoria Infirmary, Newcastle-upon-Tyne (Mr N Bown); Wessex Regional Genetics Laboratory, Salisbury (Dr F Ross); Centre for Human Genetics, Sheffield (Ms A Watmore); Westlakes Research Institute, Cumbria (Mrs C Whitehouse) and the Medical Research Council Clinical Trials Service Unit, Oxford. We also thank all the consultants, hospital staff, general practitioners, interviewers and interviewees who participated in the case–control study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Moorman, A., Roman, E., Cartwright, R. et al. Age-specific incidence rates for cytogenetically-defined subtypes of acute myeloid leukaemia. Br J Cancer 86, 1061–1063 (2002). https://doi.org/10.1038/sj.bjc.6600195
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600195