Abstract
The endogenous viral superantigen 7 in DBA/2 mice serves as a target antigen on syngeneic ESb-MP lymphoma cells for allogeneic graft-vs-leukaemia reactive cells. Allogeneic viral superantigen 7 reactive Vβ6+ T cells are able to transfer graft-vs-leukaemia reactivity and to kill specifically viral superantigen 7+ ESb-MP tumour cells in vitro. Here we elucidate the mechanism of this superantigen specific cell lysis. Already 10 min after co-incubation with in vitro stimulated Vβ6+ T cells, viral superantigen 7+ ESb-MP tumour cells show an apoptotic phenotype (Annexin V-positivity, DNA-fragmentation). This extremely rapid type of cell death is not mediated by the death inducing ligands CD95L, TRAIL and TNF but by perforin and granzyme B. Surprisingly, neither mitochondria nor any of the known caspases appear to be involved in this type of tumour cell killing. In contrast, nitric oxide, released by activated macrophages and endothelial cells, induces in the same tumour cells another type of apoptosis which is much slower and involves mitochondria and caspase activation. A synergistic effect between the two different effector mechanisms of superantigen reactive donor cytotoxic T lymphocytes and nitric oxide releasing host macrophages and endothelial cells might explain the effective immune rejection of even advanced metastasised cancer in this graft-vs-leukaemia animal model.
Similar content being viewed by others
Main
In patients with chronic myeloid leukaemia, the adoptive transfer of allogeneic bone marrow and additionally the use of allogeneic donor lymphocytes have been shown to result in long-term survival of up to 80% of the patients (Slavin et al, 1998). This favourable graft-vs-leukaemia (GvL) effect is often associated with a risk for the development of graft-vs-host (GvH) disease with significant morbidity and mortality (Mackinnon et al, 1995; Slavin et al, 1998). We have established an animal model for the investigation of GvL and GvH reactivity of tumour-immune lymphocytes (Schirrmacher et al, 1995). In situ activated tumour-reactive lymphocytes from the tumour-resistant mouse strain B10.D2 are transferred into 5 Gy irradiated late-stage ESb-MP tumour-bearing DBA/2 mice. This leads to complete remission of the primary tumour and to the eradication of metastases. The two strains of mice are identical at the MHC but differ in minor histocompatibility and in Mls antigens (Schirrmacher et al, 1995, 1998). The latter represent endogenous viral superantigens (vSAGs) which are encoded by mouse mammary tumour virus proviruses (Mtvs) that are integrated in murine genomes (Beutner et al, 1992). In contrast to conventional antigens, SAGs are presented by MHC II molecules outside the binding groove and are recognised by certain Vβ-chains of the TCR (Choi et al, 1996). Since these endogenous SAGs behave like self-antigens, the reactive T cells are eliminated from the T cell repertoire by intra-thymic deletion (Speiser et al, 1989). One of the best studied vSAGs is vSAG7 which is encoded by Mtv7 and is expressed in DBA/2 mice and on syngeneic ESb-MP tumour cells but not in B10.D2 mice (Schirrmacher et al, 2000). vSAG7 is recognised by Vβ6+ T cells which are present in B10.D2 but deleted in DBA/2 mice.
We previously demonstrated that Vβ6+ T cells which are transferred with other splenic lymphocytes from the donor strain B10.D2 into tumour-bearing DBA/2 mice are able to break the anti-tumour tolerance (Schirrmacher et al, 2000) and to infiltrate the metastasised organs (Schirrmacher et al, 1995). In the liver, these Vβ6+ T cells form close contacts with vSAG7 expressing metastasised tumour cells (vSAG7+ ESb-MP) and with host macrophages in the vicinity of metastases (Müerköster et al, 1998). Moreover, treatment of tumour-bearing DBA/2 mice with freshly isolated Vβ6+ T cells led to retarded tumour outgrowth and to prolonged survival in comparison to untreated animals. In addition, Vβ6+ cells killed specifically tumour cells expressing the endogenous vSAG7 in vitro (Schirrmacher et al, 2000).
Cytotoxic T lymphocytes (CTL) kill their target cells via apoptosis by different mechanisms, for instance, via CD95-CD95L interaction (Henkart, 1994; Kägi et al, 1994) or via the release of cytolytic granules containing perforin and granzymes upon contact with the target cell (Kägi et al, 1994; Pinkoski et al, 2000). Other molecules which can induce apoptosis especially in tumour cells are TNF-α and TNF-related apoptosis inducing ligand (TRAIL) (Wiley et al, 1995). After triggering the respective death receptor a cascade of caspases is activated, which finally leads to DNA-fragmentation and cell death (Krammer, 1998; Pinkoski et al, 2000). The apoptotic process can also implicate changes in the mitochondria that leads to the loss of the mitochondrial transmembrane potential (Δψm) (Ushmorov et al, 1999; Kroemer and Reed, 2000). Granzymes (Ebnet et al, 1991) which belong to the family of serine proteases are also found to induce DNA-fragmentation, for instance by activating caspase-3 (Pinkoski et al, 2000). Yet, several recent reports indicate that induction of apoptosis and the subsequent DNA-fragmentation do not necessarily involve the activation of caspases (Thomas et al, 2000).
SAGs are a collection of bacterial and viral proteins with potent immunostimulatory properties. The targeting of them to tumour cells has become an interesting new concept to augment endogenous anti-tumour reactivity but little is known so far about the mechanisms involved (Choi et al, 1996). This study aimed to investigate how vSAG7 activated T lymphocytes kill SAG expressing tumour cells and to obtain more insights into the mechanism of SAG specific tumour cell lysis and GvL activity.
Materials and methods
Animals and cell lines
B10.D2 mice (Olac, Bicester, UK) were kept under specific pathogen free conditions and were used at the age of 6–8 weeks. All animal experiments were performed according to the standards required by the UKCCCR Guidelines. Eb is a chemically induced T cell lymphoma (L5178Y/E) of DBA/2 mice. ESb-MP is a spontaneous high metastatic adhesion variant of Eb and arose most likely after fusion of Eb cells with a host macrophage (Larizza et al, 1984). Jurkat is a human leukaemia T cell line, BL60 is a human leukaemia B cell line and U937 is a human promonocytic cell line. Cell lines were maintained in 5% CO2 at 37°C in RPMI-1640 containing 10% FCS (both Life Technologies, Eggenstein, Germany). In some experiments, Vβ6+ T cells were primed by injecting 5 × 104 ESb-MP tumour cells in PBS into the ear pinna of B10.D2 mice. Animals were sacrificed 9 days after injection.
Abs and other reagents
The rat-anti-mouse Vβ6 mAb was used as culture supernatant (clone 44-22-1) (Payne et al, 1988). The anti-APO-1 antibody (Trauth et al, 1989) is directed against human (hu) CD95. Hu TRAIL-R2-Fc, hu TNF-R2-Fc and hu CD95-Fc were used in the blocking experiments (Walczak et al, 1997, 1999). Leucine Zipper (LZ)-TRAIL, TNF-α and LZ-CD95L were used for induction of apoptosis (Walczak et al, 1999). All human reagents are also reactive to murine cells (Walczak et al, 1999). Human IgG was purchased from Sigma (Deisenhofen, Germany). Recombinant (rec.) human IFN-γ was obtained from Biomol (Hamburg, Germany). Annexin V-FITC was obtained from R&D systems (Wiesbaden, Germany). The following caspase inhibitors were purchased from Bachem (Heidelberg, Germany): ZVAD-fmk (Z-Val-Ala-DL-Asp-fluoromethylketone) and IETD-CHO (Ac-Ile-Glu-Thr-Asp-aldehyde (pseudo acid). JC1 (5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethyl-benzimidazol-carbocyanine iodide) was from Molecular Probes (Eugene, OR, USA). Concanamycin A and granzyme B inhibitor (Z-AAD-CMK) were obtained from Calbiochem (Bad Soden, Germany). To evaluate apoptotic effects of nitric oxide (NO), glycerol trinitrate (GTN; Merck; Darmstadt, Germany) was used.
Isolation of Vβ6+ T cells via magnetic beads
Vβ6+ T cells were isolated as previously described (Müerköster et al, 1998). Spleen cells from B10.D2 mice were incubated with rat-anti-Vβ6 mAbs and with magnetic beads-conjugated anti-rat IgG isotype Abs (Dynal, Hamburg, Germany). Cells were separated via a Dynal-magnet. The purity of the positively selected Vβ6+ T cells was >88%. In some experiments, CD4+ or CD8+ T cells were isolated by depletion of CD8+ or CD4+ T cells by Dynabeads-conjugated anti-mouse CD8 or Dynabeads-conjugated anti-mouse CD4 (both Dynal) respectively. Then CD4+Vβ6+ and CD8+Vβ6+ T cells were isolated as previously described (Müerköster et al, 1998). After isolation, CD8+Vβ6+ T cell population contained 0.4% CD4+ cells and the population of CD4+Vβ6+ T cells 0.3% CD8+ cells.
Mixed lymphocyte tumour cell culture for induction of cytotoxic actitivity
Isolated Vβ6+ T cells from normal or immunised B10.D2 mice were incubated with 100 Gy γ-irradiated (Gammacell 1000, Ottawa, Canada) Vβ6 negative spleen cells (used as APC) and ESb-MP or Eb tumour cells for 4 days. Cytotoxic acticity of in vitro stimulated Vβ6+ T cells were tested either by a 51Cr-release-assay or by FACS analysis.
51Cr-release-assay
ESb-MP and Eb target cells were labelled with 0.2 μCi 51Cr sodium chromate (Amersham, Braunschweig, Germany) in RPMI-1640 medium with 30% FCS for 90 min at 37°C. Vβ6+ effector T cells were incubated with target cells (effector : target ratio 10 : 1) in 96-well round bottom plates (Renner, Dannstadt, Germany) for 4 h at 37°C. Radioactivity released in supernatants was measured by a γ-counter (LKB-Wallac, Freiburg, Germany) as described (Schirrmacher et al, 2000). In all experiments, an effector : target ratio of 10 : 1 was used. This ratio has been previously shown to be an optimal (Schirrmacher et al, 2000).
Determination of cytotoxicity via flow cytometry
Effector cells (Vβ6+ T cells) were incubated with target ESb-MP cells (10 : 1 ratio) in 6-well plates for different periods of time (10–240 min). To determine which death receptors could be involved in the induction of apoptosis, ESb-MP cells were treated with 1 or 10 μg ml−1 LZ-TRAIL, 1 μg ml−1 LZ-CD95L, TNF-α or 10 μg ml−1 control IgG for 4 h without or with 24 h pre-incubation with IFN-γ. As a control for induction of apoptosis, either ESb-MP cells were incubated with 0.5 mM GTN for 24 h or Jurkat cells were treated with 1 μg ml−1 anti-APO-1/Protein A (10 ng ml−1, Sigma) or 1 μg ml−1 LZ-CD95L, BL60 cells were treated with 1 μg ml−1 LZ-TRAIL and U937 cells were treated with TNF-α overnight to induce apoptosis. To block apoptosis in ESb-MP cells, the following reagents were used: hu TRAIL-R2-Fc (10 μg ml−1), hu CD95-Fc (10 μg ml−1), hu TNF-R2-Fc (10 μg ml−1), hu IgG1 as isotype control (10 μg ml−1), Concanamycin A (10 nM), granzyme B inhibitor (20 μM), ZVAD-fmk (25 μM) and IETD-CHO (25 μM). Treatment of effector and target cells with the respective reagent started 15–60 min before the co-incubation. As a positive control, 1–30 μg ml−1 CD95-Fc, TNF-R2-Fc and TRAIL-R2-Fc were used to block apoptosis in Jurkat, BL60 and U937 cells. After removal of effector cells, ESb-MP cells were washed, detached from the plates, and cytotoxicity was determined by staining with 1 μg ml−1 propidium iodide (PI) which was added to the cells 5 min before measurement.
Target cell apoptosis
Apoptosis was assessed either by Annexin V/PI staining (Koopman et al, 1994) or by determining DNA-fragmentation (Nicoletti et al, 1991). After co-incubation with effector cells, 5 × 105 ESb-MP target cells were either resuspended in binding buffer (R&D systems), 50 ng ml−1 Annexin V and 1 μg ml−1 PI or treated with a hypotonic solution (0.1% sodium citrate, 0.1% Triton X-100) containing 50 μg ml−1 PI overnight. Jurkat cells were incubated in the hypotonic solution containing PI and DNA-fragmentation was measured as described above. Target cell death and apoptosis were analyzed by flow cytometry using a FACScan analyzer with CellQuest software (BD Bioscience, Heidelberg, Germany).
Cytofluorometric analysis of mitochondrial transmembrane potential (Δψm)
Δψm was measured with JC1 as described (Salvioli et al, 1997). JC1 is a cyanine dye which accumulates in the mitochondrial matrix under the influence of the Δψm. In the presence of a high Δψm, JC1 forms aggregates which have characteristic absorption and emission spectra so that cells are detectable as FL1− and FL2+. 5 × 105 ESb-MP tumour cells were treated with 5 μg ml−1 JC1 for 20 min at 4°C followed by FACScan analysis. As a control, Jurkat cells were treated with 1 μg ml−1 anti-APO-1 mAb crosslinked by 10 ng ml−1 Protein A for 12 h followed by incubation with JC1 as described above.
Detection of perforin in Vβ6+ T cells
Isolated Vβ6+ T cells were stimulated either with ESb-MP or with Eb cells and APCs or were left without any stimulation. After 4 days supernatants were taken and centrifuged by 500 r.p.m. for 5 min. The pellet containing Vβ6+ T cells were washed with PBS and centrifuged on siliconised glass slides (Sigma). After drying, slides were fixed in acetone for 10 min at room temperature followed by washing in PBS. To avoid nonspecific binding, slides were treated with 1% normal goat serum for 15 min followed by incubation with the rat-anti-mouse perforin mAb (Alexis, Grünberg, Germany) for 45 min. After washing, slides were treated with a goat-anti-rat antibody conjugated with alkaline phosphatase (AP). Then slides were washed with water, counterstained with hemalaun (Sigma) and mounted with glycerol-gelatin (Merck). The substrate for the development of AP consisted of 6.3 μl 5% Neufuchsin (Sigma) or 2 mg Fast Blue (Sigma) in 16 μl 4% sodium nitrite (Fluka, Buchs, Switzerland), 2 mg naphthol-As-Bi-phosphate (Sigma) in 20 μl N,N-dimethylformamide (Merck) and 3 ml of 0.05 M l−1 Tris-HCl-buffer, pH 8.7 containing 1 mM levamisole (Sigma). As negative control either the first antibody was omitted or an isotype matched control antibody was used. Both stainings revealed no staining.
Results
Activated Vβ6+ T cells kill vSAG7+ ESb-MP tumour cells by induction of apoptosis
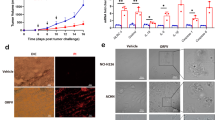
Vβ6+ T cells, stimulated for 4 days with tumour cells and spleen cells as APC were able to kill vSAG7+ ESb-MP tumour cells while vSAG7− Eb tumour cells were hardly lysed (Figure 1A). Experiments with the separation of Vβ6+ T cells into CD4+ and CD8+ T cells revealed that both T cell subpopulations induced cell death in ESb-MP target cells (Figure 1B).
Cytotoxicity towards vSAG7+ tumour cells generated by stimulated Vβ6+ T cells in vitro. (A) Vβ6+ T cells were isolated from B10.D2 mice which were either immunised with ESb-MP cells or remained untreated (1° in vivo). Then, Vβ6+ T cells were stimulated for 4 days either with irradiated vSAG7− Eb or with vSAG7+ ESb-MP cells and APC (2° in vitro) and tested for cytotoxicity towards Eb or ESb-MP target cells (effector : target ratio 10 : 1) in a 4 h 51Cr-release assay. The mean±standard deviation of triplicates of two independent experiments are shown. (B) CD4+Vβ6+, CD8+Vβ6+ and total Vβ6+ T cells were isolated from non-immunised B10.D2 mice, purified and stimulated with irradiated ESb-MP and APCs for 4 days. Then effector cells were co-cultured with target ESb-MP cells for 2 h, and tumour cell lysis was determined by PI staining and FACScan analysis. The mean±standard deviation from 2–4 independent experiments are shown.
CTLs directed to conventional antigens consisting of peptide/MHC complexes kill their target cells via apoptosis (Henkart, 1994; Kägi et al, 1994). To determine whether vSAG7 reactive Vβ6+ T cells are able to induce apoptosis, we assessed the death of vSAG7+ ESb-MP cells after co-incubation with stimulated Vβ6+ T cells by two different methods. Figure 2A shows the kinetics of apoptosis measured by Annexin V staining/PI staining. After 10 min, 21% of the ESb-MP cells were Annexin V+ indicating that they were in the early phase of apoptosis. Additionally, at this time point, 26% were Annexin V+/PI+, a phenotype specific for the late stage of apoptosis. The maximal amount of apoptotic cells (63%) was detected after 20 min and remained at this level until 240 min of coincubation. Changes in the forward/side scatter which are also typical for apoptosis started as well after 10 min of coincubation of effector and target cells (data not shown). When measuring oligonucleosomal DNA-fragmentation, 45% of apoptotic ESb-MP cells were observed after 10 min of coculture (Figure 2B). The maximal level of apoptotic cells was reached after 30 min. Taken together, these observations reveal that Vβ6+ T cells are able to rapidly induce apoptosis in vSAG7+ ESb-MP tumour cells.
Stimulated Vβ6+ T cells induce apoptosis in vSAG7+ ESb-MP tumour cells. In vitro stimulated Vβ6+ T cells were co-incubated with ESb-MP cells in a ratio of 10 : 1 for different periods of time and stained either with Annexin V-FITC and 1 μg ml−1 PI (A) or were treated with a hypotonic solution containing 50 μg ml−1 PI overnight to determine DNA-fragmentation (B). Untreated cells showed no changes in the amount of apoptotic cells during coincubation. Apoptosis was determined by FACScan analysis. One representative experiment out of four (A) or three (B) independent experiments is shown.
Induction of apoptosis in ESb-MP cells is caspase-independent and does not involve mitochondrial damage
Caspases are known as main effector enzymes responsible for the initiation of DNA-fragmentation and the typical morphological changes in apoptosis (Henkart, 1994; Krammer, 1998). To analyse the involvement of caspases in this rapid vSAG7-mediated tumour cell lysis, we added either ZVAD-fmk (a broad spectrum caspase inhibitor) or IETD-CHO (a specific inhibitor of caspase 8) to the coculture of Vβ6+ T cells and ESb-MP tumour cells. As shown in Figure 3, ZVAD-fmk and IETD-CHO blocked almost completely the death of Jurkat cells which were treated with anti-CD95 mAbs. In addition, ZVAD-fmk also inhibited NO-mediated apoptosis in ESb-MP cells. In contrast, ZVAD-fmk and IETD-CHO did not influence significantly the Vβ6+ T cell mediated apoptosis in ESb-MP cells. Thus Vβ6+ T cells were able to induce apoptosis in vSAG7+ ESb-MP tumour cells in a caspase-independent manner.
Vβ6+ T cell induced apoptosis in ESb-MP cells is caspase-independent. Stimulated Vβ6+ T cells were coincubated with ESb-MP tumour cells (effector : target ratio 10 : 1) for 4 h or treated with 0.5 mM GTN (NO). Jurkat cells were stimulated with an anti-APO-1 (CD95) mAb/Protein A for 12 h. In some cultures, 25 μM ZVAD-fmk or 25 μM IETD-CHO were added. As a control, ESb-MP cells and Jurkat cells were cultured without Vβ6+ T cells and reagents. Cell death was determined by PI staining and FACScan analysis. The mean±standard deviation from three independent experiments are shown.
The dye JC1 is known as a marker for changes in the Δψm which can be associated with apoptosis (Salvioli et al, 1997). To evaluate whether mitochondria are involved in the induction of vSAG7 mediated apoptosis in ESb-MP cells, we performed JC1 staining of ESb-MP cells after co-incubation with Vβ6+ T cells for different periods of time. In cells with intact mitochondria and high Δψm, JC1 forms so called J-aggregates that are associated with a large shift in emission (590 nm=Fl 1). In Jurkat cells which were treated with anti-CD95 mAbs for 12 h the involvement of mitochondria could be clearly detected (Figure 4). In contrast no changes in Δψm were observed during 4 h co-culture of Vβ6+ T cells with ESb-MP tumour cells (Figure 4). Staining with 3,3′-dihexyloxacarbocyanine iodide (DiOC6) and dihydroethidine (HE), which are used to determine changes in Δψm and the production of reactive oxygen species (ROS), respectively (Ushmorov et al, 1999) also showed no mitochondrial alterations during Vβ6+ T cell-mediated apoptosis in ESb-MP tumour cells (data not shown). In contrast, NO, another inducer of apoptosis in these cells, stimulated mitochondrial changes (data not shown).
Vβ6+ T cell-induced apoptosis in ESb-MP cells does not involve changes in Δψm. ESb-MP cells remained untreated (light line) or were cocultured with stimulated Vβ6+ T cells in a effector : target ratio of 10 : 1 for 4 h (dark line). As a control, Jurkat cells were left untreated (light line) or treated with anti-APO-1 mAb/Protein A for 12 h (dark line). Afterwards, ESb-MP cells and Jurkat cells were either analysed for DNA-fragmentation (FL3) or for changes in Δψm by JC1 staining (FL1). Upon incubation of Jurkat cells with anti-APO-1 mAb, FL2 did not significantly change, whereas FL1, which indicates the formation of dye monomer, increased due to the reduction of Δψm. This increase is taken as a measure for the loss of Δψm. One representative experiment out of three is shown.
TRAIL, CD95L and TNF-α are not involved in the induction of apoptosis in ESb-MP cells
Several death receptors and their respective ligands have been shown to be involved in the induction of apoptosis (Kägi et al, 1994; Wiley et al, 1995). The most common are TRAIL-R1+2/TRAIL, CD95/CD95L and TNF-R1+2/TNF. We tested whether ESb-MP cells were sensitive towards the apoptosis-inducing potential of CD95L, TRAIL and TNF-α. Figure 5A shows the positive controls: CD95L was able to induce apoptosis in Jurkat cells, TRAIL induced apoptosis in BL60 and TNF-α induced apoptosis in U937 cells. In each cell line, apoptosis could be blocked using soluble Fc-fusion proteins against the respective ligands. In contrast, ESb-MP tumour cells were not sensitive towards any of these ligands, even after IFN-γ stimulation for 24 h since cytotoxicity was not increased in comparison to untreated ESb-MP cells (Figure 5B). Furthermore, blocking with TRAIL-R2-Fc, CD95-Fc and TNF-R2-Fc did not significantly affect cell lysis of ESb-MP target cells by stimulated Vβ6+ T cells (Figure 5C). Treatment with the isotype matched Ig control increased slightly but not significantly the number of apoptotic ESb-MP cells. We conclude that Vβ6+ T cells induce apoptosis in ESb-MP tumour cells independently of CD95L, TRAIL and TNF-α.
ESb-MP cells are resistent towards TRAIL-, CD95L- or TNF-α induced apoptosis. (A) Jurkat cells were treated with 1 μg ml−1 CD95L, BL60 cells were cultured with 1 μg ml−1 TRAIL and U937 cells were incubated with 1 μg ml−1 TNF-α for 12 h. Apoptosis was blocked by 1–30 μg ml−1 CD95-Fc, TRAIL-R2-Fc or TNF-R2-Fc. One representative experiment out of three is shown. (B) ESb-MP cells were incubated with 10 nM recombinant IFN-γ for 24 h in RPMI medium supplemented with 10% FCS followed by treatment with 1 or 10 μg ml−1 TRAIL, 1 μg ml−1 CD95L, 1 or 10 μg ml−1 TNF-α. As a control, ESb-MP cells remained untreated (ESb-MP). (C) ESb-MP cells were cultured for 4 h alone, with Vβ6+ T cells (Vβ6), Vβ6+ T cells and IgG (10 μg ml−1), with Vβ6+ T cells and TRAIL-R2-Fc (10 μg ml−1), Vβ6+ T cells and CD95-Fc (10 μg ml−1) or with Vβ6+ T cells and TNF-R2-Fc (10 μg ml−1). In (B) and (C) the effector : target cell ratio was 10 : 1. The death of ESb-MP and Jurkat cells was assessed by PI staining and FACScan analysis. The mean±standard deviation from three independent experiments are shown.
Vβ6+ T cells induce cytotoxicity in ESb-MP cells through perforin/granzyme B
Perforin/granzymes are able to induce apoptosis in a death receptor-independent manner (Kägi et al, 1994; Trapani et al, 1998; Pinkoski et al, 2000). Figure 6A shows that Vβ6+ T cells stimulated with vSAG7+ ESb-MP cells for 4 days expressed perforin while no expression of perforin was found in Vβ6+ T cells from control cultures without stimulation or stimulated with vSAG7− Eb cells. Figure 6B shows the effects of treatment of Vβ6+ T effector cells and ESb-MP target cells with Concanamycin A, an inhibitor of perforin or of treatment with an inhibitor of granzyme B or a combination of both. Concanamycin A alone did not inhibit target cell lysis while treatment with the granzyme B inhibitor led to a significant reduction of apoptosis. Treatment with both inhibitors almost completely prevented the lysis of ESb-MP cells (from 35 to 5% apoptosis, Figure 6B). Together, these data indicate that vSAG7 stimulated expression of perforin in Vβ6+ T cells. These activated cells induced apoptosis in ESb-MP tumour cells via released perforin and granzyme B.
Apoptosis of ESb-MP cells is mediated by perforin and granzyme B. (A) Shows perforin expression in Vβ6+ T cells. Vβ6+ T cells were stimulated with vSAG7− Eb or vSAG7+ ESb-MP cells and APCs for 4 days. Then unstimulated (control) or stimulated Vβ6+ T cells were stained with an anti perforin mAb. Cells were counterstained with hemalaun. Membrane staining indicates positively labelled cells. Black dots are magnetic beads which were used for the purification and could not be removed after 4 days of stimulation. Magnification × 400. (B) ESb-MP cells were cultured either alone (ESb-MP) or with stimulated Vβ6+ T cells at an effector : target ratio of 10 : 1. Separate groups of effector cells were treated either with 10 nM Concanamycin A (Concan.A), 20 μM granzyme B inhibitor (Z-AAD-CMK) or with a combination of both inhibitors (Vβ6+Concan.A+GranzB.Inh.) for 15 min before coincubation with target cells for 4 h. Incubation of ESb-MP cells alone with Concanamycin A and granzyme B inhibitor revealed no significant difference in comparison to the ESb-MP control. Apoptosis was determined by PI incorporation and FACScan analysis. The mean±standard deviation from three independent experiments are shown.
Discussion
We have recently identified a tumour associated endogenous vSAG7 as a new target antigen for allogeneic GvL reactivity in a murine tumour model (Schirrmacher et al, 2000). In DBA/2 mice, vSAG7 behaves as a strong tolerogen leading to central deletion of SAG-reactive Vβ6+ T cells during thymic maturation. While the DBA/2 derived Eb T lymphoma cells did not express this SAG, the spontaneous metastatic variant ESb and its adhesion variant ESb-MP expressed endogenous mouse mammary tumour provirus (Mtv)- typical intracisternal A-particles (IAP), Mtv7 orf/SAG message and vSAG7 protein at the cell surface (Schirrmacher et al, 2000). MMTV and IAPs have been suggested to be associated with tumorigenicity and progression towards increased malignancy (Schirrmacher et al, 1998). We previously reported that the allogeneic MHC identical mouse strain B10.D2 in contrast to DBA/2 was able to strongly reject ESb and ESb-MP tumours and that vSAG7 reactive Vβ6+ T cells were involved in this GvL reactivity (Schirrmacher et al, 2000).
In this study, we investigated the mechanism of tumour cell destruction in vitro by vSAG7 reactive Vβ6+ T cells. We show here that Vβ6+ T cells kill vSAG7+ tumour cells via release of perforin and granzyme B. Interestingly, this form of cell death is independent of the known caspases and occurs without the involvement of mitochondria. It has been previously reported that vSAG7 can induce IFN-γ production by specifically primed CD8+ T cells but fails to trigger cytotoxicity (Herrmann et al, 1992). However, in contrast to Herrmann et al (1992), we find that vSAG7 stimulates Vβ6+ T cells to express perforin and to kill vSAG7+ target cells. This kill is SAG-specific and occurs in several tumour cells that express this endogenous viral superantigen (Schirrmacher et al, 2000). Interestingly, this SAG specific CTL activity is mediated via both CD8+Vβ6+ and CD4+Vβ6+ T cells.
Bacterial SAG have been shown to trigger CD8+ T cell clones that are specific for other antigens (e.g. influenza virus peptides), but in these systems the exerted cytotoxicity was mediated via the CD95/CD95L system (Fuller and Braciale, 1998). Sundstedt et al (1998) showed that injection of staphylococcal enterotoxin A into perforin-deficient mice led to less depletion of B-cells than in control mice. This depletion was due to the release of perforin by CD8+ T cells. In GvL and GvH reactivity, a role for both systems (granule exocytosis as well as CD95/CD95L) was reported (Miwa et al, 1999; Yasukawa et al, 2000). It was thus of interest to elucidate the mechanism by which allogeneic Vβ6+ T cells kill vSAG7+ tumour cells.
TNF-α and CD95L play a crucial role in the activation induced cell death (AICD) of mature T cells (Dhein et al, 1995; Zheng et al, 1995) whereas TRAIL has been shown to induce apoptosis mainly in tumour cells (Wiley et al, 1995; Walczak et al, 1999) but also in normal human hepatocytes, astrocytes and keratinocytes (Jo et al, 2000). ESb-MP tumour cells were not sensitive towards any of these death ligands and blocking of these pathways during coincubation of effector and tumour cells did not influence the cytotoxic reactivity of Vβ6+ T cells.
The perforin/granzyme system is involved in the cytotoxic reactivity of CD8+ T cells (Kägi et al, 1994; Pinkoski et al, 2000). Recently, perforin has been shown to play a role in AICD of T cells in an allogeneic transplantation model (Spaner et al, 1999). In our model, Vβ6+ T cells showed a high perforin expression after 4 days of in vitro stimulation. The lysis of ESb-MP tumour cells was almost completely inhibited by the perforin (concanamycin A) and granzyme B inhibitors. Interestingly, treatment with granzyme B inhibitor but not with concanamycin A alone inhibited target cell lysis. This might be due to the fact that membrane damage induced by perforin does not directly cause target cell death, but facilitates the entry of granzymes into the cell (Shresta et al, 1999; Trapani et al, 1998). Granzyme B, however, can also enter the cell via the cation-independent mannose 6-phosphate/insulin-like growth factor receptor (Motyka et al, 2000), which might explain our observations.
The vSAG7 mediated tumour cell lysis was very fast. This is in accordance with other observations demonstrating that granzyme B, in contrast to granzyme A, is responsible for a rapid cytotoxic effect (Drénou et al, 1999). We cannot exclude that granzyme A might also be active in ESb-MP cells, since application of the granzyme B inhibitor alone did not completely block apoptosis. However, there is evidence that granzyme A and B do not synergize but act independently of each other (Shresta et al, 1999).
The requirement of caspases as the main effector enzymes in the initiation of the apoptotic cascade is still a matter of debate (Krammer, 1998; Pinkoski et al, 2000). Several recent reports indicate that induction of apoptosis and subsequent DNA-fragmentation do not neccessarily involve the activation of caspases (Beresford et al, 1999; Drénou et al, 1999). vSAG7 specific Vβ6+ T cells could kill ESb-MP tumour cells independently of caspases since blocking with ZVAD-fmk and IETD-CHO did not lead to an inhibition of apoptosis in ESb-MP cells. In contrast, NO-induced apoptosis in these tumour cells required caspase activity. Beresford et al (1999) showed that cytolysis mediated by granzyme B was caspase independent whereas DNA-fragmentation was caspase-dependent. In contrast, in our model blocking with caspase inhibitors influenced neither cytolysis nor DNA-fragmentation (data not shown).
The question arises how granzyme B may lead to DNA cleavage without activation of caspases. It was reported that granzyme B directly cleaves caspase substrates such as poly (ADP-ribose) polymerase, the catalytic subunit of DNA-dependent protein kinases and NuMA to bring about apoptotic changes in cells (Froelich et al, 1996; Andrade et al, 1998). Moreover, granzyme B induced the processing of DFF45/ICAD in a caspase-independent fashion resulting in DNase activation and DNA fragmentation (Thomas et al, 2000). In addition, granule-mediated cell death can proceed independently of caspases through a non-nuclear pathway (Sarin et al, 1997). These pathways seemed to be important for cells that are infected by viruses which are able to postpone cell death by caspase inhibitors like crmA (Zhou et al, 1997). This might explain why we find this kind of cell death in ESb-MP tumour cells in which virus-like particles and proviral genes are expressed (Müerköster et al, 1998).
The involvement of mitochondria in apoptosis was described for different apoptotic agents (Kroemer and Reed, 2000). We reported previously that NO-mediated apoptosis in human leukaemia cells is associated with mitochondrial damage (i.e., a degradation of major mitochondrial lipid cardiolipin and cytochrome c release into the cytosol) followed by an activation of caspase-9 and caspase-3 (Ushmorov et al, 1999). Furthermore, we found that NO produced by activated Kupffer cells during adoptive immunotherapy with GvL-reactive T cells contributed to apoptosis in metastatic ESb-MP tumour cells in the liver (Müerköster et al, 2000). We showed also that this cell death can be induced by a mitochondria-dependent mechanism driven by CD40-CD40L interactions (Müerköster et al, 2000). In contrast, vSAG7 mediated apoptosis in ESb-MP cells occurred independently of mitochondria since staining with JC1, DiOC6 and HE revealed no mitochondrial damage.
In conclusion, we show that vSAG7 specific T cells rapidly induce apoptosis in vSAG7+ tumour cells via perforin and granzyme B which occurs without involvement of mitochondria and independently of caspases. This CTL activation leads to increased tumour resistance and can be used for cellular therapy and to break immunological tumour tolerance (Schirrmacher et al, 2000). These results support the importance of granule-mediated CTL lysis of tumour cells together with apoptosis induced by NO releasing host macrophages and endothelial cells for an effective antitumour response in vivo during adoptive immunotherapy.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Andrade F, Roy S, Nicholson D, Thornberry N, Rosen A, Casciola-Rosen L (1998) Granzyme B directly and efficiently cleaves several downstream caspase substrates: implications for CTL-induced apoptosis. Immunity 8: 451–460
Beresford PJ, Xia Z, Greenberg AH, Liebermann J (1999) Granzyme A loading induces rapid cytolysis and a novel form of DNA damage independently of caspase activation. Immunity 10: 585–594
Beutner U, Frankel WN, Cote MS, Coffin JM, Huber BT (1992) Mls-1 is encoded by the long terminal repeat open reading frame of the mouse mammary tumor provirus Mtv-7. Proc Natl Acad Sci USA 89: 5432–5436
Choi Y, Marrack P, Kappler JW (1996) Structural analysis of a mouse mammary tumor virus superantigen. J Exp Med 175: 847–852
Dhein J, Walczak H, Bäumler C, Debatin KM, Krammer PH (1995) Autocrine T-cell suicide mediated by APO-1 (Fas/CD95). Nature (Lond.) 373: 438–441
Drénou B, Blanchereau V, Burgess DH, Fauchet R, Charron DJ, Mooney NA (1999) A caspase-independent pathway of MHC Class II antigen-mediated apoptosis of human B lymphocytes. J Immunol 163: 4115–4124
Ebnet K, Chluba-de Tapia J, Hurtenbach U, Kramer MD, Simon MM (1991) In vivo-primed mouse T cells selectively express T cell-specific serine proteinase-1 and proteinase-like molecules granzyme B and C. Int Immunol 3: 9–19
Froelich CJ, Hanna WL, Poirier GG, Duriez PJ, D'Amours D, Salvesen GS, Alnemri ES, Earnshaw WC, Shah GM (1996) Granzyme B/perforin-mediated apoptosis of Jurkat cells results in cleavage of poly(ADP-ribose) polymerase to the 89-kDa apoptotic fragment and less abundant 64-kDa fragment. Biochem Biophys Res Commun 227: 658–665
Fuller CL, Braciale VL (1998) Selective induction of CD8+ cytotoxic T lymphocytes effector function by Staphylococcus Enterotoxin B. J Immunol 161: 5179–5186
Henkart PA (1994) Lymphocyte-mediated cytotoxicity: two pathways and multiple effector molecules. Immunity 1: 343–346
Herrmann T, Waander GA, Chvatchko Y, MacDonald HR (1992) The viral superantigen Mls-1a induces interferon-γ secretion by specifically primed CD8+ cells but fails to trigger cytotoxicity. Eur J Immunol 22: 2789–2793
Jo M, Kim TH, Seol DW, Esplen JE, Dorko K, Billiar TR, Strom SC (2000) Apoptosis induced in normal human hepatocytes by tumor necrosis factor-related apoptosis-inducing ligand. Nature Med 6: 564–567
Kägi D, Vignaux F, Ledermann B, Bürki K, Depraetere V, Nagata S, Hengartner H, Golstein P (1994) Fas and perforin pathways as major mechanisms of T-cell mediated cytotoxicity. Science 265: 528–530
Koopman G, Reutelingsperger CP, Kuijten GA, Keehnen RM, Pals ST, van Oers MH (1994) Annexin V for flow cytometric detection of phosphatidylserine expression on B cells undergoing apoptosis. Blood 84: 1415–1420
Krammer PH (1998) CD95 (Apo-1/Fas)-mediated apoptosis: Live and let die. Adv Immunol 71: 163–207
Kroemer G, Reed JC (2000) Mitchondrial control of cell death. Nature Med 6: 513–519
Larizza L, Schirrmacher V, Pflüger E (1984) Acquisition of high metastatic capacity after in vitro fusion of a non-metastatic tumor line with a bone-marrow derived macrophage. J Exp Med 160: 1579–1584
Mackinnon S, Papadopoulos EB, Carabasi MH, Reich L, Collins NH, Boulad F, Castro-Malaspina H, Childs BH, Gillio AP, Kernan NA (1995) Adoptive immunotherapy evaluating escalating doses of donor leukocytes for relapse of chronic myeloid leukemia after bone marrow transplantation: separation of graft-versus-leukemia responses from graft-versus-host disease. Blood 86: 1261–1268
Miwa K, Hashimoto H, Yatomi T, Nakamura N, Nagata S, Suda T (1999) Therapeutic effect of an anti-Fas ligand mAb on lethal graft-versus-host disease. Int Immunol 11: 925–931
Motyka B, Korbutt G, Pinkowski MJ, Heilbein JA, Caputo A, Hobman M, Barry M, Shostak I, Sawchuk T, Holmes CFB, Gauldie J, Bleackley RC (2000) Mannose 6-Phosphate/Insulin-like Growth factor II receptor is a death receptor for granzyme B during cytotoxic T cell-induced apoptosis. Cell 103: 491–500
Müerköster S, Wachowski O, Zerban H, Schirrmacher V, Umansky V, Rocha M (1998) Graft-versus-leukemia reactivity involves cluster formation between superantigen-reactive donor T lymphocytes and host macrophages. Clin Cancer Res 4: 3095–3106
Müerköster S, Laman JD, Rocha M, Umansky V, Schirrmacher V (2000) Functional and in situ evidence for nitric oxide production driven by CD40-CD40L interactions in graft-versus-leukemia reactivity. Clin Cancer Res 6: 1988–1996
Nicoletti I, Migliorati G, Pagliacci MC, Grignani F, Riccardi C (1991) A rapid and simple method for measuring thymocyte apoptosis by propidium iodide staining and flow cytometry. J Immunol Method 139: 271–279
Payne J, Huber BT, Cannon NA, Schneider R, Schilham MW, Acha-Orbea H, Mac-Donald HR, Hengartner H (1988) Two monoclonal rat antibodies with specificity for the β-chain variable region Vβ6 of the murine T-cell receptor. Proc Natl Acad Sci USA 855: 7695–7698
Pinkoski MJ, Heilbein JA, Barry M, Bleackley RC (2000) Nuclear translocation of granzyme B in target cell apoptosis. Cell Death Diff 7: 17–24
Salvioli S, Ardizzoni A, Franceschi C, Cossarizza A (1997) JC-1, but not DiOC6(3) or rhodamine 123, is a reliable fluorescent probe to assess Δψ changes in intact cells: implications for studies on mitochondrial functionality during apoptosis. FEBS Lett 411: 77–82
Sarin A, Williams MS, Alexander-Miller MA, Berzofsky JA, Zacharchuk CM, Henkart PA (1997) Target cell lysis by CTL granule exocytosis is independent of ICE/Ced-3 family proteases. Immunity 6: 209–215
Schirrmacher V, Beckhove P, Krüger A, Rocha M, Umansky V, Fichtner KP, Hull WE, Zangemeister-Wittke U, Griesbach A, Jurianz K, von Hoegen P (1995) Effective immune rejection of advanced metastasized cancer. Int J Oncol 6: 505–521
Schirrmacher V, Beutner U, Bucur M, Umansky V, Rocha M, von Hoegen P (1998) Loss of endogenous mouse mammary tumor virus superantigen increases tumor resistance. J Immunol 161: 563–570
Schirrmacher V, Müerköster S, Bucur M, Umansky V, Rocha M (2000) Breaking tolerance to a tumor-associated viral superantigen as a basis for graft versus leukemia (GvL) reactivity. Int J Cancer 87: 695–706
Shresta S, Graubert TA, Thomas DA, Raptis SZ, Ley TJ (1999) Granzyme A initiates an alternative pathway for granule-mediated apoptosis. Immunity 10: 595–605
Slavin S, Nagler A, Naparstek E, Kapelushnik Y, Aker M, Cividalli G, Varadi G, Kirschbaum M, Ackerstein A, Samuel S, Amar A, Brautbar C, Ben-Tal O, Eldor A, Or R (1998) Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases. Blood 91: 756–765
Spaner D, Raju K, Rabinovich B, Miller RG (1999) A role for perforin in activation-induced T cell death in vivo: Increased expansion of allogeneic perforin-deficient T cells in SCID mice. J Immunol 162: 1192–1199
Speiser DE, Schneider R, Hengartner H, MacDonald HR, Zinkernagel RM (1989) Clonal deletion of self-reactive T cells in irradiation bone marrow chimeras and neonatally tolerant mice. Evidence for intercellular transfer of Mls-1a. J Exp Med 170: 559–600
Sundstedt A, Grundstrom S, Dohlsten M (1998) T cell- and perforin-dependent depletion of B cells in vivo by staphylococcal enterotoxin A. Immunology 95: 76–82
Thomas DA, Du C, Xu M, Wang X, Ley TJ (2000) DFF45/ICAD can be directly processed by granzyme B during the induction of apoptosis. Immunity 12: 621–632
Trapani JA, Jans PJ, Smyth MJ, Froelich CJ, Williams EA, Sutton VR, Jans DA (1998) Perforin-dependent nuclear entry of granzyme B precedes apoptosis, and is not a consequence of nuclear membrane dysfunction. Cell Death Diff 5: 488–496
Trauth BC, Klas C, Peters AMJ, Matzku S, Möller P, Falk W, Debatin KM, Krammer PH (1989) Monoclonal antibody-mediated tumor regression by induction of apoptosis. Science 245: 301–305
Ushmorov A, Ratter F, Lehmann V, Dröge W, Schirrmacher V, Umansky V (1999) Nitric oxide-induced apoptosis in human leukemic lines requires mitochondrial degradation and cytochrome C release. Blood 93: 2342–2352
Walczak H, Degli-Esposti MA, Johnson RS, Smolak PJ, Waugh JY, Boiani N, Timour TS, Gerhart MJ, Schooley KA, Smith KA, Goodwin RG, Rauch CT (1997) TRAIL-R2: a novel apoptosis-mediating receptor for TRAIL. EMBO J 16: 5386–5397
Walczak H, Miller RE, Ariail K, Gliniak B, Griffith TS, Kubin M, Chin W, Jones J, Woodward A, Le T, Smith C, Smolak P, Goodwin RG, Rauch CT, Schuh JC, Lynch DH (1999) Tumoricidal activity of tumor necrosis factor-related apoptosis-inducing ligand in vivo. Nature Med 5: 155–162
Wiley SR, Schooley K, Smolak PJ, Din WS, Huang C-P, Nicholl JK, Sutherland GR, Smith TD, Rauch CT, Smith CA (1995) Identification and characterization of a new member of the TNF family that induces apoptosis. Immunity 3: 673–682
Yasukawa M, Ohminami H, Kasahara Y, Ishida Y, Fujita S (2000) Granule exocytosis, and not the Fas/Fas ligand system, is the main pathway of cytoxicity mediated by alloantigen-specific CD4+ as well as CD8+ cytotoxic T lymphocytes in humans. Blood 95: 2352–2355
Zheng L, Fisher G, Miller RE, Peschon J, Lynch DH, Lenardo MJ (1995) Induction of apoptosis in mature T cells by tumor necrosis factor. Nature 377: 348–351
Zhou Q, Snipas S, Orth K, Muzio M, Dixit VM, Salvesen GS (1997) Target protease specificity of the viral serpin CrmA. Analysis of five caspases. J Biol Chem 272: 7797–7800
Acknowledgements
We thank Dr T Sebens for critical reading of the manuscript and helpful discussions. We also thank H Stahl and D Suess for the production of recombinant proteins. Grant sponsor: Dr Mildred Scheel Stiftung (project number 10-0980).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Müerköster, S., Weigand, M., Choi, C. et al. Superantigen reactive Vβ6+ T cells induce perforin/granzyme B mediated caspase-independent apoptosis in tumour cells. Br J Cancer 86, 828–836 (2002). https://doi.org/10.1038/sj.bjc.6600104
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600104
Keywords
This article is cited by
-
Complete remission of cancer in late-stage disease by radiation and transfer of allogeneic MHC-matched immune T cells: lessons from GvL studies in animals
Cancer Immunology, Immunotherapy (2014)
-
SEC2-induced superantigen and antitumor activity is regulated through calcineurin
Applied Microbiology and Biotechnology (2013)