Abstract
Data Sources
PubMed, Ovid (including OLDMedline), Google Scholar Beta, the Cochrane Library and references of identified articles were used to identify data sources.
Study selection
Studies were included if they involved more than 10 adults, a followup of greater than 6 months, and mandibular advancement by bilateral sagittal split osteotomy (BSSO) with rigid internal fixation. Studies that included another surgical intervention (eg, Le Fort I osteotomy), syndromic or medically compromised patients, case reports, case series, descriptive studies, review and opinion articles or abstracts were excluded.
Data extraction and synthesis
The following data items were extracted: year of publication, study design, followup, number and mean age of patients, ethnic background of patients, number of surgeons operating, type of rigid internal fixation, use of MMF (maxillomandibular fixation), use of genioplasty, mean advancement, mean relapse, correlations between relapse and different variables, proportion of patients with more than 2 mm of sagittal relapse, and authors' conclusions. A quality assessment of the included studies was undertaken following selection. Studies were categorised as medium or low quality based on study design, sample size, selection descriptions, withdrawals, valid methods, confounding factors, method error analysis, blinding in measurements and adequate statistics. None of the included studies met the criteria of the high-quality category.
Results
Twenty-four articles were finally included, comprising six prospective and 18 retrospective studies. The range of postoperative study records was 6 months to 12.7 years. The short-term relapse for bicortical screws was between 1.5 and 32.7%, for miniplates between 1.5 and 18.0%, and for bioresorbable bicortical screws between 10.4 and 17.4%, at point B (the deepest concavity on the anterior profile of the maxilla). The long-term relapse for bicortical screws was between 2.0 and 50.3%, and for miniplates between 1.5 and 8.9%, at point B.
Conclusions
To obtain reliable scientific evidence, further short-term and long-term research into BSSO advancement with rigid internal fixation should exclude additional surgery, ie, genioplasty or maxillary surgery, and include a prospective study or randomised controlled clinical trial (RCT) design with correlation statistics.
Similar content being viewed by others
Commentary
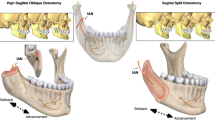
Mandibular advancement by BSSO is a commonly undertaken orthognathic procedure for the correction of mandibular retrognathia.1 It can be completed as a standalone procedure or combined, as required, with procedures such as genioplasty or maxillary osteotomy. It can also be undertaken for mandibular setback in the correction of mandibular prognathia, the stability of which was the subject of a previous review by the same authors in 2008.2 Before the advent of rigid internal fixation, intermaxillary fixation was used in osteotomy patients throughout bony healing. Today rigid internal fixation is used almost exclusively in BSSO procedures in the UK, but a number of different forms of fixation are in use including titanium and bioresorbable bicortical screws and miniplates.
This review aimed to determine the amount of relapse that might be expected in mandibular advancement BSSO within three groups of rigid internal fixation: bicortical screws, miniplates, or bioresorbable bicortical screws. Despite an extensive literature search in which 488 articles dealing with BSSO were identified, only 24 studies met the criteria for inclusion in this review. Studies were assessed for quality, with only six out of the 24 meeting medium-quality standards and the remainder were only of low quality. The quality assessment was not used as part of the inclusion criteria. Data on relapse as a proportion of the original horizontal mandibular movement at cephalometric points B and pogonion was classified as short-term if recorded at less than 18 months postsurgery and as long-term at more than 18 months postsurgery.
The striking feature of the results is the range of relapse rates within all three fixation groups in both short- and long-term studies. In the original review paper, the authors tentatively suggest that, “A greater number of studies with higher skeletal long-term relapse rates were seen in patients treated with bicortical screws instead of miniplates” although it is notable that they do not go as far as suggesting that miniplates have a lower long-term relapse rate. Because of the small number, varying quality and heterogeneity of included studies and their results, any apparent difference should be interpreted with caution. The fact that relapse rates vary so greatly between studies within each group, and that little difference can be demonstrated between the three groups, may suggest that there are other, potentially more important, factors than the type of rigid internal fixation that contribute to relapse. The authors themselves describe the multifactorial aetiology of relapse and rank the factors influencing relapse in terms of the strength of evidence for one factor over another. It should be kept in mind, however, that the evidence supporting the majority of these factors is poor and therefore the ranking of factors by the relative strength of their evidence may be meaningless. The second strongest factor is listed as “Type and material of fixation” but it must be appreciated that this ranking is on the basis of evidence of increased stability when using rigid internal fixation over wire fixation, rather than of evidence of differences between rigid internal fixation types and materials. Another point of note is that the authors have not separated studies in which lag (compression) screws have been used from those using bicortical (noncompression) screws. A difference between the relapse rates of compression screws and bicortical screws may well be as great as any difference between these screw types and miniplates.
The evidence of variation in relapse rates between rigid internal fixation methods would appear relatively equivocal at the present time. This review is useful in establishing the current position and highlighting the need for further high quality, prospective RCT in this area. It also provides an important reminder of the potential for relapse with all BSSO techniques and the need to appreciate this in treatment planning and in the consent process.
Practice points
-
The aetiology of relapse in mandibular advancement BSSO is multifactorial.
-
The evidence of variation in relapse rates between rigid internal fixation methods is currently unclear.
-
Relapse occurs with all methods of rigid internal fixation which should be borne in mind when planning treatment and in the consent process.
References
Ward Booth P (Ed). Maxillofacial Surgery 2nd Edn. London: Churchill Livingstone; 2007: pp1247–1256.
Joss CU, Vassalli IM . Stability after bilateral sagittal split osteotomy setback surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg 2008; 66: 1634–1643.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Dr Joss, Section de Médecine Dentaire, Faculté de Médecine, University of Geneva, Rue Barthélémy-Menn 19, CH-1205 Geneva, Switzerland. E-mail: christof.joss@medecine.unige
Joss CU, Vassalli IM. Stability after bilateral sagittal split osteotomy advancement surgery with rigid internal fixation: a systematic review. J Oral Maxillofac Surg 2009; 67: 301–313
Rights and permissions
About this article
Cite this article
Hughes, R. Relapse following bilateral sagittal split osteotomy with rigid internal fixation. Evid Based Dent 10, 81–82 (2009). https://doi.org/10.1038/sj.ebd.6400671
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400671