Abstract
This study determines whether genetic variability in the gene-encoding factor V contributes to differences in pre-eclampsia susceptibility. Allele and genotype frequencies of three single-nucleotide polymorphisms (SNPs) in the factor V gene leading to nonsynonymous changes (M385T in exon 8, and R485K and R506Q (Leiden mutation) in exon 10) were studied in 133 Caucasian women with pre-eclampsia and 112 healthy controls. Single-point analysis was expanded to haplotype analysis, and haplotype frequencies were estimated using an expectation-maximization algorithm. Comparison of single-point allele and genotype distributions of SNPs in exons 8 and 10 of the factor V gene revealed statistically significant differences in R485K allele (P=0.003) and genotype (P=0.03) frequencies between the patients and the control subjects. The A allele of SNP R485K was over-represented among the patients (12%) vs the control subjects (4%), at an odds ratio (OR) of 2.8 (95% confidence interval (CI) 1.2–6.2) for combined A genotypes (GA+AA vs GG). Allele and genotype differences between the patients and control subjects as regards M385T and Leiden mutation were not significant. In haplotype estimation analysis, there was a significantly elevated frequency of haplotype T-A-G encoding the M385-K485-R506 variant in the pre-eclamptic group vs the control group (P=0.01), at an OR of 2.6 (95% CI 1.2–5.5). We conclude that the T-A-G haplotype was more frequent among the patient group than in the control group, and genetic variations in the factor V gene other than the Leiden mutation may play a role in disease susceptibility.
Similar content being viewed by others
Introduction
Dahlbeck et al assigned the factor V gene to chromosome region 1q23. Activated factor V (factor Va) is an essential cofactor for the factor Xa-catalyzed activation of prothrombin to the clotting enzyme thrombin.1,2 Activated protein C (APC) is a naturally occurring anticoagulant that selectively degrades coagulation factors Va and VIIIa.3 The factor V Leiden mutation, a common point mutation in the factor V gene, encoding substitution of arginine for glutamate at position 506 of the factor V molecule, has been reported to be the site where APC cleaves factor Va.4 The factor V Leiden mutation has been reported to be a significant risk factor for thrombophilia.5 In the same line of thought, APC resistance not due to factor V Leiden mutation has been identified as an independent risk factor for deep vein thrombosis, and interestingly, factor V R485K polymorphism has been found to be associated with a poor response to APC, and thrombotic and cardiovascular diseases, the less frequent A allele (K485) increasing the risk.6,7,8
During pregnancy an inherited predisposition to thromboembolic events has been associated with a number of adverse pregnancy outcomes such as fetal loss and pre-eclampsia.9,10 The central mechanism is probably endothelial cell injury and dysfunction resulting from fibrin deposition and the formation of microthrombi.11 Overall, the prevailing evidence suggests that the risk of pre-eclampsia is increased two- to six-fold in women carrying the factor V Leiden mutation. Recently, Watanabe et al12 reported that the R485K polymorphism of the factor V gene is associated with pre-eclampsia in Japanese women who lack the Leiden mutation entirely. In their study, the G allele (R485) was associated with pre-eclampsia (0.76 vs 0.67).
The present study was designed to explore the relationship between genetic variation in coagulation factor V and the occurrence of pre-eclampsia in Finnish women, among whom there is a strong founder effect. Thus they are ideal for genetic association studies.13 Screening involved not only the Leiden mutation, but also the M385T and R485K polymorphisms, the latter of which has previously been found to be associated with pre-eclampsia in Japan. We further analyzed the haplotype structure in the critical area covering a region in the proximity of the Leiden mutation.
Materials and methods
Written approval for the study was obtained from the Ethics Committee of Kuopio University Hospital and the Institutional Review Board approved the protocol. All subjects gave written informed consent, which was documented.
Information was collected retrospectively in connection with 133 consecutive pre-eclamptic singleton pregnancies and 112 healthy control women who delivered at Kuopio University Hospital between January 1997 and December 1998. Using the Birth Registry at Kuopio, pre-eclamptic subjects were contacted and blood samples were drawn. At the same time, blood samples were collected from controls who had given birth at the same hospital after uncomplicated pregnancies and who had had at least two normal pregnancies, including the current one. From the controls, blood was drawn for DNA analysis at enrolment. To ensure homogeneity of the genetic background, controls originating from a regional population with no clinical signs of the disorder were enrolled by random selection in this study. The study and control groups were derived only from women with singleton deliveries at our hospital during the study period. Pre-eclampsia was defined as the development of hypertension and new-onset proteinuria (>300 mg of urinary protein in 24 h) in the absence of urinary tract infection after the 20th week of gestation in women with no proteinuria at baseline. Hypertension was defined according to current guidelines that accept 140 and/or 90 mm Hg of systolic and diastolic pressure (Korotkoff phase V), respectively, or higher, as hypertension, when measured on two consecutive occasions at least 24 h apart (Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy).14 Women with a previous history of chronic hypertension, renal disease or diabetes mellitus were excluded from the study.
Two polymorphisms in the F5 gene, a transition of T to C in exon 8 leading to the replacement of methionine with threonine (M385T) and a transition of G to A in exon 10 leading to the replacement of arginine with lysine (R485K), were detected using PCR-RFLP. The target DNA sequence in exon 8 was amplified using primers 5′-ACA TAC AGT GAA TCC CAG TA-3′ and 5′-ATG AGC ATC TTT TTC TTT TA-3′. The incubation mixture contained 50 ng of genomic DNA, 10 pmol of each amplification primer, 5 nmol each of four deoxynucleotide triphosphates, 1 U AmpliTaq Gold™ DNA polymerase (Roche, Branchburg, NJ, USA), 10 mM Tris-HCl (pH 8.3 at 25°C), 50 mM KCl and 1.5 mM MgCl2 in a reaction volume of 25 μl. The cycling protocol included initial denaturation at 95°C for 3 min, followed by a cycle of 95°C for 1 min, 51°C for 1 min and 72°C for 1 min. A total of 34 cycles were carried out, with final extension at 72°C for 10 min. For the detection of the M385T polymorphism, PCR mixtures containing an amplified 176-bp DNA region were incubated with 5 U of RsaI enzyme (Promega, Madison, WI, USA), 1 × Buffer C (10 mM Tris-HCl, pH 7.9, 50 mM NaCl, 10 mM MgCl2 and 1 mM dithiothreitol) and acetylated bovine serum albumin (0.1 mg/ml) in a total volume of 30 μl for 3 h at 37°C. After digestion, the reaction mixtures were subjected to electrophoresis on 3% agarose gels and photographed under an UV transilluminator after staining with ethidium bromide. The PCR product of an M385 homozygote is digested into two fragments of 136 and 40 bp. In the case of a T385 homozygote, the PCR primers create an artificial restriction site for the RsaI enzyme in the PCR product leading to 117-, 40- and 19-bp fragments after digestion. For an M385T heterozygote, the restriction fragments are 136, 117, 40 and 19 bp.
The primers used for the amplification of the target DNA sequence in exon 10 of the F5 gene were 5′-ACC CAC AGA AAA TGA TGC CCA G-3′ and 5′-AAA ATA CCT GTA TTC CTC GCC TG-3′. The incubation mixture and the cycling protocol were similar to those used for exon 8, except that an annealing temperature of 57°C was used. The R485K polymorphism in exon 10 was detected by incubating the mixtures containing a PCR product with 2 U Alw26I enzyme (Promega), 1 × Buffer C and acetylated bovine serum albumin (0.1 mg/ml) in a total volume of 30 μl for 6 h at 37°C. A single Alw26I site is present in the 143-bp PCR product from the wild-type exon 10 allele, and hence 86- and 57-bp fragments are seen for an R485 homozygote. In the case of a K485 homozygote, the undigested 143-bp fragment is present. For an R485K heterozygote, three fragments are seen (143, 86 and 57 bp) after electrophoresis on 3% agarose gel.
Pronto™ primer extension assays (Savyon Diagnostics Ltd, Ashdod, Israel) were used for the detection of factor V Leiden mutation (G1691A leading to an R506Q substitution).
Two-tailed pooled t-tests were used to analyze continuous variables. Statistical analyses for comparing single-point allele and genotype frequencies were carried out using Pearson's χ2 test (two-sided asymptotic P-values), with SPSS 11.0 software. Odds ratios (ORs), as estimates of relative risk of disease, were calculated using 95% confidence intervals (CIs). We used an expectation-maximization (EM) algorithm to obtain estimated haplotype frequencies for factor V gene exon 8 and 10 polymorphisms (each haplotype consisting of three SNPs, and unknown gametic phase; Arlequin ver. 2.000 software). Haplotype frequency comparisons between the pre-eclamptic and control groups, with absolute chromosome numbers, were carried out using Fisher's exact test (two-sided P-values with Monte Carlo estimation at the 99% confidence level). Hardy–Weinberg distribution of genotypes in the pre-eclamptic and control groups, as well as pair-wise linkage disequilibrium (LD) analyses, were assessed using Arlequin ver. 2.000 software. A RxC program employing the Metropolis algorithm was used for the analysis of contingency tables to obtain unbiased estimates of exact P-values with standard errors (SEs) in haplotype analyses. The level of statistical significance was defined as P<0.05. Sample size and power assessments were performed using nQuery Advisor Release 3.0 software. We used frequency data from exon 4 genotypes to calculate the necessary sample sizes to achieve a power of 80% and an α value of 0.05.
Results
The characteristics of the subjects and the clinical data are summarized in Table 1. In comparison with the controls, women with pre-eclampsia had higher systolic and diastolic blood pressure, a greater BMI and lower gestational age at delivery, with no significant difference in age.
We studied three SNPs in the factor V gene that lead to nonsynonymous changes: M385T, R485K and R506Q (Leiden mutation). Genotype and allele distributions of these SNPs in the patients and controls are shown in Table 2. A statistically significant difference between patients and control subjects was observed in the genotype (P=0.03) and allele frequencies (P=0.003) of the R485K polymorphism, while the differences between patients and control subjects as regards the M385T polymorphism and the Leiden mutation were not significant. The A allele of SNP R485K, which encodes lysine, was over-represented among the patients (12%) vs the control subjects (4%) and the OR for combined A genotypes (GA+AA vs GG) was 2.8 (95% CI 1.2–6.2). In the case of SNP R485K, we found a significant deviation from Hardy–Weinberg equilibrium among the patient group (P=0.004), but not among the control group (P=0.19). This deviation was a consequence of over-representation of AA homozygotes among the patient group. Genotype frequencies of the other SNPs among the patient and control groups did not differ significantly from Hardy–Weinberg equilibrium.
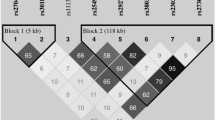
Haplotype frequencies of SNPs encoding M385T, R485K and R506Q were estimated separately in the patient and control groups (Table 3). We estimated haplotype frequencies by means of the maximum-likelihood method employing an EM algorithm and carried out haplotype association analysis. Rare haplotypes (<5%) were pooled in statistical analyses. Comparison of the overall haplotype distribution profiles revealed a statistically significant difference (P=0.03) between the pre-eclamptic women and the controls (Table 3). In single haplotype association analysis, the estimated frequency of the T-A-G haplotype encoding the M385-K485-R506 variant was greater in the patient group than in the control group (P=0.01), giving an OR of 2.6 (95% CI 1.2–5.5). To obtain unbiased estimates for the above-mentioned exact test P-values, the Metropolis algorithm was used to analyze overall (P=0.04; SE±0.004) and T-A-G (P=0.01; SE±0.001) haplotype contingency tables. Pair-wise LD analysis did not reveal significant LD between SNP pairs.
Discussion
The familial nature of pre-eclampsia clearly indicates a significant genetic component, and this genetic component probably comprises multiple gene variants each contributing a small effect.15 A number of investigators have demonstrated that pregnant women with thrombotic events have an increased frequency of genetic defects predisposing them to thrombosis.11,12,16,17,18,19 In this study, the candidate gene was selected on the basis of the previously reported association between obstetric disturbances and factor V gene polymorphism, and the data tested for significance using single-point as well as haplotype association analyses involving three intragenic SNPs. The main finding in this study was that the genotype and allele frequencies of the R485K polymorphism in the factor V gene differed significantly in the patient vs the control population. To further assess the role of intragenic SNPs of factor V, we performed a haplotype estimation analysis in which different allele combinations of SNPs were considered. The haplotype M-K-R was found in a significantly higher proportion of the pre-eclamptic patients, conferring a high risk of developing pre-eclampsia in individuals carrying this haplotype (OR=2.6; 95% CI 1.2–5.5). Interestingly, the frequency of the Leiden mutation was comparable in both groups and corresponded well to the previously known population frequency (4.2%).20
The present results may be explained by the fact that APC resistance may occur without the Leiden mutation, as shown in previous studies.21,22 The R485K polymorphism has been reported to be associated with thrombophilic and cardiovascular diseases, the less frequent A allele increasing the risk.21,22 This may reflect true functional significance of the less frequent A allele or it may merely reflect LD between the A allele and the actual predisposing alteration. Interestingly, the results of a study by Watanabe et al among pre-eclamptic Japanese women clearly show that the association is not brought about by the Leiden mutation, although they found strong LD over the chromosomal area of interest.12 However, in their study the increased risk of pre-eclampsia was confined to individuals heterozygous for the G variant, that is, women with the more frequent allele. Our results contrast with the findings in the study by Watanabe et al and showed unexpectedly that the A allele was associated with affected women in eastern Finland.
A positive genetic association does not necessarily indicate a predisposing genetic defect in the putative site, because the associated polymorphism site may be in LD with another alteration in the same gene or with alteration in another gene nearby. Furthermore, the functional significance of the variant amino acid at position 485 is still unresolved. All in all, the significant association that emerged between R485K polymorphism and pre-eclampsia may reflect a disease-modifying effect of another alteration in the factor V gene contributing to the actual risk that is in LD with the R485K polymorphism. Interestingly, we did not find significant LD between R506Q and R485K regardless of their close physical proximity. The fact that we did not detect significant LD values as regards R506Q and R485K could be a consequence of low minor allele frequency of the Leiden mutation, which subsequently affected the power of LD calculations.
The main limitations of this study are that we have a small data set and only Finnish women were studied. Power analysis showed that more than 2400 patients and controls would be necessary to have an 80% chance of showing a difference in Leiden mutation frequency associated with pre-eclampsia at a significance level of P<0.05. The present results may not be applicable to all populations and ethnic groups, but more homogeneous populations such as the relatively genetically isolated Finnish population have been proposed as possible alternatives to large sample sizes, because environmental variation might be lower and the genetic make-up of such populations is expected to be less complex owing to founder effects, thus improving the signal-to-noise ratio.13
In summary, we found that the less frequent amino-acid variant (lysine) at position 485 is a significant risk factor for pre-eclampsia rather than a protective factor against the disease.
As with all possible disease-modifying genes, their overall impact on the risk of pre-eclampsia is likely to remain small and hence their clinical relevance remains to be seen. The results of the present study contradicts the findings of Watanabe et al12 However, the significant association with the R485K polymorphism indicates that the factor V gene is one of the genes of interest in pre-eclampsia research, and genetic variants other than the Leiden mutation should also be investigated. Few studies on three-marker haplotypes of the factor V gene have been published in connection with different ethnic groups, although the statistically significant over-representation of the Leiden mutation in pre-eclamptic women is well established. Further studies also assessing the parental haplotypes are needed to investigate the effect of the R485K polymorphism of the factor V gene in other populations.
References
Dahlback B, Hansson C, Islam MQ et al: Assignment of gene for coagulation factor V to chromosome 1 in man and to chromosome 13 in rat. Somat Cell Mol Genet 1988; 14: 509–514.
Kane WH, Davie EW : Blood coagulation factors V and VIII: structural and functional similarities and their relationship to hemorrhagic and thrombotic disorders. Blood 1988; 71: 539–555.
Dahlback B, Carlsson M, Svensson PJ : Familial thrombophilia due to a previously unrecognized mechanism characterized by poor anticoagulant response to activated protein C: prediction of a cofactor to activated protein C. Proc Natl Acad Sci USA 1993; 90: 1004–1008.
Bertina RM, Koeleman BP, Koster T et al: Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature 1994; 369: 64–67.
Zoller B, Svensson PJ, He X, Dahlback B : Identification of the same factor V gene mutation in 47 out of 50 thrombosis-prone families with inherited resistance to activated protein C. J Clin Invest 1994; 94: 2521–2524.
Graf LL, Welsh CH, Qamar Z, Marlar RA : Activated protein C resistance assay detects thrombotic risk factors other than factor V Leiden. Am J Clin Pathol 2003; 119: 52–60.
Hiyoshi M, Arnutti P, Prayoonwiwat W et al: A polymorphism nt 1628G–>A (R485K) in exon 10 of the coagulation factor V gene may be a risk factor for thrombosis in the indigenous Thai population. Thromb Haemost 1998; 80: 705–706.
Le W, Yu JD, Lu L et al: Association of the R485K polymorphism of the factor V gene with poor response to activated protein C and increased risk of coronary artery disease in the Chinese population. Clin Genet 2000; 57: 296–303.
Rey E, Kahn SR, David M, Shrier I : Thrombophilic disorders and fetal loss: a meta-analysis. Lancet 2003; 361: 901–908.
Spina V, Aleandri V, Morini F : The impact of the factor V Leiden mutation on pregnancy. Hum Reprod Update 2000; 6: 301–306.
van Pampus MG, Dekker GA, Wolf H et al: High prevalence of hemostatic abnormalities in women with a history of severe preeclampsia. Am J Obstet Gynecol 1999; 180: 1146–1150.
Watanade H, Hamada H, Yamada N et al: Association analysis of nine missense polymorphisms in the coagulation factor V gene with severe preeclampsia in pregnant Japanese women. J Hum Genet 2002; 47: 131–135.
Peltonen L, Jalanko A, Varilo T : Molecular genetics of the Finnish disease heritage. Hum Mol Genet 1999; 8: 1913–1923.
National High Blood Pressure Working Group: Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol 2000; 183: S1–S22.
Arngrimsson R, Björnsson H, Geirsson R : Analysis of different inheritance patterns in preeclampsia/eclampsia syndrome. HypertensPregnancy 1995; 14: 27–38.
Grandone E, Margaglione M, Colaizzo D et al: Factor V Leiden, C>T MTHFR polymorphism and genetic susceptibility to preeclampsia. Thromb Haemost 1997; 77: 1052–1054.
Dizon-Townson DS, Nelson LM, Easton K, Ward K : The factor V Leiden mutation may predispose women to severe preeclampsia. Am J Obstet Gynecol 1996; 175: 902–905.
Lindoff C, Ingemarsson I, Martinsson G, Segelmark M, Thysell H, Astedt B : Preeclampsia is associated with a reduced response to activated protein C. Am J Obstet Gynecol 1997; 176: 457–460.
Rigo Jr J, Nagy B, Fintor L et al: Maternal and neonatal outcome of preeclamptic pregnancies: the potential roles of factor V Leiden mutation and 5,10 methylenetetrahydrofolate reductase. Hypertens Pregnancy 2000; 19: 163–172.
Pastinen T, Perola M, Ignatius J et al: Dissecting a population genome for targeted screening of disease mutations. Hum Mol Genet 2001; 10: 2961–2972.
Gandrille S, Greengard JS, Alhenc-Gelas M et al: Incidence of activated protein C resistance caused by the ARG 506 GLN mutation in factor V in 113 unrelated symptomatic protein C-deficient patients. The French Network on the behalf of INSERM. Blood 1995; 86: 219–224.
Helley D, Besmond C, Ducrocq R et al: Polymorphism in exon 10 of the human coagulation factor V gene in a population at risk for sickle cell disease. Hum Genet 1997; 100: 245–248.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faisel, F., Romppanen, EL., Hiltunen, M. et al. Susceptibility to pre-eclampsia in Finnish women is associated with R485K polymorphism in the factor V gene, not with Leiden mutation. Eur J Hum Genet 12, 187–191 (2004). https://doi.org/10.1038/sj.ejhg.5201124
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201124