Abstract
Few data are available on genotype–phenotype interactions among familial hypercholesterolemia (FH) patients in South European populations and there are no data about the influence of R3500Q mutation on lipoprotein phenotype compared to low-density lipoprotein receptor (LDLR) mutations. The objective of the study is to analyze the influence of mutations in the LDLR and apolipoprotein B (apoB) genes on lipoprotein phenotype among subjects clinically diagnosed of FH living in East Spain. In all, 113 FH index patients and 100 affected relatives were studied. Genetic diagnosis was carried out following a protocol based on Southern blot and PCR-SSCP analysis. A total of 118 FH subjects could be classified into three groups according to the type of LDLR mutations (null mutations, missense mutations affecting the ligand binding 3–5 repeat, and missense mutations outside this domain). In addition, the lipoprotein phenotype of these FH groups was compared with 19 heterozygous subjects with familial ligand-defective apoB (FDB), due to R3500Q mutation. FH patients carrying missense mutations affecting the ligand binding repeat 3–5 showed total and LDL cholesterol levels significantly higher than FH patients with missense mutations in other LDLR domains or FDB patients. FH subjects carrying null mutations showed lower high-density lipoprotein cholesterol plasma values compared to FH carrying missense mutations. FDB subjects showed the lowest total and LDL cholesterol plasma values. In conclusion, the type of LDLR gene mutation and R3500Q mutation influences the lipoprotein phenotype of FH population from East Spain.
Similar content being viewed by others
Introduction
Familial hypercholesterolemia (FH) is an autosomal dominant disease defined at the molecular level by the presence of mutations in the low-density lipoprotein receptor (LDLR) gene and characterized by markedly elevated low-density lipoprotein cholesterol (LDLc) levels, tendon xanthomata and increased risk of coronary heart disease (CHD).1,2,3,4 FH shows great variability in phenotypic expression, which may be influenced by factors such as age, gender, diet, type of LDLR mutations or other genes.5,6,7,8
The type of LDLR gene mutation has been associated to different phenotype expression,6,8,9 response to statins10,11 and risk of premature CHD.5 In Northern European FH populations, several studies have demonstrated that the type of mutation in the LDLR gene influences the FH phenotype expression.12,13,14,15 Affected individuals with LDLR mutations predicted to be severe, such as null mutations or mutations affecting the ligand-binding repeat 3–5 of the receptor, presented higher plasma levels of total and LDLc. In Southern European FH populations, only Bertolini et al16 have studied the relationships between the type of LDLR gene mutation and expression of the FH phenotype, as far as we know. These authors have reported that receptor-negative mutations are associated with higher plasma levels of total and LDLc compared to affected subjects with receptor-defective mutations. Altogether, these results suggest that DNA diagnosis could allow the study of genotype–phenotype interactions in terms of estimating the clinical severity and prognosis.
When compared with Northern Europeans, Spanish FH subjects present lower levels of plasma LDLc and lower prevalence of tendon xanthomata,17 making genetic diagnosis even more important. We have previously described large and point mutations in Spanish FH subjects and analyzed the influence of LDLR gene mutation on treatment response in our population.18,19,20 FH subjects carrying large mutations affecting promotor region have higher LDLc plasma values. FH subject carriers of null mutations showed a poorer response to simvastatin treatment than FH carriers of no null mutations.
Familial ligand-defective apolipoprotein B (apoB)-100 (FDB) is an autosomal dominant inherited disease due to mutations in the apoB gene.21 It is characterized by elevated plasma total and LDLc levels and premature CHD. Three mutations (R3500Q, R3500W and R3531C) are mostly responsible for the disease by reducing the binding of LDL particles to the LDLR.21,22 The R3500Q mutation was the first described and is the most prevalent, while other point mutations (R3500W and R3531C) are rare causes of FDB.23,24 The prevalence of FDB has been estimated to be approximately 1/500 in North America,22 whereas in Europe seems to be high in the Northwestern part of Switzerland (1/114), Eastern France and Southern Germany22,25,26 and low in Italy and Spain. Miserez et al27 proposed that FDB emerged from mesolithic ancestors of Celtic people.
FDB is clinically indistinguible from FH. However, the plasma LDLc levels in age-matched FDB heterozygotes vary over a wide range and, in some families, heterozygous carriers of the R3500Q mutation show normal LDLc plasma levels.21,25
In the Spanish population, we have recently described the first FDB family and predicted a low prevalence of this disease, since only one FDB out of 113 FH index patients was detected.26 On the contrary, and due to a founder effect in an isolated region of the Valencia province, we have been able to identify seven affected pedigrees and 19 FDB heterozygotes and one homozygote.28 This has made possible to compare the phenotype of this group of patients with that of FH subjects.
The present study was undertaken to evaluate the influence of the LDLR gene mutation type and the R3500Q mutation of the apoB gene on the lipoprotein phenotype in a South European population where few data on this issue were available up to now.
Subjects and methods
Subjects
The study population consisted of a total of 213 clinically diagnosed FH subjects: 113 index patients and 100 affected relatives that had been referred to our Lipid Clinic (Table 1). All subjects were Caucasian and lived in the Valencia region. The institutional ethics committee from our institution approved the protocol and all subjects gave written informed consent to enter the study.
Diagnostic criteria for FH included: plasma levels of total and LDLc above the 95th percentile corrected for both age and sex,29 presence of tendon xanthomata, CHD in the index patient or in a first-degree relative, and bimodal distribution of total and LDLc levels in the family, indicating an autosomal dominant pattern of phenotype IIa.
A complete medical history and physical examination were obtained in all participants. Body mass index (BMI) was calculated as weight divided by height squared (kg/m2). Blood pressure was measured with a von Recklinghausen sphygmomanometer in the sitting position and after a 5-min rest. The mean value of three measurements was considered. CHD was diagnosed if there was a documented history of previous myocardial infarction and/or coronary artery bypass surgery, or angioplasty, or history of angina pectoris and alterations in the stress ECG.
One of the clinically defined FH index patients was found to be a carrier of the R3500Q mutation of the apoB gene (1/113 FH index patients), responsible for FDB.26 Extending the study to seven affected pedigrees, we could identify 19 heterozygotes for the R3500Q mutation and one homozygote.26,28
Laboratory methods
Measurement of lipids and lipoproteins
After a 12–14 h fast and in basal situation (4 weeks without treatment with drugs that affect lipid metabolism), blood samples were drawn from an antecubital vein in tubes containing EDTA (Vacutainer) and were centrifuged within 4 h. Plasma was stored at 4°C for a maximum of 3 days. Cholesterol and triglyceride levels were measured by enzymatic techniques.30,31 High-density lipoprotein cholesterol (HDLc) was measured after precipitation of apoB-containing lipoproteins with polyanions,32 and very-low-density lipoprotein cholesterol (VLDLc) after separation of VLDL (d<1.006 g/ml) by ultracentrifugation.33 The LDLc was calculated by subtraction of VLDL and HDL cholesterol from total cholesterol (TC). Total plasma apoB was measured by immunoturbimetry.34 Plasma Lp(a) concentrations were determined by ELISA.35 The coefficients of variation for lipids and lipoproteins were <5%.
Genetic methods
DNA extraction was performed by a standard procedure. Genetic diagnosis of FH was previously established through identification of mutations of LDLR gene by Southern blot analysis18 and DNA sequencing of abnormal SSCP bands.20 Screening for the apoB mutations was performed by PCR amplification, as described by Schuster et al,36 and SSCP analysis;20 DNA samples carrying the mutations R3480P, R3500Q, R3500W and R3531C, responsible for FDB, were used as controls.
Genotyping for the ApoE polymorphisms was performed following the method described by Hixon and Vernier37 with minor modifications.
Statistical analysis
Data were analyzed with the Statistical Package for the Social Sciences (SPSS 6.1. 3 for Windows) and expressed as mean±standard deviation (SD). The mean values of quantitative variables were compared with one-way ANOVA. Proportions were compared with contingency tables and the χ2 test or the Fischer's exact test (n<5).
ANCOVA analysis was used to estimate the independent contributions of the different LDLR gene mutations, age, gender and BMI to the mean baseline lipid values.
Results
Genetic diagnosis of FH and FDB
The genetic diagnosis of FH was previously established using a three-step protocol that screened mutations at the apoB gene, responsible for FDB, and major rearrangements and minor or point mutations in the LDLR gene, responsible for FH.18,20 Only one R3500Q mutation carrier was identified among the 113 FH index patients.20 The sample was screened for major rearrangements in the LDLR gene by Southern blot analysis. Five rearrangements were detected and characterized,18 two of them were due to duplications of internal regions of the gene (FH Valencia-2 and FH Valencia-3), whereas the rest were caused by partial deletions, which eliminate the promoter region in two cases (FH Valencia-1 and -5). The mRNA analysis of the alleles with internal rearrangements (FH Valencia-2, -3 and -4) indicated that these resulted in in-frame alterations of the RLDL gene.18 Thus, FH Valencia-1 and -5 may be classified as null mutations and FH Valencia-2, -3 and -4 as defective mutations.
SSCP analysis of the LDLR gene was used to screen for point and minor mutations. A total of 42 minor mutations causing FH were identified; a detailed description of them can be found in a previous report.20
Effect of LDLR gene and R3500Q mutations on plasma lipids and lipoproteins
FH subjects were classified into four groups according to the type of mutation. Group 1 included 45 subjects with null mutations; group 2, 13 subjects with missense mutations affecting ligand binding 3–5 repeat; group 3, 60 subjects with missense mutation not affecting this domain; and group 4, 19 heterozygotes with the R3500Q mutation in the apoB gene.
Mutations in the LDLR gene were considered null in the case of: (a) major rearrangements deleting the promoter region (FH Valencia-1 and -5), or (b) small mutations producing stop codons (W-18X, E10X, Q133X) or frameshifts in the LDL open reading frame (112insA, 790delATGA). Subjects with null mutations included: FH Valencia-1 (n=4), FH Valencia-5 (n=8), W-18X (n=10), E10X (n=2), Q133X (n=2), 112insA (n=15) and 790delATGA (n=4) (see Figure 1).
Missense mutations in the exon 4 of the LDLR gene may affect the role of the binding repeat 3–5 region of the LDLR. The missense mutations used in this study were: C95R (n=4), E119K (n=2), P160R (n=3), D200G (n=1) and S205P (n=3) (Figure 1). Carriers of S156L (n=5) were not included in this group because this mutation of exon 4 abolishes the binding of LDL, but not that of VLDL, causing only a mild reduction of the receptor function in vitro.15
Missense mutations classified as no affecting the ligand binding repeat 3–5 region were: C68W (n=6), Q71E (n=2), E80K (n=3), E246A (n=3), E256K (n=4), D280G (n=4), Y354C (n=2), C358Y (n=11), R395W (n=8), N407K (n=1), T413R (n=12), G528V (n=2), D679G (n=2) and N804K (n=2) (see Figure 1).
Finally, as previously mentioned, group 4 included 19 heterozygotes with the R3500Q mutation, which is responsible of FDB.
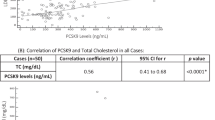
Plasma lipid and apoB values at baseline of patients classified according to their respective mutation type are shown in Table 2. No differences were found between the four groups with respect to age, BMI, gender distribution, presence of CHD, and APOE genotype distribution. Significant differences were observed with respect to TC and LDLc depending on the type of LDLR gene mutation. The mean plasma TC and LDLc levels were significantly higher in subjects with missense mutations affecting the binding repeat 3–5 domain, whereas the lowest values were found in the FDB group. No statistical differences were found between groups in plasma triglycerides (TG) and VLDL values. HDLc values in the null mutation group were significantly lower than in the missense mutation group. In order to control covariables we have also used the ANCOVA analysis. The intersubjects effect of the type of LDLR mutation on HDLc plasma values was not significantly different (P=0.66) when BMI was included as covariate and gender as independent variable.
Interestingly, in the whole group, the ANCOVA analysis showed that the type of LDLR mutation (P=0.006, 0.014), but not age or gender, had an independent influence on TC and LDLc plasma values.
Discussion
This is the second study carried out in a South European FH population aimed to analyze the relationships between the type of mutation affecting genes involved in lipid metabolism (the LDLR and ApoB genes) and phenotype. Our results indicate that the type of LDLR gene mutation has an impact on lipoprotein phenotype. The FH group with missense mutations affecting the binding repeat 3–5 domain (group 2) presents the highest TC and LDLc plasma concentrations, which determines a significant difference with groups 3 and 4 (P<0.05). However, the TC and LDLc values of the group with null mutations (group 1) were not statistically different than those of the other groups. On the other hand, FDB subjects showed the lowest TC and LDLc plasma values.
Our results are partially in agreement with previous data from Northern European FH populations. Thus, Gudnasson and Humphries15 reported that FH subjects with null mutations and mutations affecting repeat 5 had the highest mean LDLc plasma values. Sun et al12 showed that carriers of LDLR mutations predicted to be ‘severe’ (like null mutations or mutations that affect exon 4 repeat 3–5) have higher plasma TC and LDLc values and will not decrease lipid levels with treatment to the same extent than carriers of ‘mild mutations’. Finally, a study performed by Graham et al14 indicated that families with LDLR defects had higher total and LDLc plasma levels and higher incidence of xanthomas, than those with FDB.
Our study expands the few data available from South European FH populations about genotype–phenotype relationships. As far as we know, only Bertolini et al16 has addressed this issue. They studied 282 FH subjects from Italy, and identified 71 LDLR gene mutations responsible for the disease. Separating the molecularly defined FH subjects into two groups (receptor negative and receptor defective), they showed that FH subjects with receptor-negative mutations had higher TC plasma values (18%) and lower HDLc (−5%) than subjects in the receptor-defective group. The percentage of xanthomas and CHD in the receptor-negative group was two-fold higher than in the receptor-defective group.
All these observations suggest that different mutations of the LDLR gene are associated with differences in plasma lipid levels, although the basis for these differences are not clear. One possible explanation could be that upregulation of the wild-type LDLR allele was affected by the nature of the mutant allele, or that some defective mutations had residual LDLR activities13,14 On the other hand, genetic variability due to DNA polymorphisms of the wild type allele could quantitatively influence LDLc concentrations, as has been reported by Bétard et al38 in French Canadian FH women carrying the French Canadian 10 kb deletion, which may further complicate the interpretation of data.
One could expect that null mutations where nonreceptor is expressed and missense mutations affecting the binding domain will correlate with a severe phenotype, compared to other mutations where residual activity or expression of the receptor will be predicted. In contrast to this hypothesis, the results of previous studies14,15,39,40 indicate that FH patients carrying null mutation not always have the highest TC and LDLc plasma values. In most studies, FH subject carriers of a mutation predicted to be severe (not only null mutations) or that affects five repeat of the binding domain region have the most atherogenic lipid profile (higher plasma values of TC and LDLc). This is consistent with our results. In our study, we have found that FH patients carrying mutations predicted to be severe (null plus missense mutations affecting the binding repeat 3–5 region) have the worst lipid phenotype (higher plasma values of TC and LDLc and lower HDLc). The differences found in the revised studies could be explained by methodological differences, selection vias and the classification used for LDLR gene mutations.
We have not found statistically significant differences in TC and LDLc plasma values between the null mutation group (group 1) and the group with missense mutations affecting 3–5 binding repeat (group 2). Similar results have been previously demonstrated.14,15,40 One possible explanation is that FH patient carriers of null mutations (predicted to be severe) only express the normal receptor in the membrane of their cells. In contrast, FH patient carriers of the missense mutations express both the normal receptor and the altered receptors. This situation could facilitate a local competition between both receptors so that the internalization process could be affected. In addition, in the case of missense mutations affecting the 3–5 repeat, the situation would worsen, because the affected protein could not bind the apoB.
Another possibility is that, in group 3 (missense mutations not affecting the binding repeat 3–5 region), we could have included some mutations affecting the binding domain (missense mutations localized in exon 3 and 6), which could increase the average values of TC and LDLc of the entire group.
Finally, we cannot exclude differences in lipid profiles due to the influence of environmental or other genetic factors in our FH population. It should be noted that interaction with other genes41 and environmental factors42 could also influence the phenotype in FH patients. Pimstone et al42 have demonstrated that Chinese FH heterozygotes living in Canada exhibit a similar phenotype to that of other FH patients from Western societies, and different to those living in China. Leitersdorf et al.43 have shown the important effect of environmental factors like diet, physical activity, weight and others on the lipid phenotype in FH patients. Finally, the contribution of the ApoE genotype has been studied by Bertolini et al.16 These authors have reported a lowering effect of the e2 allele, and a raising effect of the e4 allele on the LDL cholesterol levels in both receptor-negative and -defective groups. In our study, the effects of environment (age, gender, BMI) and genetic factors (apoE genotype) that might modulate the lipid phenotype of FH or FDB subjects appear similar in the four groups.
On the other hand, and in agreement with Sijbrands et al44 and Bertolini et al,16 our FH subjects with null mutations showed plasma HDLc values significantly lower than those carrying missense mutations. Our observation on HDLc values suggests that the LDLR could be important in HDL metabolism of FH patients. The role of the LDLR on the clearance of remnant chylomicrons and VLDL particles could explain the HDLc plasma levels found in our group of FH subjects. In recent human studies, there was a markedly delayed clearance of retinol-labelled triglyceride-rich lipoproteins following an oral fat load in six Japanese homozygous FH subjects. In addition, the binding and clearance of chylomicron remnants by fibroblasts was substantially decreased in the homozygous FH group.45 Along the same lines, Castro-Cabezas et al46 reported, in heterozygous FH subjects, a two-fold delay in the area under the curve for clearance of remnant particles. Thus, it is possible that FH subjects with null mutations would have a lower clearance of remnant particles (chylomicron and IDL) and, as a consequence, lower HDLc concentrations. In addition, this subgroup of FH presented the highest risk of CHD in the study of Vohl et al.5
Different studies in North European populations47,48 have demonstrated that FDB subjects have lower total and LDLc plasma values than FH subjects. This is also the case in our study done in a South European population. The explanation for these differences has been attributed to the increased clearance of LDL precursors that has been observed in heterozygous and homozygous FDB patients.49
There are different possible classifications of FH according to the type of LDLR mutations.12,13,14,15,16 An alternative is to classify them into two groups (receptor negative and receptor defective). The problem is that the defective mutations group can include severe or mild mutations, limiting the study of genotype–phenotype relationship in FH subjects.
Our study points out, in a South European outbreed FH population, that the type of LDLR mutation and the R3500Q mutation of the apoB gene have an impact on the lipid phenotype expression. In the general population, a direct relationship exists between the magnitude of hypercholesterolemia and prevalence and incidence of CHD, as well as onset of symptoms. Therefore, the differences in TC and LDLc, found between molecularly defined FH subjects, could explain the different risk for CHD observed in these patients. Moreover, Vohl et al5 and Bertolini et al16 have demonstrated that FH subjects carrying a receptor-negative mutation have an increased risk for CHD compared to receptor-defective subjects. In addition, Jansen et al50 have demonstrated that LDLc plasma values alone could not account for the difference in CHD risk in these FH subjects.
We have not found significant differences in CHD prevalence between the groups. This can be attributed to the low number of subjects studied that limited the power of the study to investigate this issue.
Our results and those of others5,8,9,11,12,15,16 suggest that identification of mutations in the LDLR gene may allow a better assessment of clinical expression in these subjects with high CHD risk. In this sense, prospective studies should be performed to evaluate further the impact of genotype on severity of FH. In addition, the genetic diagnosis and molecular characterisation of LDLR gene mutations will allow a better assessment of response to treatment, prevention and family screening in these subjects.
References
Brown MS, Goldstein JL : A receptor-mediated pathway for cholesterol homeostasis. Science 1986; 232: 34–47.
Hobbs H, Brown MS, Goldstein JL : Molecular genetics of the LDL receptor gene in familial hypercholesterolemia. Hum Mutat 1992; 1: 445–466.
Varret M, Rabes JP, Thiart R et al: LDLR database (second edition): new additions to the database and the software, and results of the first molecular analysis. Nucl Acid Res 1998; 26: 248–252.
Wilson DJ, Gahan M, Haddad L et al: A world wide website for LDLR gene mutations in FH: sequence-based, tabular, and direct submission data handling. Am J Cardiol 1998; 81: 1509–1511.
Volh MC, Gaudet D, Moorjani S et al: Comparison of the effect of two low-density lipoprotein receptor class mutations on coronary heart disease among French–Canadian patients heterozygous for familial hypercholesterolemia. Eur J Clin Invest 1997; 27: 366–373.
Hoeg JM : Homozygous familial hypercholesterolemia: a paradigm for phenotypic variation. Am J Cardiol 1993; 72: 11D–14D.
Ferrières J, Lambert J, Lussier-Cacan S, Davignon J : Coronary artery disease in heterozygous familial hypercholesterolemia patients with the same LDL receptor gene mutation. Circulation 1995; 92: 290–295.
Kotze MJ, de Villiers WJS, Stein K et al: Phenotypic variation among familial hypercholesterolemic heterozygous for either one of two Afrikaner founder LDL receptor mutations. Arterioscle Thromb 1993; 13: 1460–1468.
Gudnason V, Day INM, Humphries SE : Effect on plasma lipid levels of different classes of mutations in the low-density lipoprotein receptor gene in patients with familial hypercholesterolemia. Arterioscle Thromb 1994; 17: 1717–1722.
Vuorio AF, Ojala JP, Sarna S, Turtola H, Tikkanen MJ, Kontula K : Heterozygous familial hypercholesterolaemia: the influence of the mutation type of the low-density-lipoprotein receptor gene and PvuII polymorphism of the normal allele on serum lipid levels and response to lovastatin treatment. J Intern Med 1995; 237: 43–48.
Leren TP, Hjermann I : Is responsiveness to lovastatin in familial hypercholesterolaemia influenced by the specific mutation in the low density lipoprotein receptor gene? Eur J Clin Invest 1995; 25: 967–973.
Sun XM, Neuwirth C, Patel DD, Knight BL, Soutar AK, with the familial hypercholesterolemia regression study group: Influence of genotype at the low density lipoprotein receptor gene locus of the clinical phenotype and response to lipid lowering drug therapy in heterozygous familial hypercholesterolemia. Atherosclerosis 1998; 136: 175–185.
Moorjani S, Roy M, Torres A et al: Mutations of low density lipoprotein receptor gene, variation in plasma cholesterol, and expression of coronary heart disease in homozygous familial hypercholesterolemia. Lancet 1993; 341: 1303–1306.
Graham CA, McClean E, Ward AJM et al: Mutation screening and genotype: phenotype correlation in familial hypercholesterol-emia. Atherosclerosis 1999; 147: 309–316.
Gudnasson V, Humphries SE : Effect on plasma lipid levels of different classes of mutations in the low density lipoprotein receptor gene in patients with familial hypercholesterolemia. Arterioscle Thromb 1994; 14: 1717–1722.
Bertolini A, Cantafora A, Averna M, Cortese C, Motti C, Martini C : Clinical expression of familial hypercholesterolemia in cluster of mutations of the LDL receptor gene that cause a receptor defective or receptor negative phenotype. Arterioscle Thromb Vasc Biol 2000; 20: e41–e52.
Villaverde CA, Sardá P, Vallbé JC et al: Manifestaciones clínicas de la hipercolesterolemia familiar en una población mediterránea. Med Clin (Barna) 1999; 113: 521–525.
Chaves FJ, Real JT, García-García AB et al: Large rearrangements of the LDL receptor gene and lipid profile in a Spanish population. Eur J Clin Invest 2001; 31: 309–317.
Chaves FJ, Real JT, García-García AB et al: Genetic diagnosis of familial hypercholesterolemia in a south European outbreed population: influence of low density lipoprotein (LDL) receptor gene mutations on treatment response to simvastatin in total, LDL and high density lipoprotein cholesterol. J Clin Endocrinol Metab 2001; 86: 4926–4932.
García-García AB, Real JT, Puig O et al: Molecular genetics of familial hypercholesterolemia in Spain: ten novel LDLR mutations and population analysis. Hum Mutat 2001; 454: 1–9.
Myant NB : Familial defective apolipoprotein B-100: a review, including some comparison with familial hypercholesterolemia. Atherosclerosis 1993; 104: 1–18.
Soria LF, Ludwig EH, Clarke HR, Vega GL, Grundy SM, McCarthy BJ : Association between a specific apoprotein B mutation and familial defective apo B-100. Proc Nat Acad Sci USA 1989; 86: 587–591.
Pullinger CR, Hennessy LK, Chatterton JE et al: Familial ligand-defective apolipoprotein B: identification of a new mutation that decreases LDL receptor binding affinity. J Clin Invest 1995; 95: 1225–1234.
Gaffney D, Reid JM, Cameron IM et al: Independent mutations at codon 3500 of the apolipoprotein B gene are associated with hyperlipidaemia. Arterioscle Thromb Vasc Biol 1995; 15: 1025–1029.
Rauh G, Séller C, Schuster H, Wolfgram G, Zöllnner N : Familial defective apolipoprotien B-100: a common cause of primary hyperlipemia. Clin Investigator 1995; 95: 1225–1234.
Real JT, Chaves FJ, Ascaso JF, Armengod ME, Carmena R : Estudio del defecto familiar de la apo B-100 en sujetos con el diagnóstico clínico de hipercolesterolemia primaria: identificación de la primera familia afectada en España. Med Clin (Barna) 1999; 113: 15–17.
Miserez AR, Muller PY : Familial defective apolipoprotein B-100: a mutation emerged in the Mesolithic ancestor of Celtic people? Atherosclerosis 2000; 148: 433–436.
Real JT, Chaves JF, Martín de Llano JJ et al: Identificación y caracterización del primer homocigoto español con defecto familiar de unión de la apolipoproteina B. Med Clin (Barna) 2001; 116: 138–141.
Gutierrez Fuentes JA, Gómez Gerique JA : Estudio DRECE. Dieta y riesgo de enfermedades cardiovasculares en España.; Ministerio de Sanidad y Consumo, Dirección General de Salud Pública, Madrid, 1993.
Allain CC, Poon LS, Chan CSG, Richmond W, Fu PC : Enzymatic determination of total serum cholesterol. Clin Chem 1974; 20: 470–475.
Ter Welle HF, Baartscheer T, Fiolet JWT : Influence of free glycerol on enzymatic evaluation of triglycerides. Clin Chem 1984; 30: 1102–1103.
Burstein M, Scholnick HR, Morfin R : Rapid method for the isolation of lipoproteins from human serum by precipitation with polyanions. J Lipid Res 1970; 11: 583–595.
Havel RJ, Eder HJ, Bragdon JH : The distribution and chemical composition of centrifugally separated lipoproteins in human serum. Eur J Clin Invest 1995; 34: 1345–1354.
Rosseneu M, Vercaemst R, Steinberg KK, Cooper GR : Some considerations of methodology and standarization of apolipo-protein B immunoassays. Clin Chem 1983; 29: 427–433.
Real JT, Ascaso JF, Chaves FJ et al: Plasma Lp(a) values in familial hypercholesterolemia and its relation to coronary heart disease. Nutr Metab Cardiovas Dis 1999; 9: 41–44.
Schuster H, Rauh G, Müller S, Keller C, Wolfram G, Zöllner N : Allele specific and asymetric polymerase chain reaction amplification in combination: a step polymerase chain reaction protocol for rapid diagnosis of familial defective apolipoprotein B-100. Ann Bioch 1992; 204: 22–25.
Hixon JE, Vernier DT : Restriction isotyping of human apolipoprotein E by gene amplification and cleavage with HhaI. J Lipid Res 1990; 31: 545–548.
Betard C, Kessling AM, Roy M, Davignon J : Influence of genetic variability in the non deletion LDL-receptor allele on phenotypic variation in French Canadian familial hypercholesterolemia heterozygotes sharing a ‘null’ LDL receptor gene defect. Atherosclerosis 1996; 119: 43–55.
Ward AJ, ÓKane M, Nicholls DP, Young IS, Nevin NC, Graham CA : A novel single base deletion in the LDLR gene (211delG): effect on serum lipid profiles and the influence of other genetic polymorphism in the ACE gene, apoE and apoB genes. Atherosclerosis 1996; 120: 83–91.
Jensen HK, Jensen LG, Hansen PS, Faergeman O, Gregersen N : The Trp23Stop and Trp66Gly mutations in the LDL receptor gene: common causes of familial hypercholesterolemia in Denmark. Atherosclerosis 1996; 120: 57–65.
Carmena-Ramón R, Ascaso JF, Real JT, Ordovás JM, Carmena R : Genetic variation at the apo A IV gene locus and response to diet in familial hypercolesterolemia. Arterioscler Thromb Vasc Biol 1998; 18: 1266–1274.
Pimstone SN, Sun XM, du Souich C, Frohlich JJ, Hayden MR, Soutar AK : Phenotypic variation in hetrozygous familial hypercholesterolemia. A comparison of Chinese patients with the same or similar mutations in the LDL receptor gene in China or Canada. Arterioscler Thromb Vasc Biol 1998; 18: 309–315.
Leitersdorf E, Eisenberg E, Eliav O et al: Genetic determinants of responsiveness to HMG-CoA reductase inhibitor fluvastatin in patients with molecularly defined heterozygous familial hypercholesterolemia. Circulation 1993; 87: 35–44.
Sijbrands EJG, Lombardi MP, Westendorp RGJ et al: Similar response to simvastatin in patients heterozigous for familial hypercholesterolemia with mRNA negative and mRNA positive mutations. Atherosclerosis 1998; 136: 247–254.
Mamo JCL, Smith D, Yu KC et al: Accumulation of chylomicron remnants in homozygous subjects with familial hypercholesterolemia. Eur J Clin Invest 1998; 28: 379–384.
Castro MC, De Bruin TWA, Westerveld HE, Meijer E, Erkelens DW : Delayed chylomicron remnants clearance in subjects with heterozygous familial hypercholesterolemia. J Internal Med 1998; 244: 299–307.
März W, Ruzicka V, Phol T, Usadel KH, Gross W : Familial defective apolipoprotein B-100: mild hypercholesterolemia without atherosclerosis in a homozygous patient. Lancet 1992; 340: 1362.
Gallagher JJ, Myant NB : Variable expression of the mutation in familial defective apolipoprotein B-100. Arterioscler Thromb 1993; 13: 973–976.
Schaefer JR, Scharngl H, Baumstark MW et al: Homozygous familial defective apolipoprotein B 100. Enhaced removal of apolipoprotein E containing VLDLs and decreased production of LDLs. Arterioscler Thromb Vasc Biol 1997; 17: 348–353.
Jansen ACM, van Wissen S, Defesche JC, Kastelein JJP : Phenotypic variability in familial hypercholesterolemia: an update. Curr Opin Lipidol 2002; 13: 165–171.
Acknowledgements
We thank the patients and their relatives for their cooperation. This work was supported by grants from Fondo de Investigaciones Sanitarias and Generalitat Valenciana to JT Real (FIS 02/1875 and GV01-46) and Red de Centros Metabolismo y Nutrición del Instituto Carlos III (C 03/08).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Real, J., Chaves, F., Ejarque, I. et al. Influence of LDL receptor gene mutations and the R3500Q mutation of the apoB gene on lipoprotein phenotype of familial hypercholesterolemic patients from a South European population. Eur J Hum Genet 11, 959–965 (2003). https://doi.org/10.1038/sj.ejhg.5201079
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201079



