Key Points
-
Check all 10-year-olds for the position of their permanent canines by initial clinical examination and palpation, if necessary with further radiographs to locate possible impactions
-
Check for late eruption of permanent incisors, if one incisor has erupted, the others should not be far behind. If the permanent lateral incisors have erupted but not the permanent central incisors then suspicion of impaction should be heightened
-
Refer too early rather than too late
Key Points
Orthodontics
-
1
Who needs orthodontics?
-
2
Patient assessment and examination I
-
3
Patient assessment and examination II
-
4
Treatment planning
-
5
Appliance choices
-
6
Risks in orthodontic treatment
-
7
Fact and fantasy in orthodontics
-
8
Extractions in orthodontics
-
9
Anchorage control and distal movement
-
10
Impacted teeth
-
11
Orthodontic tooth movement
-
12
Combined orthodontic treatment
Abstract
This section deals with the important issue of impacted teeth. Impacted canines in Class I uncrowded cases can be improved by removal of the deciduous canines. There is some evidence that this is true for both buccal and palatal impactions. Treatment of impacted canines is lengthy and potentially hazardous. Interceptive measures are effective and preferred to active treatment. Supernumerary teeth may also cause impaction of permanent incisors, their early diagnosis and appropriate treatment is essential to optimise final outcomes. If there are any doubts about impacted teeth it is better to refer too early than too late, this latter option may unnecessarily extend the length of treatment as well as the treatment required.
Similar content being viewed by others
Main
This section brings together the information general dental practitioners need in order to diagnose and deal effectively with impacted teeth.
Impacted canines
A canine that is prevented from erupting into a normal position, either by bone, tooth or fibrous tissue, can be described as impacted. Impacted maxillary canines are seen in about 3% of the population. The majority of impacted canines are palatal (85%), the remaining 15% are usually buccal. There is sex bias, 70% occur in females. One of the biggest dangers is that they can cause resorption of the roots of the lateral or central incisors and this is seen in about 12% of the cases.
The cause of impaction is not known, but these teeth develop at the orbital rims and have a long path of eruption before they find their way into the line of the arch. Consequently in crowded cases there may be insufficient room for them in the arch and they may be deflected. It seems that the root of the lateral incisor is important in the guidance of upper permanent canines to their final position. There is also some evidence that there may be genetic input into the aetiology of the impaction.
Late referral or misdiagnosis of impacted canines places a significant burden on the patient in relation to how much treatment they will subsequently need. If the canines are in poor positions it will require a considerable amount of treatment and effort in order to get them into the line of the arch and a judgement must be made as to whether it is worth it. Sacrificing the canine is unsatisfactory since this presents a challenge to the restorative dentist, an aesthetic problem and by definition, cannot be used to guide the occlusion. There are times when it might be sensible to consider its loss, but early diagnosis can make a significant difference to how much treatment is needed by the patient.
Diagnosis
It is easy to miss non-eruption of the permanent canines, but there are some markers which should increase suspicion of possible impaction. Any case with a deep bite, missing lateral incisors or peg-shaped upper lateral incisors needs a detailed examination. Figure 1 shows such a case and in this instance both canines were significantly impacted on the palatal aspect. The retained deciduous canine is self evident. Other clues include root and crown positions. Figure 2 shows a lateral incisor which is proclined. There is a retained deciduous canine and the permanent canine lies buccal which moves the root of the lateral incisor palatally and the crown labially.
Any general dental examination of a patient from the age of 10 years should include palpation for the permanent canine on the buccal aspect. It is possible to locate the canines with palpation, but this will lead to some false observations. For instance, the buccal root of a decidous canine, if it is not resorbing, can feel like the crown of the permanent tooth. It is therefore important to back up clinical examination with radiographs. Failure to make these observations will eventually result in patients complaining of loose incisors; inevitably some permanent canines will resorb adjacent teeth with devastating efficiency as shown in Figures 3 and 4.
The patient shown in Figure 3 had both lateral incisors removed because of the severe root resorption caused by the unerupted permanent canines
What are the best radiographic views to locate canines?
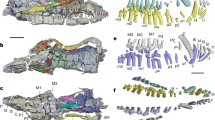
Most patients undergoing routine orthodontic screening will have a dental pantomogram. Location of tooth position requires two radiographs in different positions. In the interests of radiation hygiene it is sensible to use this as a base x-ray and to take further location radiographs in relation to the dental pantomogram. An anterior occlusal radiograph allows this and the principle of vertical parallax can be used to locate the position of the canine. The tube has to shift in order to take an anterior occlusal and it moves in a vertical direction. If the tooth crown appears to move in the direction of the tube shift (ie vertically) then the tooth will be positioned on the palatal aspect. If the crown appears to move in the opposite direction it is buccal and if it shows no movement at all it is in the line of the arch (Figures 5,6,7). This also provides a reasonably detailed intra-oral view in cases of root resorption.
Although there are other radiographic techniques which can be used to locate canines, this method works well. If there are difficulties in being sure of the exact location then two periapicals taken of the region with a horizontal shift of the tube may give slightly better precision. The periapical radiographs will also give good detail of the roots of adjacent teeth, particularly the lateral incisors. The proximity of the canine crown to incisor roots does make them vulnerable to root resorption. The percentage of teeth adjacent to the crown of the canine which undergo some form of resorption is probably quite high at the microscopic level. No extractions should be contemplated until the canines have been located. Figure 8 shows a dental pantomogram of a patient who had both upper and lower first premolars removed as part of a treatment plan, but where the canines had not been located beforehand. The dental pantomogram clearly shows the poor position of the canines and subsequent treatment involved the removal of the permanent canines since their position was deemed hopeless and movement of the canines may well have resulted in root resorption of the incisors. The canines had to be replaced prosthetically and it would be difficult to see how a legal defence of this situation could be raised.
Interceptive measures for canines
One of the most significant publications in the orthodontic literature came from Ericson & Kurol (1988)1 who demonstrated that extraction of upper deciduous canines where the upper permanent canines were developing on the palatal aspect, resulted in nearly an 80% chance of correcting the impaction. The paper was very specific about what types of malocclusions this could be applied to. Nearly all the cases were Class I with no incisor crowding. This is important to emphasise, a subsequent follow-up paper2 confirmed their original observation and also indicated that the technique could not be applied easily to crowded cases and in some cases this would result in a worsening of the situation rather than an improvement. The dental pantomogram of a patient is shown in Figure 9. The canines are palatally positioned. Since this was an uncrowded case, the deciduous canines were extracted and Figure 10 shows that both the permanent canines erupted with no orthodontic assistance. Clearly this saved the patient a considerable amount of treatment and early appropriate referral would be wise if a general dental practitioner is unsure. The interceptive measure of extracting deciduous canines works well if carried out between the ages of 11–13 years. The closer the crowns are to the mid-line the worse the prognosis. It is worth re-emphasising that this works best in Class I uncrowded cases.
Treatment of canines
The treatment of buccally or palatally impacted canines involves exposure and then a form of traction to pull the tooth into the correct position in the arch. Palatally impacted teeth can be exposed and allowed to erupt. This tends to form a better gingival attachment since the tooth is erupting into attached mucosa. This cuff may be lost on the palatal aspect as the tooth is brought into line. Some operators prefer to raise a flap, attach a bracket pad with a gold chain to the tooth in theatre and then replace the flap. Traction is subsequently applied to the chain and the tooth pulled through the mucosa (Fig. 11). There is some evidence that this procedure is less successful than a straight forward exposure. It also has a disadvantage that if the bonded attachment fails then a further operation, either to expose or reattach, is needed. The advantage with this technique is that the root usually needs less buccal torque once the crown is in position.
If the canine is moderately high and buccal, it will not be possible to expose the tooth since it will then erupt through unattached mucosa and an apically repositioned flap should be considered. If it is very high, it is not possible to apically reposition the flap and therefore it is better in this situation to raise a flap and bond an attachment with a gold chain. It is critical that the chain passes underneath the attached mucosa and exits in the space where the permanent canine will eventually be placed as in Figure 11. If it is not placed in this situation and exits out of non-keratinised mucosa the final gingival attachment will be poor (Fig. 12).
Other options include:
Accept and observe
Leaving the deciduous canine in place and either observing the impacted canine or removing it. Long term, the deciduous canine will need prosthetic replacement.
Extract the impacted canine
If there is a good contact between the lateral incisor and the first premolar then it has to be carefully considered whether this should be accepted. The purists of occlusion will argue that the premolar is not capable of providing good canine guidance. Aesthetically there are problems since the palatal cusp hangs down. This can be disguised by grinding or rotating the tooth orthodontically so that the palatal cusp is positioned more distally. The placement of a veneer on the premolar is another way of improving the appearance.
Transplantation
Canine transplantation has received poor press in the past. Many of the problems arose because the canines were transplanted with a closed apex. These teeth were seldom followed up with root fillings on the basis that they would revascularise. This is unlikely through a closed apex and it is preferable to treat them as if they were non-vital. Transplantation is an option which should only be reserved for teeth that are in almost an impossible position and where there is extensive hypodontia or other tooth loss.
Implants
Implants are also an option and as single tooth implants improve, this may become more favoured in future. It is important to remember that implants in a growing child will ankylose and appear to submerge as the alveolus continues to develop. These are not therefore an option until the patient is at least 20 years of age.
Correction of canine position
Favourable indications for correction of impacted canines.
Canines are moved most easily into their correct position if the root apex is in a favourable position. If the tooth lies horizontally it is extremely difficult to correct this and generally the closer the tooth to the midline the more difficult the correction will be. Treatment is nearly always lengthy and can damage adjacent teeth. Figure 13 shows a lateral incisor adjacent to a palatally impacted canine where the opposite reaction to pulling the palatal canine out is the labial positioning of the lateral incisor root. Obviously this is not favourable and the gingival recession will worsen. The force to move the canines can be obtained from elastomeric chain or thread. Figure 14 shows elastomeric chain being used to pull the canine labially. An attachment has been bonded to the tooth, but as the tooth moves to its correct position it will be necessary to rebond it. Moving the tooth over the bite sometimes requires the occlusion to be disengaged with a bite plane or glass ionomer cement build ups on posterior teeth, for a few weeks.
When the canine is pulled labially the reaction will be for the lateral root to move labially. It is essential therefore to use thick rectangular wires during the movement of palatally positioned canines. Further labial movement of the lateral root would be potentially damaging to the periodontal attachment
An alternative is to use a smaller diameter nickel titanium 'piggy back' wire with a stiff base wire to align the tooth (Fig. 15). The thicker base wire maintains the archform by resisting local distortion caused by the traction on the canine. The nickel titanium piggy back wire produces flexibility and a constant low force, unlike elastomeric chain or thread which have a high initial force and then a rapid decay of this force. It is better not to tie the piggy back in fully as the wire needs to be able to slide distally as the canine moves labially. If tied in fully the friction does not allow this function. It also helps if the piggy back wires run through auxiliary tubes on the first molar bands. One further method which has gained some popularity is the use of a sectional archwire made of beta-titanium alloy. This wire is formable and flexible, it can be deflected as a sectional arm and pulls the canine labially. It is important to use a palatal arch which cross braces the molars to prevent them moving into crossbite as an opposite force reaction to the buccal movement of the canines (Fig. 16).
The use of heat activated nickel titanium alloys has also done much to improve the efficiency of moving impacted canines into the correct position. Figures 17 and 18 show a sequence of tooth movements where a nickel titanium alloy has been deflected, after cooling with a refrigerant, into the bracket. The length of time between the two slides was 8 weeks and it can be seen how much tooth movement has occurred. The transpalatal arch is also useful anchorage for vertical and antero-posterior tooth movements.
Same patient as shown in Figure 17 nearly 8 weeks later where significant tooth movement has taken place
What can go wrong?
There are a number of problems with moving permanent canines from either a buccal or a palatal position. By and large, the older the patient the less chance there is of succeeding, and certainly moving canines in adults requires caution. If the canines have to be moved a considerable distance then ankylosis is a distinct possibility as well as loss of vascular supply and therefore pulp death. Treatment often takes in excess of 2 years and it is important to maintain a motivated and co-operative patient. It is necessary to create sufficient space for the canine to be aligned and this is usually around 9 mm.
The periodontal condition of canines that have been moved into the correct position in the arch can deteriorate, this is particularly true if care has not been taken to ensure that the canine either erupts or is positioned into keratinised mucosa. There may also be damage to adjacent teeth during surgery, or indeed the surgeons can damage the canine itself with burs or other instruments. Figure 19 shows the crown of a canine which has clearly been grooved by a bur which was used for bone removal when the canine was exposed. It is quite easy to induce root resorption of adjacent teeth (either the lateral incisor or the first premolar), particularly if care is not taken in the direction of traction applied to the impacted canine. Loss of blood supply of adjacent teeth can also occur. It is quite common at the end of treatment to see a slightly darker crown of the permanent canine, this probably results from either a change in vascularity and vitality of the canines, or potentially haemoglobin products can be produced and seep into the dentine thus changing the colour of the overlying enamel. The worst scenario of all is that the canine ankyloses and will not move. The protracted length of treatment also results in patients abandoning treatment.
Despite all of our improvements in treatment mechanics and diagnosis for impacted canines, the eruption path is often unpredictable. Canines which have a seemingly hopeless prognosis can sometimes correct their position and erupt. Nevertheless, to sit and observe a patient where the canines are clearly in difficulty without referral to a specialist would be difficult to defend legally. Hopefully the days of patients arriving in orthodontic departments with retained deciduous teeth at the age of 16 will diminish as the profession takes on the challenge of life long learning.
Other impacted teeth
The most common cause of unerupted maxillary incisors is the presence of a supernumerary tooth. These are often typed as follows:
-
Conical
-
Tuberculate
-
Odontomes (complex or compound)
-
Supplemental teeth
There are some conditions which have a genetic basis where impacted teeth are seen more frequently and this includes cleidocranial dysplasia, cleft lip and palate, gingival fibromatosis and Down's Syndrome.
It is worth remembering that most central incisors should have erupted by the age of 7 and lateral incisors by the age of 8. Surprisingly, most referrals for impacted maxillary incisors are when the patient is 9 years of age. This delay in diagnosis could potentially influence the outcome and it is important that when the contralateral incisor has erupted 6 months previously there is likely to be a problem. Similarly, if the lateral incisors erupt well before the central incisor then consideration should be given to investigating further (Fig. 20).
It is perfectly possible that a supernumerary tooth may be present and not affect the eruption of the incisors (Fig. 21). Indeed one of the clinical signs that a supernumerary may be present is the evidence of spacing where a supernumerary is in the midline and causing a diastema between the upper incisors. The different types of supernumerary teeth seem to have different implications for treatment.
Conical supernumerary teeth are small and peg-shaped, they usually have a root and they do not often affect incisor eruption (Fig. 21), but if they are in the midline they can cause a median diastema. They should only be removed if they are adjacent to incisors which need to undergo root movement. Potentially the movement of the root against the supernumerary tooth could cause resorption of an incisor root.
Where the supernumerary teeth are tuberculate these usually have no roots and develop palatally. They often prevent the eruption of central incisors and if they do, they need to be removed (Fig. 22). Complex and compound odontomes are rare, but can similarly prevent eruption of the permanent incisors and also need to be removed. Obviously, radiographs are needed to confirm any clinical observations about impacted teeth and parallax used in the same way as for canines in order to locate the position of the supernumerary teeth. Eighty per cent of supernumerary teeth occur in the anterior part of the maxilla and there is a male to female ratio of 2:1. The incidence in the population as a whole varies, but is somewhere in the region of 1–2%.
Treatment of impacted supernumeraries
Although guidelines have been published from the Royal College of Surgeons,3 these review what the options are rather than defining what the best treatment is. In part this is due to a lack of good research to show what the best methods are.
Obviously if there is an obstruction the sooner it is removed the better. Some suggest exposing the incisor at the same time or attachment of a gold chain in order to prevent re-operation if the tooth fails to erupt. However, this is potentially damaging, particularly if bone has to be removed in order to expose or bond an attachment to the tooth with a gold chain brought out through the mucosa in order to place traction and move the impacted incisor.
If diagnosed early and the supernumerary is removed when the apex of the incisor is open then eruption of the tooth can be anticipated. Even if there is a need to re-operate at a later date, if the tooth has come further down it is much easier to either expose the tooth or raise a flap and place an attachment on an incisal edge that is now much closer to its correct position. Often incisors will erupt quite a long way and then become impacted in fibrous tissue (Fig. 23). In this situation it only requires a small exposure usually on the palatal aspect to allow the tooth to come down. Apically repositioned flaps are often disastrous and produce poor mucosal attachment. In the main they should be avoided.
Fixed appliances are usually needed in order to regain lost space where adjacent teeth have drifted and these appliances are also useful if traction does need to be applied to the impacted teeth. Removable appliances in this situation are often cumbersome, although they have been used with a magnet bonded to the unerupted tooth and a further magnet embedded into the removable appliance in order to bring the tooth down. The use of fixed appliances in this situation allows alignment, space management and overbite correction. Ultimately the early diagnosis of unerupted teeth is the biggest contribution a practitioner can make to the management of impacted teeth.
Impacted premolars
Where crowding exists or where there has been early loss of deciduous molars, premolars are sometimes unable to erupt. Often relief of crowding (usually extraction of first premolars) allows impacted second premolars to erupt. Second premolars do seem to have enormous potential to erupt and given time these teeth often find their way into the arch (Figs 24 and 25). Often in the upper arch they displace palatally. There may also be clues from the deciduous teeth. If the deciduous teeth become ankylosed they often appear to submerge as alveolar bone growth continues. This may indicate the absence of a second premolar, but sometimes this submergence can be seen when permanent successors are present. Most of these situations will resolve, but it is thought wise to consider removing the second deciduous molar if it slips below the contact points and there is then space loss as the molar tips forward. Where first molar mesial migration compromises the contact point relationship, space maintenance might be considered. Figure 26 shows a radiograph of a patient who appears to have generalised submergence since all second deciduous molars are seen to be submerging in all four quadrants. In this situation continued observation of the development of the occlusion with appropriate loss of deciduous molars is essential. With the extensive restorations and caries, an argument could be made for loss of all four first molars in this case.
Other impactions
The only other impactions to be considered in a general form are first molars. These may impact in soft tissue and it is sometimes worth considering occlusal exposure where a first molar has not erupted. This usually occurs in the upper arch and can be accepted if the oral hygiene is good with minimal caries experience. Impacted molars of this type quite frequently self correct before or during eruption of the second premolar. There may also be primary failure of eruption and if the tooth fails to move with orthodontic traction this is usually a good indication that the tooth will not move. First molars may also impact into second deciduous molars as they erupt and the options then are to try and move the molar distally with a headgear or removable appliance, to consider using separators (brass wire) to relieve the impaction or ultimately to remove the second deciduous molar if any of these methods fail to relieve the impaction.
It is clear that the biggest single contribution that can be made to the treatment of impacted teeth is to improve diagnostic skills and define care pathways with clinical protocols. Early referral does not harm, a late referral will increase the burden of care for patients and practitioners.
References
Ericson S, Kurol J . Early treatment of palatally erupting maxillary canines by extraction of the primary canine. Eur J Orthod 1988; 10: 283–295.
Power S, Short MBE . An investigation into the response of palatally displaced canines to the removal of deciduous canines and an assessment of factors contributing to favourable eruption. Br J Orthod 1993; 20: 215–223.
National Clinical Guidelines. Faculty of Dental Surgery, Royal College of Surgeons of England, 1997.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Roberts-Harry, D., Sandy, J. Orthodontics. Part 10: Impacted teeth. Br Dent J 196, 319–327 (2004). https://doi.org/10.1038/sj.bdj.4811074
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4811074
This article is cited by
-
Comprehensive characterization of epidemiological and 3D radiographic features of non-third molar impacted teeth in a Chinese dental population
Clinical Oral Investigations (2022)