Key Points
-
Renal patients may have impaired drug excretion. Drugs used in dental sedation and general anaesthesia should be used with caution and in consultation with a physician.
-
Renal disease influences the use of other drugs in dentistry, particularly NSAIDS and some antimicrobials
-
Platelet dysfunction may occur in renal patients giving rise to a bleeding tendency. Patients on haemodialysis may be heparinised. Dental treatment should be carried out on the day after dialysis. Renal condition is optimal at this time and the anticoagulant effect has stopped.
-
The arm with vascular access for dialysis (the surgically created arterio-venous fistula) should not be used for venepuncture by the dentist.
-
Patients who have had a kidney transplant may need corticosteroid cover, have a bleeding tendency if anticoagulated, may have gingival hyperplasia if taking ciclosporin and are prone to infection due to immunosuppression.
Key Points
General medicine and surgery for dental practitioners:
-
1
Cardiovascular system
-
2
Respiratory system
-
3
Gastrointestinal system
-
4
Neurological disorders
-
5
Liver disease
-
6
The endocrine system
-
7
Renal disorders
-
8
Musculoskeletal system
-
9
Haematology and patients with bleeding problems
-
10
The paediatric patient
Abstract
Patients with kidney disorders are increasingly encountered in dental practice due to improvements in medical care leading to prolonged life expectancy. In order to provide appropriate and safe dental care for these patients it is important to have a working knowledge of renal disorders and related problems.
Similar content being viewed by others
Points in the History
The principal renal condition that the dental practitioner is likely to encounter is chronic renal failure. Occasionally, patients with nephrotic syndrome are seen (see later). It is not uncommon to encounter patients who have undergone a renal transplant.
It is worth bearing in mind that there is significant potential for renal problems in diabetic patients. Diabetic nephropathy is the most common cause of end-stage renal failure (ESRF) in developing countries and accounts for 14% of those patients affected in the UK. It is unlikely that the dentist would be the first to diagnose diabetes mellitus, but suspicion should be raised in patients who show a changing profile of dental disease such as newly presenting or rapidly progressive periodontal disease. Further questioning may elicit that the patient feels the need to drink plenty of fluids and appears susceptible to infections including dental abscesses and fungal conditions.1,2
Chronic renal failure (CRF) occurs after progressive kidney damage and constitutes a low glomerular filtration rate persisting over a period of 3 months or more. The symptoms and signs vary depending on the degree of malfunction. In early CRF the patient may notice a need to urinate frequently at night (nocturia) or may notice an uncharacteristically poor appetite. Adult CRF leads to hypertension and uraemia (a clinical and biochemical syndrome constituting end-stage renal disease). CRF can affect diverse body systems and these are summarised in Table 1. This can have wide ranging implications on patient management.3
Bone disease or 'renal osteodystrophy' is an almost universal feature of CRF and may take one or a combination of forms. As a result of an increase in plasma phosphate levels, there is a consequent suppression of plasma calcium resulting in an elevated parathormone (PTH) level. Calcium metabolism is further compromised by disruption in vitamin D metabolism. There is a failure in conversion of 25-hydroxycholecalciferol to the active form 1, 25 di-hydroxycholecalciferol. This results in secondary hyperparathyroidism. Hyperparathyroidism is discussed in more detail in the endocrine paper in this series. Many patients have been taking steroids, either to combat renal disease or to avoid transplant rejection. Steroids are well known to produce osteoporosis after prolonged use and this may become evident following a renal transplant.
Renal disease almost invariably causes an anaemia. This occurs mainly due to failure of production of erythropoietin (EPO) by the kidney. Renal loss of red blood cells, marrow fibrosis and increased red cell fragility with subsequent early destruction also contribute. The anaemia may result in tiredness and decreased concentration. Shortage of breath and palpitations due to decreased oxygen carriage and increased cardiac output may also occur. Marrow fibrosis leads to a reduced platelet count and poor platelet function. Patients may give a history of taking recombinant EPO, having multiple transfusions and taking iron supplements.
Renal dialysis The timing of dental treatment must be co-ordinated with dialysis. Treatment should be performed on the non dialysis days
It is worth asking which type of dialysis a patient undergoes and when the last session was since patients are best treated when they have recently dialysed. Haemodialysis may be carried out in the body (peritoneal) or outside (extra-corporeal). Both types rely on the patient's blood being exposed to a solution hypotonic in metabolites across a semi-permeable membrane. Extra-corporeal dialysis relies upon a high flow of blood from the patient to the dialysis machine and then back to the patient. The dialysis team produce a peripheral arterio-venous fistula for regular large vessel diameter access (Fig. 1). It is of vital importance that the fistula is well-maintained and not used for any other purpose. Accidental damage to the area can result in torrential haemorrhage. Peritoneal dialysis uses the patient's own peritoneal membrane as the semi-permeable barrier. The dialysing fluid is instilled into the peritoneal cavity, left in-situ and drained as effluent. Infection of the peritoneal catheter is a major potential complication leading to peritonitis. It is important to consider the use of prophylactic antibiotics for any dental procedure that may cause a bacteraemia. Dialysis itself still carries a risk of infection (HIV, hepatitis, bacterial) and this should be borne in mind.
Haemostasis is impaired to varying degrees in patients with CRF and enquiry regarding any bleeding tendency should be made. The main factors involved are impaired platelet adhesiveness, decreased von Willebrand's factor and decreased thromboxane. Prostacyclin levels are raised leading to vasodilatation. The bleeding time is often prolonged. In addition, patients who are being dialysed will be heparinised during dialysis. However, as the effects of heparin are not prolonged, treatment performed on a day when the patient is not being dialysed presents no problem with drug-induced anti-coagulation.
Infections tend to be poorly controlled in a patient with CRF and patients post-kidney transplant are immunosuppressed to prevent rejection. Signs of infection tend to be masked, particularly in patients taking steroids, and therefore care needs to be taken to treat odontogenic infections promptly and effectively. Transplant patients have an overall mortality of less than 5% and steroids will be used as part of the immunosuppression as well as other agents, usually ciclosporin. Antibiotic cover should be considered for at least two years post transplant. Patients may give a history of oral candidosis or oral viral infections eg herpes simplex, cytomegalovirus and Epstein-Barr virus (EBV). There is an increased chance of malignancy due to immunosuppression and these may range from lymphomas to cutaneous cancers eg basal cell (Fig. 2) and squamous cell cancers.
The nephrotic syndrome is found in some patients. This comprises proteinuria, hypoalbuminaemia, oedema and hyperlipidaemia. Causes include diabetes mellitus and systemic lupus erythematosus. An increase in the level of circulating factor VIII leads to hypercoagulability and the possibility of thromboses. As a result such patients may give a history of taking prophylactic heparin. A patient with nephrotic syndrome may also be taking corticosteroids and using a low salt and high protein diet. Prophylactic antibiotics may be given for procedures likely to cause a bacteraemia. There is an increased likelihood of atheroma in these patients.
Kidney stones are of little relevance to dental practice, except for the fact that they may be associated with hyperparathyroidism. A summary of salient points to be obtained in the history is given in Table 2.
Examination of the dental patient with renal disease
Oedema may occur as a result of sodium retention and may be evident both at the ankles and around the face. Periorbital oedema is often seen and the patient may exhibit the characteristic 'moon face' of steroid therapy. The fluid retention may lead to pulmonary oedema, pleural and cardiac effusions which may present as shortage of breath and an inability to lie flat during dental treatment. Bone pain may result from a disruption of vitamin D metabolism.
The incidence of oral ulceration is increased in these patients and the oral mucosa may be pale secondary to anaemia but this sign is often rather subjective. As mentioned previously dental infections may become widespread very rapidly and oral candidosis may be present. Herpes simplex, zoster, cytomegalovirus, EBV and toxoplasmosis are increased in incidence and prophylactic aciclovir may be used.
Gingival hyperplasia occurs with ciclosporin therapy.4 It is also associated with an increased and rapid build up of calculus. The hyperplasia often reduces with improved oral hygiene involving scaling and polishing.
As previously mentioned, there is an increased incidence in disorders which can be related to immunosuppression including lymphoma, skin cancers (Fig. 2), hairy leukoplakia, leukoplakia and Kaposi's Sarcoma.5
Patients undergoing dialysis may experience swelling of the major salivary glands (especially the parotid glands). Salivary flow may be decreased in CRF leading to increased oral problems.6 Palatal and buccal keratosis is sometimes seen. The conditions tend to resolve with established dialysis or transplant. The tongue may be dry and coated. Periodontal disease may be evident and there may be bleeding from the gingival margins. In children, CRF leads to decreased growth and sometimes delayed tooth eruption and enamel hypoplasia. A summary of clinical features which may be encountered in CRF is shown in Table 1.
The patient may have an arterio-venous fistula at the wrist or in the antecubital fossa (Fig. 1). High blood flow through the fistula leads to a palpable vibration or thrill when the examiner's fingers are placed lightly on the skin over the area of the fistula. As mentioned earlier, this arm should not be used for routine venepuncture or IV sedation.
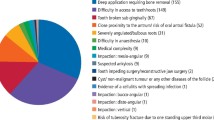
Dental management of patients with renal disorders (Table 3)
It is important to appreciate the problems faced by a patient with chronic renal disease and anticipate their reduced resistance to infection as well as their concurrent disease. Antibiotic prophylaxis should be considered for dental procedures likely to produce a bacteraemia. Routine dental care requires little modification but it is obvious from the above that oral hygiene is important. Standard procedures should be employed to prevent cross-infection. Infiltration analgesia is not contraindicated but any bleeding tendency should be excluded prior to administering a nerve block.
Most patients are best treated under local anaesthesia due to the anaemia and potential electrolyte disturbances which would complicate GA. Corticosteroids are often prescribed for these patients and thus a steroid boost may be required for surgical procedures (see respiratory paper in this series). These patients are often hypertensive and this should be considered prior to any form of treatment. It is important to ensure good haemostasis after oral surgical procedures because of this and the bleeding tendency. Patients are best treated the day after dialysis as platelet function will be optimal and the effect of the heparin will have worn off. Consultation with the renal physician is advised. Desmospressin (DDAVP) has been used to assist with haemostasis in cases of prolonged bleeding.
Intra-oral manifestations Renal disease may cause oral ulceration, candidosis, gingival hyperplasia and dysplastic lesions in the mouth
Renal disease progresses at a varying rate ranging from subclinical loss of renal reserve to renal insufficiency culminating in ESRF. Loss of reserve may not manifest itself unless the kidneys are placed under stress. This can happen after the administration of certain drugs, a heavy dietary protein load or pregnancy. Swallowed blood acts as a protein load and may occur, for example, from a post-extraction haemorrhage. Dietary manipulation is useful in decreasing sodium and potassium load and a low protein diet reduces the need to excrete nitrogenous metabolites.
The patient's cardiovascular status should be considered since these patients are predisposed to arrhythmias due to electrolyte disturbances and the incidence of atheroma is increased in patients with nephrotic syndrome, as stated earlier. Congestive cardiac failure may ensue and such patients are best treated sitting up to minimise pulmonary oedema and avoidance of placing the legs in a dependent position, again to minimise oedema.
Impaired drug excretion leads to the need for care with drug prescriptions and is discussed in the next section.
Prescribing for patients with renal disease.
Renal disease influences the use of drugs in dentistry. Many drugs prescribed by dentists are excreted by the kidney.7 Failure to excrete a drug or its metabolites may lead to toxicity. As a general rule any drug that is nephrotoxic (such as gentamicin which may be used in prophylaxis against endocarditis) should be avoided. Other drugs may require dose reduction. Erythromycin is contraindicated in patients who have had a kidney transplant and are taking ciclosporin. Ciclosporin metabolism is reduced leading to an increase in toxicity.8
Drugs contained in the Dental Practitioners Formulary whose dose should be reduced in the presence of significant kidney disease include the antimicrobials aciclovir, amoxicillin, ampicillin, cefalexin and erythromycin. Tetracyclines other than doxicycline should be avoided. Non-steroidal analgesics should not be prescribed in those with more than mild renal impairment, paracetamol being the drug of choice for post-operative pain control. Drugs used in dental sedation should be used with extreme care as a greater effect than normal may be produced.
Conclusion
Renal disease impacts on dental management. The timing of treatment may be affected in patients with serious renal impairment. Co-operation with the physician is necessary in such patients.
References
Harrison GA, Schultz TA, Schaberg SJ . Deep neck infection complicated by diabetes mellitus. Report of a case. Oral Surg Oral Med Oral Path 1983; 55: 133–137.
Ueta E, Osaki T, Yoneda K, Yamamoto T . Prevalence of diabetes mellitus in odontogenic infections and oral candidiasis: an analysis of neutrophil suppression. J Oral Path Oral Med 1993; 22: 168–174.
De Rossi SS, Glick M . Dental considerations for the patient with renal disease receiving haemodialysis. J Am Dent Assoc 1996; 127: 211–219.
Seymour RA, Jacobs DJ . Cyclosporin and the gingival tissues. J Clin Perio 1992; 19: 1–11.
Seymour RA, Thomason JM, Nolan A . Oral lesions in organ transplant patients. J Oral Path Oral Med 1997; 26: 297–304.
Kao CH, Hsieh JF, Tsai SC, Ho YJ, Chang HR . Decreased salivary function in patients with end-stage renal disease requiring haemodialysis. Am J Kidney Diseases 2000; 36: 1110–1114.
Seymour RA, Meechan JG, Walton JG . Adverse Drug Reactions in Dentistry. 2nd ed. pp 169–175. Oxford: Oxford University Press, 1996.
Jensen CWB, Flechner SM, Van Buren CT, Frazier OH, Cooley DA, Lorber MI, Kahan BD . Exacerbation of ciclosporin toxicity by concomitant administration of erythromycin. Transplantation 1987; 43: 263–270.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Greenwood, M., Meechan, J. & Bryant, D. General medicine and surgery for dental practitioners Part 7: Renal disorders. Br Dent J 195, 181–184 (2003). https://doi.org/10.1038/sj.bdj.4810434
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4810434
This article is cited by
-
Evaluation of UK paediatric nephrology teams’ understanding, experience and perceptions of oral health outcomes and accessibility to dental care: a mixed-methods study
Pediatric Nephrology (2024)
-
General medicine and surgery for dental practitioners. Part 1 – the older patient
British Dental Journal (2010)
-
Oral and salivary changes in patients with end stage renal disease (ESRD): a two year follow-up study
British Dental Journal (2007)