Key Points
-
The Siqveland matrix is by far the most popular in general dental practice in Scotland.
-
Most dental practitioners do not remove and change the matrix band between patients, relying on routine instrument decontamination procedures.
-
Time, cost and lack of perception of need were the main barriers identified to changing bands between patients.
-
Most dentists who reponded had provided their dental nurses with training in cleaning and sterilisation of instruments.
-
Hand-scrubbing remains a component of instrument cleaning protocols in many dental surgeries, but ultrasonic baths were used by 59% of practitioners.
Abstract
Aims The aims of this study were to determine the pattern of use and re-use of matrix bands in general practice in Scotland, to demonstrate which type of matrix band is most commonly used and to examine infection control measures of relevance to the safe use and re-use of matrix bands.
Materials and methods Subjects: 621 of Scotland's 1,849 general dental practitioners were randomly selected. Data collection: A 19-item self-reported questionnaire was mailed in June 1999 with a follow-up mailing sent in August 1999. Analysis: Data analysis involved descriptive statistics and cross-tabulation. Where appropriate, differences between categories were tested for significance by a Chi-square test.
Results A total of 479 questionnaires were returned, representing a response rate of 77%. Reported compliance with routine glove wearing was high (91%). Most dentists (92%) provided training on instrument cleaning and sterilisation for their dental nurses. Ultrasonic baths were used by 59% of practitioners; the remainder soaked or manually scrubbed instruments to remove debris before autoclaving. The Siqveland matrix was the matrix of choice for 96% of respondents. 7% provided a new matrix band for each patient. Most (64%) changed bands only when they were bent or damaged; 29% changed them daily or weekly. Deterrents to use of a new band for each patient were cost (39%) and time (52%). A total of 54% of respondents considered matrix band replacement unnecessary between patients.
Conclusions The Siqveland matrix band is the most popular among the study group of dental practitioners. Re-use of matrix bands is common. Guidelines for the safe re-use of matrix bands are required.
Similar content being viewed by others
Main
The emergence of human immunodeficiency virus (HIV) in the 1980s provided a catalyst for significant improvements in cross infection control in dental practice. As a result of increased public concern and professional awareness, official guidelines from statutory bodies and advice from associated organisations have led to standardisation of infection control procedures for all patients, now termed Universal Precautions.1 All practitioners have an ethical, legal and professional obligation to implement effective infection control procedures within their practices. In order to achieve this, all instruments contaminated with oral and other body fluids must be sterilised after use. The surfaces of the items to be sterilised must be exposed to the sterilising agent for a sufficient length of time to ensure destruction or denaturation of all micro-organisms. Any factor that interferes with this exposure will prevent effective sterilisation.2 It is therefore essential that all surface debris be removed prior to sterilisation.
One item of dental equipment which has received little attention in this context is the matrix band. The ideal matrix should be simple to insert and remove; cause minimal trauma to hard and soft tissues during placement; allow establishment of correct restoration contour; be sufficiently rigid during restoration placement to allow condensation of restorative material; show good compatibility with restorative materials; be non-toxic to soft tissues; allow use in conjunction with rubber dam; be economical and finally, be sterilisable. A wide variety of types are available. In the UK, the Siqveland is commonly used, but others include the Tofflemire matrix, sectional matrices, and the recently introduced Omni-matrix, the latter offering a fully disposable alternative to the more traditional matrix systems, but at a higher unit cost.
The previous literature on matrix bands has focused on selection criteria and placement technique.3,4,5,6 To date there have been no studies to evaluate the extent of matrix band re-use and the methods used for their cleaning and sterilisation. The aims of this investigation were to determine the degree of re-use of matrix bands in general dental practice in Scotland, to determine the type of matrix system that is most commonly used and finally, to examine general infection control measures relevant to safe use and re-use of matrix bands.
Materials and methods
Study group selection
Advice was sought from a statistician to determine sample size and selection methods. Each Scottish Health Board provided a list of dental practitioners holding a current general dental services contract. The study sample for this investigation was chosen using a systematic random sampling method, stratified by the health board. The final sample size was 621 dentists.
Questionnaire
A 19-item self-reported questionnaire was designed using selected principles of Dilman's total design method.7 Questions were divided into three subsections. The first assessed demographics to determine the sample population characteristics. The second section inquired after relevant general cross infection control procedures, training and methods of cleaning and sterilisation. The final section evaluated the use of matrix systems and approaches to their re-use and replacement. A brief pilot study involving six dental practitioners was carried out in order to assess any difficulty with response or ambiguity of questions. Constructive suggestions were incorporated into the final version of the questionnaire.
Practitioners were allocated a coding to aid identification of responses and thus facilitate follow-up mailing to those who did not respond initially. During June 1999, the questionnaire, a covering letter and a stamped addressed envelope were mailed to each sample individual. Each letter was addressed personally and signed, with participants being advised of the importance of practice-based research to support their clinical decisions. Replies were collected over a 10-week period during June–August 1999. A duplicate questionnaire printed on a different coloured paper, and a modified covering letter were posted to those who failed to respond within this period. Coding was deleted from this arm of the study to enhance anonymity and encourage response. This second batch of replies was collected over a further 8-week period.
Data handling and statistical analysis
Data collected were entered into a Microsoft Access database and replies were assigned a new identification number. A sample of twenty randomly selected questionnaires was re-checked to verify accuracy of data entry. Data were analysed using Minitab version 11. Statistical analyses were undertaken of group I (response within 10 weeks of initial mailing), follow-up group II (response during follow up data collection period) and overall responses in an attempt to detect any late response bias. Data analysis involved descriptive statistics and cross tabulation. With regard to behaviour, differences between categories were tested for significance using a Chi-square test of association, combining categories where necessary.
Results
Demographic data
A total of 479 questionnaires were returned, representing a response rate of 77%. During the initial ten-week data collection period, 391 replies were received with a further 88 during the follow up exercise. Practitioners from the early and late responding groups did not demonstrate any differences with regard to demographic characteristics. As a result of the design of this survey, it was not possible to identify practitioners who failed to respond and thus no estimation could be made of non-response bias.
Of responding practitioners, 73% were male. The mean interval since graduation was 17 (range 1–43) years, but over two thirds of responding dentists had been qualified for less than 20 years. Over 80% of respondents operated within a group or partnership. A total of 62% were practice principals with a further 37% practising under associateship agreements. The majority of the dentists (85%) were practising within city centre or suburban areas. Despite selecting practitioners with an active NHS contract number, it was apparent that the commitment to provision of NHS treatment varied. Of the respondents, 65% were providing care within the NHS, a further 30% combined NHS and private treatment, while 5% provided mainly private care.
This questionnaire did not record details of specific courses attended, but attendance at meetings may indicate a general willingness to maintain levels of knowledge. Within the preceding 12 months, only 42 respondents (9%) stated that they had not attended any courses, whilst 33% had attended one to two courses and the remainder had attended three or more courses.
General infection control measures
The wearing of gloves and facemasks were used as measures of compliance with established infection control measures. The early and late responding clinicians exhibited no significant difference in their use of personal protective equipment. In total, 91% of respondents in this study reported wearing gloves for all procedures, with only two respondents stating that they never wore gloves. There was no difference in prevalence of glove wearing between those dentists providing private treatment or those working within the NHS. Associate dentists demonstrated a significantly higher level of compliance (97%) compared with principals (87%) (p<0.001), while a similar trend was observed between group practitioners (93%) and single-handed practitioners (82%) (p=0.003). The incidence of reported glove wearing was significantly higher in the younger practitioners, with 93% of those qualified 20 years or less using gloves for all patients compared with 85% of those qualified for more than 20 years (p=0.004). Mask use for all patients was reported by 53% of dentists, with similar trends towards higher rates of usage in younger associates in group practices.
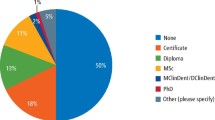
A total of 92% of respondents provided their dental nurses with formal training in the cleaning and sterilisation of instruments after use. The distribution of the mode of training is shown in Table 1. Fifty four per cent of dentists were personally involved in training procedures, with dedicated dental nurse training courses being used by 76%, although in the late responding group, training outside the practice was less popular. Seven practitioners indicated that specialist equipment manufacturers or suppliers provided additional training.
The distribution of the cleaning procedures for contaminated instruments is shown in Table 2. Both combined and one-stage methods were reported. Ultrasonic baths were used by 59% of practitioners, with the remainder soaking or scrubbing instruments to remove debris. No respondents used a clinical dishwasher. Although over 99% of respondents used a steam autoclave to sterilise instruments, 30 (6%) indicated that dry heat or disinfection were used in addition. However no details of the types of instruments concerned or circumstances of use were recorded.
Matrix band systems
The Siqveland system was recorded as the matrix band of choice for posterior restorations by 96% of respondents (Table 3). For 2% of respondents the Tofflemire matrix was the primary choice and was used on occasions by a further 8%, whilst both sectional and disposable systems were used by five respondents (1%).
In relation to frequency of changing bands, only 7% provided a new band for each patient. The majority of respondents (64%) changed bands only when they were bent or damaged, with the remaining 29% changing them at daily or weekly intervals (Table 4). Major factors cited by respondents which deterred the use of a new band for each patient were cost (39%) and time (52%). A total of 54% of practitioners in this study considered it to be unnecessary to replace bands after each use and 60% would not consider using a disposable system in the future.
Discussion
In this investigation the sampling frame comprised the Scottish Health Boards lists of general dental practitioners with an active NHS contract number. The survey sample of 621 dentists represented one third of Scotland's 1,849 general dental service clinicians.8 Of the 29,951 practitioners registered with the General Dental Council, 70% are male, with a comparable percentage of male respondents (73%) in this investigation.
The mailed questionnaire method is frequently used to gather data from medical and dental clinicians and their patients. Questionnaire surveys have the advantage of reduced cost and time input, and are sufficiently simple for individuals to implement without the need to involve research organisations.7 The major disadvantage is often cited as the poor response rate. However, Dilman, in his total design method7 has suggested many factors that may positively influence response rate, some of which were used in the design of the current questionnaire. According to Mangione,9 the response rate of 77% obtained in the present study would be classified as very good, helping to reduce the effects of a non-response error.
During the investigation of sensitive issues such as implementation of infection control procedures, reported responses may differ from the true underlying behaviour trends. The professional desirability of certain actions may encourage practitioners to provide the perceived ideal response. Data relating to the compliance with recommendations may be flawed in this way, yet there is no satisfactory ethical mechanism to verify self-reported data.10 Nevertheless, by comparison with previous studies, it is encouraging to note a progressive increase in reported levels of compliance with guidelines issued by national advisory bodies. For example, routine glove wearing among dental practitioners has increased from 75% in 1990-9111 to 86% in 199312 to 96% in the current investigation performed during 1999.
Placement of matrix bands is a common procedure in restorative practice with approximately six million Class II amalgam restorations being placed in England and Wales in the year to March 2000.13 It is clear from the present study that an overwhelming majority of dental practitioners use the Siqveland matrix system. In the light of the regular blood contamination of these items and the fact that they frequently pass into gingival tissues during placement, it is perhaps surprising that so little attention has been paid to matrix bands as a potential route for transmission of blood-borne pathogens. The results of this investigation show that only a small proportion of the responding practitioners change matrix bands after each patient, most relying on their routine instrument cleaning and sterilisation procedures to render the assembled band and retainer safe for re-use. This is an acceptable practice if the cleaning of the item, prior to sterilisation, can be guaranteed. However, a recent study14 has demonstrated that the complex surface topography of Siqveland matrix bands can render cleaning of the assembled device difficult and unreliable. If Siqveland matrix bands are used, then practitioners should give serious consideration to changing the bands between patients. Alternatively, a disposable matrix system can be used.
Clearly, such a change in practice would, for many, have time and cost implications, both of which were cited as barriers to matrix band changing between patients. Even more importantly, more than half of the respondents did not believe it to be necessary to replace bands between patients. This is understandable, since there is little in the way of official guidance. Evidence for the difficulties in providing adequate cleaning of assembled Siqveland matrix bands14 may help in the formulation of appropriate guidelines in this area and result either in design changes which favour effective cleaning and sterilisation or in changes to working patterns.
References
BDA Advisory Service Advice Sheet A12. Infection control in dentistry. London: British Dental Association 2000.
Block SS Disinfection, Sterilisation and Preservation Philadelphia: Lea & Febiger 1991.
Cunningham PJ Matrices for amalgam restorations. Aust Dent J 1968; 13: 139–142.
Kaplan I, Schuman N Selecting a matrix for a Class II amalgam restoration. J Prosthet Dent 1986; 56: 25–31.
Meyer A Proposed criteria for matrices. J Can Dent Assoc 1987; 1: 851–853.
Qualtrough AJE, Wilson NHF Matrices, their development and in clinical practice. Dental Update 1992; 19: 281–286.
Dilman DA Mail and telephone surveys: The total design method New York: Wiley 1978.
Scottish Dental Practice Board (SDPB) Annual Report 1998–1999.
Mangione TW The basics of avoiding non-response error. London: Sage Publications 1995.
Gordon BL, Burke FJT, Bagg J, Marlborough HS, McHugh S Systematic review of dental team's adherence to infection control guideline. J Dent Res 2000; 79: 570.
Hudson-Davies SCM, Jones JH, Sarll DW Cross infection control in general dental practice: dentist's behaviour compared with their knowledge and opinions. Br Dent J 1995; 178: 365–369.
Bentley EM, Sarll DW Improvements in cross infection control in general dental practice. Br Dent J 1995; 179: 19–20.
Dental Practice Board (DPB). Digest of statistics 2000 Dental Practice Board, Eastbourne 2000.
Lowe AH, Bagg J, Burke FJT, MacKenzie D, McHugh S A study of blood contamination of Siqveland matrix bands. Br Dent J 2002; 192: 43–45.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Lowe, A., Burke, F., McHugh, S. et al. A survey of the use of matrix bands and their decontamination in general dental practice. Br Dent J 192, 40–42 (2002). https://doi.org/10.1038/sj.bdj.4801286
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4801286
This article is cited by
-
An in vitro study on the use of circumferential matrix bands in the placement of Class II amalgam restorations
British Dental Journal (2008)
-
Cleanability of dental instruments – implications of residual protein and risks from Creutzfeldt-Jakob disease
British Dental Journal (2007)
-
An investigation of the decontamination of Siqveland matrix bands
British Dental Journal (2007)
-
A study of blood contamination of Siqveland matrix bands
British Dental Journal (2002)