Abstract
Objective To provide a critical review of the current evidence that links dental treatment to infective endocarditis (IE) and appraise the risks of antibiotic chemoprophylaxis.
Design Retrospective analysis
Setting Mainly hospital based patients or subjects
Outcome measures The interrelationship between infective endocarditis and dental treatment is complex and in many instances uncertain. The risk from antibiotic chemoprophylaxis appear greater than the risk of contracting IE.
Results There is increasing evidence that spontaneous bacteraemia are more likely to cause IE in at risk patients than specific episodes of dental treatment. Antibiotic chemoprophylaxis may not necessarily reduce dental-induced bacteraemia and the protective effect if any from antibiotic cover may arise from an inhibitory action upon bacterial colonisation on the compromised cardiac valves.
Conclusion There is increasing concern over the misuse of antibiotics in general and this has focused attention on chemoprophylaxis in dentistry to prevent IE. New evidence on dental-induced bacteraemia and the prevalence of IE in association with dental treatment raises further questions on the need to provide antibiotic cover in at risk patients. More prescriptive guidelines to define who is at risk from IE and what procedures require cover will help to reduce overprescribing of antibiotics and reduce the risks of their unwanted effects.
Similar content being viewed by others
Main
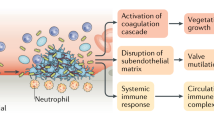
Infective endocarditis (IE) is a microbial infection of the endocardial surfaces usually involving the cardiac valves. The condition is relatively uncommon with a prevalence of 11–50 cases per million population per year.1 Figures for England and Wales show that approximately 1500 cases of IE occur per year.2 It is interesting to note that the prevalence of IE has remained consistent even after the introduction of antibiotic 'prophylaxis' in the 1940's.3 Whilst figures from the UK are between 14–20 years old, the more recent epidemiological studies confirm4,5,6 the prevalence of this disease. This could imply that antibiotic prophylaxis is ineffective or not directed towards the appropriate 'at risk' population.
Dental procedures, especially those that result in a bacteraemia, are frequently blamed for IE, hence the need for antibiotic prophylaxis to cover such procedures in at risk patients. This has been the clinical doctrine and teaching for the past 50 years. Recent evidence from the USA4 and studies from the Netherlands5,6 have presented further data which challenges the practice of prescribing antibiotics before dental procedures to prevent endocarditis. This information also needs to be considered in tandem with the increasing concern over the unnecessary use of antibiotics. Thus, it seems pertinent to reassess the topic of antibiotic prophylaxis, dental treatment and infective endocarditis.
Dental-induced bacteraemia
General dental practitioners often express concerns as to what dental procedures produce bacteraemia and who is at risk from such bacteraemia. Poor oral health, especially periodontal status, is an important risk factor for IE. Gingival inflammation correlates positively with the prevalence and magnitude of bacteraemia.7 However, bleeding per se is a poor predictor of odontogenic bacteraemia.8
Certain dental procedures are associated with bacteraemia, although the magnitude will vary. The prevalence of such bacteraemia and the associated procedures is shown in Table 1.
Also, by contrast are the prevalence of bacteraemia arising after various oral hygiene practices and after chewing. In many instances their magnitudes are comparable with the listed dental procedures. It has been suggested that oral hygiene practices and chewing are responsible for so-called random cases of bacteraemia. Such bacteraemia either from dental treatment or oral hygiene practices etc. are of a low grade intensity (1↔101 – 2↔102 ctu/ml of blood) and of short duration.9
Dentists and dental treatment are often regarded as the culprit for IE. In many instances the occurrence of endocarditis does not relate to the so-called dental-induced bacteraemia. It may well transpire that random bacteraemia may be more causative in IE than dental surgeons carrying out treatment. This view is supported in a recent review article8 which has evaluated the evidence of dental-induced bacteraemia and IE. The three main conclusions are as follows: bleeding is a poor predictor of dental-induced bacteraemia; the intensity of bacterial inoculae arising from dental operative procedures is low when compared to the high intensity needed for ID90 in experimental animals: the procedures most often regarded as requiring antibiotic prophylaxis do not carry the greatest risk of cumulative bacteraemia. The latter arise from chewing and various oral hygiene practices.
Further evidence to support this finding comes from an analysis of cases of IE where dental treatment has been implicated as the cause. Oral streptococci cause approximately 50% of all IE cases.10 Similarly, only 15% of patients where IE has been diagnosed report medical or dental treatment within the previous 3 months.11 It has been estimated that 4% or less of all IE cases are related to dental treatment-induced bacteraemia.3,7 Whether such bacteraemia arise from dental treatment or were spontaneous is not discernible. Oakley (1987)2 suggested that if spontaneous random bacteraemia cause 96 % of all cases of IE, then these bacteraemia as opposed to those arising from dental treatment may also have caused the remaining 4 %.
There is considerable debate as to whether endodontic procedures result in significant bacteraemia and be the cause of IE. The controversies surrounding endodontics are discussed below.
Endodontics
Most pulp and periapical disease is caused by microbial infection.12,13,14 Operative procedures for its management range from simple pulp capping, through conservative root canal treatment to emergency drainage and surgical endodontics. In practice, any of these interventions and their adjuncts including local anaesthetic administration and rubber dam placement involving infected tissues are capable of inducing bacteraemia and placing patients at risk of infective endocarditis. Review of the available evidence suggests that this is not so and that many endodontic manipulations, especially those confined to the pulp canal system, are relatively low risk. Several researchers have shown that bacteraemia does not occur15,16,17,18 or is an uncommon and short-lived event19,20,21 following pulpotomy or root canal preparation short of root-end. But many of these older studies15,16,17,19 should be interpreted with caution due to the crude sampling, transport and culture methods employed. Contemporary studies employing rigorous microbiological techniques20,21 have yielded more positive blood cultures, and even the application of rubber dam was recently shown in children to produce bacteraemia of comparable magnitude to a dental extraction.22 Highly sensitive, molecular methods have yet to be applied in the identification and sourcing of cultivable and non-cultivable microbes in the circulation after careful endodontic treatment. It is likely that a wide variety of organisms would be detected, though their significance with respect to infective endocarditis is not known. By contrast, even with crude methods, bacteraemia may occur in one third to one half of cases after deliberate and repeated instrumentation beyond the root apex.16,17,18,21 It may appear that endodontics as a risk factor for IE depends upon the nature of instrumentation, including the deliberate or inadvertent extension of instruments beyond the root end. A review of legal evidence has revealed that in 13% of cases of IE there is a recent episode of endodontic treatment prior to the onset of the disease (Martin 1997). More invasive, surgical endodontic procedures with flap retraction and periapical curettage are associated predictably with a very high prevalence of bacteraemia.23
Perhaps based on the evidence of older, flawed studies, recent American Heart Association guidelines24 recommend that antimicrobial prophylaxis is not required for:
-
Non-intraligamentary local anaesthesia
-
Placement of rubber dams
-
Intracanal endodontic treatment; post placement and build-up.
Prophylaxis is specifically recommended for:
-
Root canal instrumentation or surgery beyond the apex
-
Incision and drainage and other procedures involving infected tissues
The latter may imply that prophylaxis should be considered for manipulation of the acutely abscessed tooth, even if efforts are made to confine instrumentation within the tooth,25 although there is currently no evidence to suggest that drainage through teeth in this way presents any increased risk.
Microorganisms probably enter the circulation more commonly during endodontic treatment than the current body of scientific literature would suggest. What is not clear is whether such events place dental patients at significant risk of infective endocarditis, and if the risks of antimicrobial prophylaxis outweigh the possible benefits on an individual or community level. It is certainly the consensus within the American guidelines that responsible clinicians should think carefully before covering endodontic procedures in known at-risk patients.
As in other circumstances, it is the responsibility of clinicians to minimise risks, and on that basis, it is likely that local measures contribute as much as antimicrobial drug therapy to endocarditis prophylaxis in endodontics.26 Patients should be encouraged to use a chlorhexidine mouthrinse prior to local anaesthetic injection and rubber dam placement, and the operative site should be routinely sanitised by effective rubber dam isolation and the use of an antimicrobial irrigant.
Confining instrumentation to the root canal is notoriously difficult due to the unpredictability of root-end topography, and difficulties of radiographic working-length determination.27,28 Operators should err on the cautious side during working length determination in at risk patients, and consider the use of a contemporary electronic apex locator to confirm length at intervals during the preparation to avoid inadvertent over-instrumentation.29,30 Crown down approaches (that is removing the coronal pulp first and proceeding incrementally to the apex) to canal preparation may also reduce microbial extension and the prevalence of bacteraemia, though this has yet to be proved clinically.
Antibiotic prophylaxis and the at risk patients
In spite of the uncertainty surrounding the relationship between dental treatment and IE, it is still recognised clinical practice to provide antibiotic prophylaxis for 'at risk patients'. Guidelines for such prophylaxis are published on a regular basis and those applicable to the UK are shown in Table 2. Some countries follow the UK guidelines, whilst others follow those recommended by the American Heart Association (Table 3). There are some obvious differences between the two guidelines. The American guidelines have categorised patients as high, moderate and negligible risk, whilst those from the BSAC have identified 'special risk patients'. The AHA have also defined further the problems of mitral valve prolapse as a risk factor for IE. Procedures that require cover are listed by the AHA (Table 4) whereas the BSAC recommend cover for scaling (supra and subgingival), extractions, oral and dental surgery.
Differences also exist between the AHA and BSAC guidelines with respect to antibiotic regimens. Irrespective of the patient's status or procedure to be undertaken, the AHA recommend an oral dose of amoxycillin 2g or clindamycin 600mg if the patient is allergic to penicillin. No follow-up doses are required.
Efficacy of antibiotic prophylaxis in the prevention of IE
It is standard clinical practice to provide antibiotic prophylaxis for patients at risk from IE before undergoing certain dental procedures. Guidelines followed are those recommended by the BSAC57and these are based upon the current evidence to date to support efficacy of such prophylaxis in the prevention of IE.
However, the efficacy of antibiotic prophylaxis to prevent this disease has not been subjected to a randomised, placebo-controlled study. Such a study would require at least 6000 at risk patients31and would probably encounter strong ethical concerns. Evidence to date on the efficacy of antibiotic prophylaxis has come from case-controlled studies, animal experiments and antibiotic efficacy studies on bacteraemia after tooth extractions. There is uncertainty as to whether prophylactic administration of penicillins has an impact on orally-induced bacteraemia. Parenteral penicillin has been shown to reduce bacteraemia by 84–86% at 5 minutes and 95–97% at 30 minutes after a bacteraemic induction. These figures compare with a reduction of 24–42% and 49–76% respectively when no prophylaxis is used.32 By contrast other workers have shown that penicillin 2 g and amoxycillin 3 g fails to prevent bacteraemis after dental extractions.33 There is now a growing consensus that antibiotic prophylaxis may not prevent IE by a bactericidal blood activity but may do so by decreasing microbial adherence to damaged cardiac valves or by eliminating bacteria after their attachment to valves.34,35,36
Although most attention has focused on antibiotic prophylaxis there is evidence that antiseptic mouthwashes (i.e. chlorhexidine and povidone-iodine) used prior to certain dental procedures may reduce the prevalence and severity of bacteraemias.37,38 The American Heart Association recommend use of local irrigation with chlorhexidine before treatment that can result in a bacteraemia. Whether such a procedure is sufficient to prevent infective endocarditis in either high or moderate risk patients has yet to be determined. One possible disadvantage is that regular use of chlorhexidine may lead to the selection of resistant streptococci such as Strep sanguis39 and other gram-negative bacteria. An endocarditis from such resistant organisms would have a higher mortality rate than one caused by viridans streptococci.40
Compliance with antibiotic prophylaxis regimens
Compliance with antibiotic prophylaxis regimens does seem to be a problem world wide, irrespective of the recommendation. Figures for compliance range from 15–35%. In such instances compliance relates to using the recommended antibiotic dose, identifying the 'at risk patient' and providing cover for the appropriate dental procedure.
A UK study has evaluated the cost effectiveness of prophylaxis in dental practice to prevent IE.41 Their survey estimated that in England and Wales approximately 27 million high risk dental procedures are carried out per year. Of these, 5% of the patients will have cardiac valvular lesions, most of which will be mitral valve prolapse. Extrapolation of the figures reveals that 1.35 million high risk procedures will be undertaken on at risk patients each year. It is estimated that half of these patients will receive the appropriate antibiotic prophylaxis.42 Thus 670,000 at risk patients will be undergoing high risk dental procedures in the absence of prophylaxis. This figure becomes meaningful when compared to 2410, which is the number of cases of IE that occurs in the UK each year (1500 cases from England and Wales, plus 910 from Scotland and Northern Ireland). Many of these cases will be of non-dental origin. This data does challenge the relationship between high risk dental procedures and the prevalence of IE together with the efficacy of antibiotic prophylaxis.
Possible risks associated with antibiotic prophylaxis
When antibiotics are given prophylactically to prevent IE, the clinician needs to consider the risk and cost benefit of such treatment. The most significant adverse event associated with the penicillins is hypersensitivity reactions. These can range from a troublesome rash to a life threatening anaphylactic reactions. One-to-ten per cent of patients report a penicillin allergy43 although many of these will not be confirmed if subjected to the appropriate test. More importantly, the chance of a penicillin reaction following administration of the drug is in the range of 0.7–5 %.44 This prevalence does vary with the route of drug administration, with the intramuscular route causing a 5 % prevalence and oral penicillin a 0.3 %. However, high doses of oral amoxycillin can cause an allergic rate similar to intramuscular penicillin.45
Data from the USA show that 400–800 deaths are caused each year by anaphylactic reactions to the penicillins, although only a proportion of these will arise from penicillin prophylaxis to prevent IE. To put the risk-benefit into perspective, it has been estimated that 1.36 people per million population are likely to die from penicillin anaphylaxis to prevent IE, whereas only 0.26 deaths per million population are due to dental procedure-induced endocarditis.46 Put another way, patients receiving penicillin (amoxycillin) prophylaxis to prevent IE are 5 times more likely to die from an anaphylactic reaction to the drug than to die from contracting endocarditis.
A further unwanted effect from regular use of antibiotic prophylaxis is the development of resistant strains. The World Health Organisation has recognised antimicrobial resistance as a global problem.47 Approximately one third of all antibiotics are prescribed for prophylactic purposes and a high proportion of these are for prevention of IE.48 The continued and repeated use of prophylactic antibiotics has caused selection of antimicrobial resistance in oral streptococci.49 Overprescribing of antimicrobials has made some antibiotic regimens less effective.50 There is also recent evidence that overprescribing by dental practitioners for prophylactic purposes is high and knowledge of the cardiac conditions which may predispose to infective endocarditis is poor. The prevalence of resistant oral streptococci in patients susceptible to infective endocarditis has only been estimated in one trial. About one third of all streptococci isolated were found to have minimum infective concentrations which were high and would be normally classed as resistant.49 The mechanism whereby antimicrobial prophylaxis prevents infective endocarditis is however probably dependent on a number of factors independent of resistance mechanisms.
Recent evidence on the need for prophylaxis
In a recent editorial,51 four papers were reviewed which called into question the need for pre-dental treatment antibiotic prophylaxis7,52,53,54 and three recent major studies that investigated the link between dental procedures and IE4,5,6 were examined.
The first paper reviewed 18 paediatric patients with infective (bacterial) endocarditis for failure of chemoprophylaxis and found none had had a previous dental procedure.7 This concurred with the reportedly low prevalence of extractions preceding infective endocarditis (3.6 %) and was put in the context of the relative rates of bacteraemia reported for mastication and dental sepsis without intervention (38 % and 11 % respectively). In the second study of case-control design, a substantially higher risk of endocarditis was calculated in patients with mitral valve prolapse (MVP) as diagnosed on echocardiography. MVP is a condition 'quite common' in the population (but not apparent in the asymptomatic) and not therefore subjected to chemoprophylaxis. The third study was based on reported cases of infective endocarditis in patients with mitral valve prolapse and a survey of leading authorities on bacterial endocarditis.53 It concluded that no prophylaxis or prophylaxis with erythromycin appeared preferable to prophylaxis with penicillin. This was based on 10 million patients with mitral valve prolapse, and the cases of fatal and non-fatal endocarditis and deaths from drug reactions (47,2 and 0 with no prophylaxis, 12,1 and 0 with erythromycin and 5,0 and 175 with penicillin). The fourth paper concluded that 'the general impression that dentist-induced bacteraemia are responsible for the vast majority of infective endocarditis cases is erroneous, for these bacteraemia may cause as little as 4% or less of all infective endocarditis'.54
Of the three recent studies cited in the Editorial,51 one was a case study and the remaining two were of case-control design. In the first,5 a prospective study was undertaken of all hospitalised cases of bacterial endocarditis. Out of 427 patients with late prosthetic or native valve endocarditis, 275 were eligible for antibiotic prophylaxis (197 because of a known cardiac lesion, 78 a prosthetic heart valve). Out of the eligible 275 patients, 64 (23.3 %) had undergone a prophylaxis-indicating procedure within 180 days of onset; 17 (26 %) of them had antibiotic prophylaxis. In 31 (11.3 %), the procedure had been within 30 days of onset; 8 (26 %) had antibiotic prophylaxis. The authors found that 'For an incubation of 180 days, full compliance with prophylaxis might have prevented endocarditis in 47 (17%) patients with late prosthetic or native valve endocarditis involving a previously known cardiac lesion who underwent a procedure with an indication for prophylaxis'. The comparable figure for 30-day incubation was 23 (8.4%), or 5% of all patients with endocarditis (472). In the same year, the Dutch group published the second cited study of 438 patients diagnosed with endocarditis over a two year period.6 Of these, 48 were eligible as cases because they had had a medical or dental procedure for which chemoprophylaxis was indicated within 180 days. Out of 889 cases eligible 200 controls were identified comprising patients with the same cardiac status who did not develop endocarditis after the same challenge. One in six patients in both groups had received chemoprophylaxis. The best estimate of protective efficacy was 49% for first-ever endocarditis occurring within 30 days of a procedure. Finally, a recent study of community-acquired endocarditis4 found that dental treatment was no more frequent among cases than controls (adjusted odds ratio 0.8) and that among cases with known cardiac lesions (the target of prophylaxis) dental therapy was significantly less common than among controls; and few participants received chemoprophylaxis. The authors concluded that the lack of a link between dental treatment and IE, together with the rare occurrence of this disease does not justify the routine use of antibiotic prophylaxis.
Criticisms of the cited papers
That two of the cited studies are of a case-control design is important. Whilst case-alone studies can demonstrate a risk, the addition of controls allows risk to be quantified. However, case-control studies are not first rate in hierarchies of evidence which reflect the degree to which different study designs are susceptible to bias, or how certain it is that the observed effects are attributable to the intervention and are not the result of other factors (Table 5). Close scrutiny of the cited case control studies shows even these have weaknesses (Table 6).
For example, the van der Meer study,5 cases were inpatients diagnosed with endocarditis, controls non-endocarditis medical/cardiology outpatients matched for age, sex and cardiac defect. Cases were interview face-to-face, controls by telephone (though pre-warned by letter including disclosure of the nature of the study). There may have been a recall bias in that patients with endocarditis might unwittingly rationalise dental treatment as the cause of their demise, whereas in telephone-interviewed controls that connection would not necessarily be considered.
In the study by Strom and colleagues,4 cases were hospital endocarditis patients, controls community residents matched for age, sex and neighbourhood. Cases had been examined recently because of their endocarditis status, controls not. Here, under-reporting of dental interventions by controls may have compounded any discrepancies in cardiac status to introduce a bias.
In their study, they conclude, 'only a few cases of infective endocarditis could be prevented by antibiotic prophylaxis for dental treatment even if 100 % effectiveness were assumed.' Even though they could not demonstrate a difference between cases and controls in relation to dental treatment and endocarditis status, they showed that 38.8 % of cases were infected with dental flora. Although this last point is not thought to be relevant by the authors, a small but statistically-insignificant association between dental extraction and endocarditis was noted. In view of the small numbers involved (six cases of endocarditis with an extraction history, no controls), the authors speculate that this might be a chance finding.
One other case control study has been reported, similar in design to that of van der Meer et al.55 Even though recall bias might be less of a problem (as face-to-face interviews were conducted), the study showed a small increased risk of endocarditis in relation to scaling and root canal treatment but not extraction. A small proportion of cases and controls had received appropriate chemoprophylaxis.
Other criticisms of the cited studies have been aired. For example, following the publication of one of the studies cited by Durack in his editorial.6 Simmonds et al. published a critical letter in the Lancet.56 They raised three points. The first was that, although the number of cases of endocarditis prevented was negligible in population terms, the effect on individual patients could not be ignored. Secondly, they were concerned at the small numbers of cases eventually entered into the trial, and the even smaller number who received adequate prophylaxis. Finally, they doubted the feasibility of mounting a sufficiently large trial to settle this question, and commented that it might be fruitless anyway. For these reasons, they did not see good reason to waiver current antibiotic prophylaxis practice for dental patients, and did so with some authority (having considered the issue inside the Working Party of the British Society for Antimicrobial Chemotherapy.)57
The same criticisms could be raised with the other two papers cited in Durack's editorial. The earlier van der Meer paper5 reports a small but important relationship between medical and dental procedures and subsequent endocarditis (23 % of people eligible for chemoprophylaxis having undergone such a procedure 180 days before onset). In addition, because there were no controls in this study, it is possible that the association between dental procedures and endocarditis may have been underestimated.
To summarise the arguments thus far: Four recent studies of endocarditis patients either fail to show a dental connection with infective endocarditis, or can only show a small one, although the study designs are low in the hierarchy of validity and can be criticised. Other contributors to the debate add that the dangers of chemoprophylaxis outweigh the dangers of endocarditis, and that chemoprophylaxis is poorly implemented even when at-risk patients are identified, which we now know is not as often as we had thought. So from a population perspective, the current regimens for antibiotic prophylaxis might be flawed. If the cost-benefit relationship is in doubt, then there is a case for undertaking a randomised controlled trial to settle the issue. Such a trial would have to be extensive given the apparent relative rarity of dentally-induced endocarditis.
Yet that is the dilemma. Few are prepared to say that dental treatment causes no endocarditis; and even advocates of less prophylaxis demonstrate that some endocarditis follows dental treatment. So it might be impossible to devise a trial in which some individuals would be denied chemoprophylaxis. In the mean time, clinicians and their patients will find it difficult to abandon chemoprophylaxis whilst circumstantial evidence exists, on an individual level, it confers some benefit (or more precisely, may reduce a theoretical risk). It would be a brave clinician indeed who would deny chemoprophylaxis to an at-risk patient in the face of a published study of 53 cases of endocarditis that were the subject of legal claims on the basis that their condition was caused by dental treatment and/or inadequate antibiotic cover.58 It might be difficult to change clinical practice even if an unequivocal randomised control trial was done. Until such a trial can be completed, current regimens are likely to remain in place, even if subject to review and modification.
Conclusions
In this paper, we have attempted to review the evidence that implicates bacteraemia arising from dental treatment to IE. We have also considered the risk/benefits associated with antibiotic prophylaxis used to prevent this condition. Certainly, there is increasing evidence that dental treatment-induced bacteraemia are no longer the culprit regarded previously. Oral streptococcal-induced infective endocarditis can only be linked to dentistry if there is a defined risk procedure, no prophylaxis is given and the incubation period is short (i.e. less than 14 days between dental treatment and onset of symptoms). Indeed, there is evidence to suggest that spontaneous bacteraemia are more likely to be the cause of IE in at risk individuals. If this is the case, then the use of antibiotic prophylaxis needs to be reconsidered and a greater emphasis placed on improving oral health in at risk patients.
The efficacy of antibiotic prophylaxis to prevent IE has never been evaluated in a randomised controlled study (RCT), and the profession has hedged away from such investigation on the grounds of numbers of patients required and ethical considerations. Perhaps the time has come for this issue to be addressed. A staged approach could be useful – that is targeting a specific cardiac condition (i.e. mitral valve prolapse) and an operative dental procedure with low risk (i.e. supragingival scaling or endodontics). In view of the numbers involved, a multi-centre approach will be required, but at least an RCT on such a population would confirm whether cover was required and also evaluate the risk/benefits of the antibiotics administered.
Concern has also been expressed over the misuse of antibiotics and inappropriate prescribing for prophylactic purposes. Other agents used topically (i.e. chlorhexidine) may reduce dental-induced bacteraemia and produce fewer significant adverse events. If spontaneous bacteraemia are the main cause of IE, then their prevalence and severity should be reduced by attending to oral hygiene practice and periodontal diseases.
The debate over the association between dental procedures and IE will continue, but the recent case-controlled studies and the review of dental-induced bacteraemia have certainly stimulated argument. The spectre of litigation does cloud judgement in this area and it is this which probably leads dentists to err on the side of caution and prescribe antibiotics to cover the patient whilst undergoing treatment. This paper has probably contributed further to this dilemma. The British Society for Antimicrobial Chemotherapy (BSAC) is the body that recommends the various antibiotic regimens which are carried out in clinical dentistry. It is anticipated that the new findings on the relationship between dental treatment and IE will be evaluated by the BSAC when they reconsider their guidelines. There is certainly a need for further research in this area since the dental team still need to know who is at risk from IE, what procedures require cover, and are patients at greater risk from receiving chemoprophylaxis than not?
References
Young S E J . Aetiology and epidemiology of infective endocarditis in England and Wales.. J Antimicrob Chemotherap 1987; 20 (Suppl A): 7–14.
Oakley C M . Controversies in the prophylaxis of infective endocarditis: a cardiological view.. J Antimicrob Chemotherap 1987; 20 (Suppl A): 99–104.
Bayliss R, Clark C, Oakley C. et al. The teeth and infective endocarditis. Br Heart J 1983; 50: 506–512.
Strom B L, Abrutyn E, Berlin J A, Kinman J L, Feldman R S, Stolley P D. et. al., Dental and cardiac risk factors for infective endocarditis. A population-based, case-control study. Ann of Int Med 1998; 729:: 761–9.
Van der Meer J T, Thompson J, Valkenburg H A, Michel M F . Epidemiology of bacterial endocarditis in The Netherlands. II. Antecedent procedures and use of prophylaxis.. Arch of Int Med 1992; 152: 1869–73.
Van der Meer J T, Van Wijik Wm Thompson J, Vandenbroucke J P, Vafkenburg H A, Michel M F . Efficacy of antibiotic prophylaxis for prevented native-valve endocarditis. Lancet 1992; 339: 135–9.
Guntheroth W G . How important are dental procedures as a cause of infective endocarditis. Am J of Cardiol 1984; 54: 797–801.
Roberts G . Dentists are innocent! "Everyday" bacteremia is the real culprit: A review and assessment of the evidence that dental surgical procedures are a principal cause of bacterial endocarditis in children. Pediatr Cardiol 1999; 20: 317–325.
Roberts G J, Gardner P, Simmons N A . Optimum time for detection of dental bacteraemia in children. Int J Cardiol 1992; 35: 311–315.
Kaye D . Prophylaxis for infective endocarditis: an update. Ann Intern Med 1986; 104: 419–423.
Cherubin C E, Neu H C . Infective endocarditis at the Presbyterian Hospital in New York City from 1938-1967. Am J Med 1971; 51: 83–96.
Sundqvist G . Bacteriological studies of necrotic pulps (Odontological Dissertation No.7). Umea 1976; University of Umea, Sweden.
Kakehashi S, Stanley H R, Fitzgerald R . The effects of surgical exposures of pulps in germfree and conventional laboratory rats. Oral Surg Oral Med Oral Path 1965; 20: 340–344.
Moller A J R, Fabricuis L, Dahlen G, Ohman A E, Heyden G . Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J of Dent Res 1981; 89: 475–484.
Beechin I, Laston D J, Garbarino V E . Transitory bacteraemia as related to the operation of vital pulpotomy. Oral Surg Oral Med Oral Path 1956; 9: 902–905.
Bender I B, Seltzer S, Yermish M . The prevalence of bacteraemia in endodontic manipulation. Oral Surg Oral Med Oral Path 1960; 13: 353–60.
Bender I B, Seltzer S, Tashman S, Melof G . Dental procedures in patients with rheumatic heart disease. Oral Surg Oral Med Oral Path 1963; 16: 466–473.
Baumgartner J C, Heggers J P, Harrison J W . The prevalence of bacteraemia related to endodontic procedures. I. Nonsurgical endodontics.. J of Endo 1976; 2: 135–140.
Klotz M D, Gerstein H, Bahn A N . Bacteraemia after topical use of prednisolone in infected pulps. J Am Dent Ass 1965; 71: 871–875.
Heimdahl A, Hall G, Hedberg M. et al. Detection and quantification by lysis-filtration of bacteraemia after different oral surgical procedures. J of Clin Microbiol 1990; 28: 2205–2209.
Debelian G J, Olsen I, Tronstad L . (1995) Bacteremia in conjunction with endodontic therapy. Endo and Dent Traumatol 1995; 11: 142–149.
Roberts G J, Gardner P, Longhurst P, Black A E, Lucas V S . Intensity of bacteraemia associated with conservative dental procedures in children. Br Dent J 2000; 188: 95–98.
Baumgartner J C, Heggers J P, Harrison J W . Prevalence of bacteraemia related to endodontic procedures. II. Surgical endodontics.. J of Endo 1977; 3: 399–402.
Dajani A S, Taubert K A, Wilson W. et al. Prevention of bacterial endocarditis. Recommendations of the American Heart Association. J of Am Med Ass 1997; 277:: 1794–1801.
McGowan D A . General and systemic aspects of endodontics. Chapter 2 in: Pitt Ford T R (ed). Harty's Endodontics in Clinical Practice 1997; 4th Edition. Oxford, UK.
Bender I B, Naidorf I J, Garvery G J . Bacterial endocarditis: consideration for physician and dentist. J of Am Dent Ass 1984; 109: 415–20.
Gelfand M, Sunderman E J, Goldman M . Reliability of radiographic interpretations. J of Endod 1983; 9: 71–5.
Dummer P M H, McGinn J H, Rees D . The position and topography of the apical canal constriction and apical foramen. Int Endo J 1984; 17: 192–8.
Shabahang S, Goon W Y, Gluskin A H . An in vitro evaluation of Root ZX apex locator. J of Endo 1996; 22: 616–8.
Pagavino G, Pace R, Baccetti T . A SEM study in vivo accuracy of the Root ZX electronic apex locator. J of Endo 1998; 24: 438–41.
Durack D T . Prophylaxis of infective endocarditis. In: Mandell GL, Douglas R G, Bennett J E, ed.. Principles and practice of infectious diseases 3rd ed. New York: Churchill Livingston, 1990: 716–721.
Baltch A L, Pressman H L, Schaffer C. et al. Bacteraemia in patients undergoing oral procedures: study following parenteral antimicrobial prophylaxis as recommended by the American Heart Association 1977. Arch Intern Med 1988; 148: 1084–1088.
Hall G, Hedstrom Sa, Helmdahl A, Nord C E . Prophylactic administration of penicillins for endocarditis does not reduce the prevalence of post extraction bacteremias. Clin Infect Dis 1993; 17: 188–194.
Durack D T . Prevention of infective endocarditis. N Eng J Med 1995; 332: 38–44.
Francioli O, Glauser M P . Successful prophylaxis of experimental streptococcal endocarditis with single doses of sublethal concentrations of penicillin.. J Antimicrob Chemother 1985; 15 (Suppl A): 297–302.
Morellion P, Francioli P, Overholser D. et al. Mechanism of successful amoxicillin prophylaxis of experimental endocarditis due to streptococcus intermedins. J Infect Dis 1986; 154: 801–807.
MacFarlane T W, Ferguson M M, Mulgrew C J . Post-extraction bacteremia: role of antiseptics and antibiotics. Br Dent J 1984; 156: 179–181.
Tzukert A A, Leviner E, Sela M . Prevention of infective endocarditis: not by antibiotics alone. Oral Surg Oral Med Oral Pathol 1986; 62: 385–388.
Svinhufuud L B, Heimdahl A, Nord C E . Effect of topical administration of vancomycin versus chlorhexidine on – hemolytic streptococci in oral cavity. Oral Surg Oral Med Oral Pathol 1988; 66: 304–309.
Durack D T . Infective and noninfective endocarditis. In: Hurst JW, Schlant R C, Rackley C E, Sonneblick E H, Wenger N K. Ed.. The Heart 7th ed. New York: McGraw Hill, 1990: 1230–1252.
Gould I M, Buckingham J K . Cost effectiveness of prophylaxis in dental practice to prevent infective endocarditis. Br Heart J 1993; 70: 79–83.
Buckingham J K, Gould I M, Teruitt G. et al. Prevention of endocarditis: communication between doctors and dentists. Br Dent J 1992; 172: 414–415.
Smith J W, Johnson J W, Cluff L E . Studies on the epidemiology of adverse drug reactions. II An evaluation of penicillin allergy. N Engl J Med 1966; 274:: 998–1007.
Parker C W . Allergic reactions in man. Pharmacol Rev 1982; 34: 85–104.
Weiss M E, Adkinson N E . β-lactam allergy. In: Mandell, G L, Douglas R G, Bennett J E. Ed. Principles and practice of infectious diseases. 3rd edn. New York: Churchill Livingstone1990.
Tzukert A A, Leviner E, Benoliel R, Katz J . Analysis of the American Heart Association for the prevention of infective endocarditis. Oral Surg Oral Med Oral Pathol 1986; 62: 276–279.
Hart C A . Antibiotic resistance: an increasing problem? It always has been, but there are things that we can do. Br Med J 1998; 316:: 1255–1256.
Palmer N A V, Pealing R M, Ireland R S, Martin M V . A study of prophylactic antibiotic prescribing in National Health Service general dental practice.. Br Dent J (in press).
Longman L P, Marsh P D, Martin M V . Amoxycillin resistant oral streptococci and experimental infective endocarditis in the rabbit. J Antimicrob Chemotherap 1992; 30: 349–335.
Opal S M, Mayer K H, Medeiros A A . Mechanisms of bacterial antibiotic resistance.. In; Mandell GL, Bennett JF, Dolin R. Principles and Practice of Infectious Diseases 8th Edn, Churhill Livingston, London.
Durack D . Antibiotics for prevention of endocarditis during dentistry: Time to scale back? Annal Intern Med 1998; 129: 829–831.
Clemens J D, Ransohoff D F . A quantitative assessment of pre-dental antibiotic prophylaxis for patients with mitral valve prolapse. J Chron Dis 1984; 37: 531–544.
Bor D H, Himmelstein D U . Endocarditis prophylaxis for patients with mitral valve prolapse; a quantitative analysis. Am J Med 1984; 76: 711–717.
Pallasch T J . A critical appraisal of antibiotic prophylaxis. Int Dent J 1989; 39: 183–196.
Lacassin F, Hoen B, Leport C. et al. Procedures associated with infective endocarditis in adults, a case control study. Eur Heart J 1995; 16: 1968–1974.
Simmons N A, Ball A P, Cawson R A. et al. Antibiotic prophylaxis and infective endocarditis. Lancet 1992; 339: 1292–1293.
Working Party of the British Society for Antimicrobial Chemotherapy. Antibiotic prophylaxis for infective endocarditis. Lancet 1992; 1: 1292–1293.
Martin M V, Butterworth M L, Longman L P . Infective endocarditis and the dental practitioner: a review of 53 cases involving litigation. Br Dent J 1997; 182: 465–468.
CRD Report 4 After Undertaking Systematic Reviews of Research on Effectiveness. University of York Centre for Reviews and Dissemination, 1996.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Seymour, R., Lowry, R., Whitworth, J. et al. Infective endocarditis, dentistry and antibiotic prophylaxis; time for a rethink?. Br Dent J 189, 610–616 (2000). https://doi.org/10.1038/sj.bdj.4800845
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800845
This article is cited by
-
Microbiota present in combined endodontic-periodontal diseases and its risks for endocarditis
Clinical Oral Investigations (2023)
-
IE advice
British Dental Journal (2019)
-
Bacterial DNA detected on pathologically changed heart valves using 16S rRNA gene amplification
Folia Microbiologica (2018)
-
Current knowledge among Japanese experienced general dentists regarding prevention of infective endocarditis
Odontology (2018)
-
Empfehlungen zur zahnärztlich-chirurgischen Sanierung vor Herzklappenersatz
Der MKG-Chirurg (2012)