Key Points
-
Autoclave performance must be monitored routinely
-
Three methods of monitoring autoclave performance are available — physical, chemical and biological
-
Sterilisation of instruments also involves proper cleaning of the instruments prior to sterilisation and correct packing of the instruments in the autoclave.
Abstract
The sterilisation of instruments is central to the infection control process in the dental surgery, with the autoclave being most frequently used for this process. For effective operation, among other factors, it is essential that the autoclave is loaded correctly and tested regularly to ensure that it is operating at a temperature and pressure which will kill all micro-organisms. Biological indicators are another method of verifying the sterilisation process, since the sterilisation of the bacterial spores within the test ampoule provides a guarantee that sterilising conditions have been achieved.
Similar content being viewed by others
Main
A number of methods are available for the sterilisation of instruments in the dental surgery. Among these are the steam autoclave, the rapid steam autoclave, the unsaturated chemical vapour steriliser (chemiclave), and the dry heat oven. The use of chemiclaves appears to be declining because of their cost and the presence of the sterilising chemicals, although they offer the speed of an autoclave and reduced risk of rusting or dulling of carbon steel materials. Dry heat ovens also produce little rusting or dulling of instruments, they are inexpensive to purchase but have substantially longer treatment cycles than an autoclave or chemiclave. Their use appears to be mainly restricted to less developed countries. It is for the practitioner to decide which method is most appropriate to their clinical practice.
The use of a steam autoclave has long been advised as a means of sterilisation of instruments used in the dental surgery,1,2,3 with results of a recent survey indicating that this advice has been accepted by all but a very small proportion of UK dental practitioners.4 Even when not required to do so by law, the dental practitioner has a moral and ethical responsibility to minimise the chances of cross infection. It is therefore the aim of this paper to discuss the means by which the dental surgery autoclave may best be used: it is not the aim to discuss the very different situation prevailing in hospitals. A second objective is to encourage practitioners to make the sterilisation not only effective, but also efficient.
Optimum operating conditions
The recommended operating conditions for the steam autoclave for heat sensitive instruments are 121°C to 124°C at 1.1 to 1.25 bar pressure for a minimum of 15 minutes, or 134°C to 137°C at 2.1 to 2.3 bar pressure for a minimum of 3 minutes.5 A cycle of 126°C to 129°C at 1.4 to 1.6 bar pressure for 10 minutes is also recommended by some manufacturers. Manufacturers' instructions for the use of the equipment should be read and followed. Ideally, time should be allowed for 'warm up', with the autoclave run empty at the beginning of the working day.6 Many autoclave types have an automatic 'warm-up', with the time cycle only commencing at a certain temperature. It would appear advisable to run multiple smaller loads rather than one larger one, as this should minimise the risk of insufficient steam penetration into the depth of the load and facilitate air removal from the chamber.
The aim of sterilisation of instruments and their storage is to deliver sterile instruments to the chairside, thereby preventing the risk of cross infection from patient to patient and between dental healthcare worker and patient by contaminated instruments. Appropriate wrapping materials should therefore be used if instruments are to be stored after sterilisation,3 since unwrapped sterilised instruments will require handling and will therefore have a zero shelf life. Wrapping serves to protect sterile instruments from contamination prior to their use. Furthermore, unwrapped non-sterile instruments cannot readily be distinguished from those that have been sterilised. If instruments are not wrapped, it would appear necessary:
-
For the practitioner to adopt an ultra-disciplined approach to segregation of dirty instruments from clean, and,
-
For the practitioner to use a flow 'production' process.
It is the consideration of the authors that unwrapping pre-packaged instruments at the chairside in view of the patient also should serve to improve patient confidence in the infection control regimen of the practice. In this respect, results of a survey of 840 UK dentists (52% response) indicated that only 54.6% of practices surveyed had special facilities for storing sterile instruments and that 67.1% of instruments were routinely covered after autoclaving.7 It may be considered that this is a cause for concern, given the potential for contamination of uncovered instruments.
Coverings and containers for instruments should permit free circulation of steam. Non-perforated, closed containers or aluminium foil are contra-indicated for use in an autoclave as they will prevent the steam from reaching the items inside. Suitability of all closed containers should be confirmed by spore testing6 (vide infra). See-through plastic or paper-plastic tubing or pouches may be used. Pins, staples or paper clips should not be used as these make holes in the wrap that permits entry of micro-organisms.3 Thin paper bags which allow sharp instruments to protrude are contra-indicated. In order to permit displacement of air and facilitate contact with steam, wrapped packages should ideally be placed well apart in the autoclave so that steam has access to all package surfaces. Packages should not be stacked.
Advice on packaging of dental instruments
There remains some ambiguity within the dental literature on the advisability of packaging dental instruments. The current UK position is that, because of the perceived difficulties of ensuring removal of air and penetration of steam into wrapped instrument packs, benchtop steam autoclaves which do not have a vacuum cycle to remove air — and this includes the majority of UK dental practice autoclaves — should be used to sterilise unwrapped instruments only. However, this practice does not address the problem of storage of unwrapped instruments. In practice, unwrapped instruments will soon become non-sterile, although they are likely to remain pathogen free and have only low numbers of environmental contaminants. This should pose no risk to the healthy patient, provided that they are covered with a clean towel or paper in order to avoid the settling out of dust or aerosols containing spores and used within a short time after autoclaving.
In the US, packaging of instruments has been the norm for about 5 years, and a number of regulatory agencies and professional organisations have recommended packaging of instruments for sterilisation. These include the Centers for Disease Control8 and the American Dental Association.3 In the US, the majority (85%) of dental practices have at least one gravity steam autoclave. Few use larger model high-vacuum autoclaves because of need, size and price. Accordingly, packing of instruments prior to sterilisation has been recommended by a number of regulatory agencies and professional associations for some years. This process has been continually assisted by the development of improved wrapping materials and metal cassettes.
Ideally, practitioners should check with autoclave manufacturers that packaging which they employ has been validated for use with their particular autoclave. Benchtop autoclaves with a vacuum cycle are now available in the UK and it could be anticipated that their use would clarify any ambiguity over the packaging and storage of sterilised instruments.
Distilled water and detergent
Distilled water should be used for the autoclave instead of tap water, given that tap water contains dissolved minerals, such as calcium, which may form deposits on the pipes and chambers of the autoclave. The autoclave seals, drains and fittings should be inspected regularly, and all internal surfaces should be regularly wiped with distilled water. A number of manufacturers produce or supply a detergent cleaner or recommend one for use with their autoclave, with the frequency of cleaning being set by the number of cycles or operational days. However, if this is not part of the manufacturer's instructions, it would appear prudent to check with the manufacturer prior to using such a detergent lest this should lead to invalidation of the manufacturer's warranty.
Preparation of instruments for sterilisation
Soiled instruments should be cleaned prior to sterilisation, since the presence of blood and debris may adversely affect steam penetration and thereby prevent the sterilisation temperature being achieved in the depth of the deposit. Debriding instruments for sterilisation should be considered to be a two-stage procedure — presoaking and cleaning. Ideally, instruments should be cleaned after use, but the practice routine and patient throughput may not always allow this; instruments should therefore be placed in a 'holding' container in a presoaking solution.9 For this process, a detergent solution should be used. It should operate by preventing the instruments from drying, although some such as those based upon phenolics and quaternary ammonium disinfectants possess cleaning and disinfectant properties. However, quaternary ammonium compounds are rapidly inactivated by organic material. The presoaking should not be an extended process, as increased time in the solution will increase the likelihood of rusting of non-stainless steel instruments such as burs. Heavy duty gloves and eye protection should be used while handling instruments at this stage to avoid sharps injury.
After soaking, the instruments should be cleaned by handscrubbing or by ultrasonic cleaning. The latter is preferred, not only because studies have shown the superiority of ultrasonic cleaning,10 but also because of the greater risk of sharps injury with increasing handling of instruments. Furthermore, splatter from contaminated instruments may contaminate the area beyond the sink during scrubbing. The ultrasonic cleaner is particularly appropriate to hinged instruments and those with moving components, although the majority of handpieces cannot be ultrasonically cleaned. Loose instruments should be placed in a basket within the ultrasonic cleaner; this holds instruments off the floor of the bath, closer to the centre of the bath where cleaning is most efficient. The ultrasonic bath cover should be kept in place while the unit is in operation. The use of a cleaning solution designed for use with the apparatus is preferable — with such solutions, presoaked instruments may be cleaned in less than 5 minutes. The solution should be replaced after several loads of instruments have been cleaned, and at the end of the working day the unit should be drained and cleaned.
Monitoring sterilisation
The sterility of instruments used in the dental surgery is a fundamental aspect of the surgery infection-control regimen. A significant part of such a process is continuous quality monitoring. It is therefore essential that the surgery autoclave is monitored regularly to ensure that it is operating at a temperature and pressure which will kill all micro-organisms. It is not possible to check visually whether instruments have been sterilised, and direct culturing of each instrument would make them unsuitable for use. There is therefore no readily available procedure which actually proves the sterility of each instrument; it is only possible to monitor a given processed autoclave load, and to employ correct operational conditions and use equipment which is correctly serviced. The monitoring procedures should be easily operable, convenient to analyse and inexpensive. A number of procedures may be employed:
-
1
A simple method of monitoring is observation of the autoclave gauges and timers during the operational cycle, recording the temperature time and pressure of operation in a log book; a number of autoclaves provide a print-out of these parameters.
However, the reliability of this method may be questioned since in some models of autoclave currently in use in general dental practice, the circuits controlling the cycle are shared by the temperature gauge and erroneous readings may result. It would therefore appear that the fitting of an independent, accurate log printer is desirable. Using this method, each autoclave cycle may be monitored accurately and with confidence.
-
1
An external chemical monitor such as autoclave tape may be used, in which a chemical is impregnated into the surface of an autoclave bag or pouch. A colour change indicates the achievement of an adequate temperature cycle. Internal chemical monitors operate in a similar manner, but the chemical is placed within the pack or tray. These chemical monitors are inexpensive and do not require the purchase of additional equipment, but they only change colour at specific temperature and/or time cycles and cannot therefore be an absolute guarantee of sterility.
-
2
Biological indicators (BI) may be used to verify the sterilisation process,6 because they measure if highly resistant bacterial spores have been killed. If the spores are killed, it may be assumed that all other microbes present on dental instruments have also been killed.
Spore tests therefore may be considered to monitor whether the operational parameters of the autoclave are achieving the conditions necessary to kill micro-organisms, while chemical indicators usually monitor a single parameter, such as the achievement of a desired temperature. A number of authorities have recommended that a biological indicator should be used within a pack or pouch at least once a week.3,5,6,9 For steam autoclaves, the use of Bacillus stearothermophilis spores are recommended, and Bacillus subtilis is recommended for dry heat. In the USA, 11 states now have laws requiring regular spore-testing of dental practice autoclaves.11,12,13 However, the European Standard for Sterilisation of Medical Devices does not address the use of biological indicators as they consider that these are of limited value in moist heat sterilisation, and recommend that they should be used in addition to the measurement of physical parameters.14 Any quality assurance programme must include quality assessment or proficiency testing in which a challenge is made to the quality control procedures.
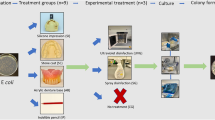
Spore tests come in several forms; spore strips are made from heavy porous paper containing spores varying in concentration from 10,000 to 100,000 per strip. After autoclaving, these strips are placed in culture medium and incubated for 7 days at 56°C after which it may be determined if the spores have been sterilised. Perhaps a simpler method of spore testing is by means of spore test ampoules such as ATTEST (3M Healthcare, St.Paul, MN, USA) (Fig. 1) which are placed in the centre of an autoclave load, and incubated on removal. The spore ampoule contains a glass vial of media which is released upon crushing, following which the ampoule is incubated for 48 hours at 56°C. Accordingly, while this method provides absolute evidence of the sterility of an autoclave load, it suffers from the disadvantage of this delay in obtaining the results.
When the effectiveness of autoclaves was assessed using spore tests in dental practices in USA,15,16 Norway,17 and Germany,18 results of tests indicated failure rates of 15%,15 33%,16 23%,17 and 12%,18 respectively. A failure rate of 4.4% has been reported when 4,579 steriliser loads were tested in Canada,19 while a failure rate of 2.3% to 7.3% was reported in Denmark.20 Most recently, when 840 UK dentists (52% response) were asked to test their practice autoclaves using spore test ampoules, 4% of the autoclaves failed to sterilise the ampoules, and only 70% of respondents reported that they checked their autoclave performance.7 These results appear to show the need for routine monitoring of steriliser performance, perhaps with every cycle, but certainly on a routine basis. A mini-incubator for use with spore test ampoules intended for use in dental practice has recently become available.
The three main monitoring processes
In summary, monitoring should include three main processes — physical, chemical and biological monitoring. Each serves an important purpose and helps to define the operation of the sterilisation unit. Physical monitoring through observation of permanently placed gauges such as temperature and pressure monitors should be supported by print-outs. The occasional use of thermocouples, which generally report internal temperatures, may also be valuable. Chemical monitoring provides immediate evidence that a sterilisation parameter was present during an autoclave cycle. Biological monitors are the main guarantee of sterilisation for two reasons — they simultaneously monitor the interaction of all sterilisation parameters (temperature, pressure and time). No gauge, thermocouple or chemical monitor can accomplish this. Furthermore, the biological indicator (BI) can measure the sterilisation process within an individual pack, tray or instrument grouping. They can report the effect that the presence of an instrument load actually had on steriliser effectiveness. Anecdotal accounts exist in which biological failures occurred although printouts showed correct functioning of an autoclave. Such failures may be related to human error, such as improper wrapping and/or loading of an autoclave, not to machine malfunction. A BI would have shown these failures, but BI should never be used alone, given the delay in obtaining results — this may vary from 12 hours to several weeks depending on the incubator employed. Given that the European Standard is now 6 years old,14 it may be that it is now time for Europe to re-evaluate its stance on biological monitors.
Conclusion
Effective operation of the dental surgery autoclave is dependent on many factors. Regular monitoring of its operation to check that it is operating at a temperature and pressure which will kill all micro-organisms is an essential element of the dental surgery infection control routine.
References
British Dental Association. Guide to blood borne viruses and the control of cross infection in dentistry. British Dental Association, 1988.
Centers for Disease Control and Prevention. Recommended infection control practices for dentistry. MMWR 1993; 41(RR-8): 9–10.
ADA Council on Scientific Affairs and ADA Council on Dental Practice. Infection control recommendations for the dental office and the dental laboratory. J Am Dent Assoc 1996; 127: 672–680.
Burke F J T, Wilson N H F, Cheung S-W . Glove use by dentists in England and Wales: results of a 2-year follow-up survey. Br Dent J 1994; 176: 337–341.
Miller C H . Infection control. Dent Clinics N Amer 1996; 40: 437–456.
Palenik C. J., Miller C. H. Improving the performance of the office steriliser. Dent Asepsis Rev 1991; 12: 1–2.
Burke F J T, Coulter W A, Cheung S W, Palenik C . J. Autoclave performance in and practitioner knowledge of autoclave use: A survey of selected UK practices. Quintessence Int 1998; 29: 231–238.
US Department of Health and Human Services, Centers for Disease Control. Practical Infection Control in the Dental Office. 1989, USPHA, Washington, DC.
Miller C H . Cleaning, sterilisation and disinfection:basics of microbial killing for infection control. J Am Dent Assoc 1993; 124: 48–56.
Miller C H, Riggen S D, Sheldrake M A, Neeb J M . The presence of microorganisms in used ultrasonic cleaning solutions. Am J Dent 1993; 6: 27–31.
Infection control rules. Columbus, Ohio: Ohio State Board of Dental Examiners, 1992.
ADA Department of State Government Affairs. Five states move quickly on handpiece sterilisation. J Am Dent Assoc 1992; 123: 119–120.
Indiana Public Law 123-1988. Dental on-site compliance review check-list. Indianapolis: Indiana State Department of Health, Dental Disciplinary Board, 1992.
European Standard BS EN 554:1994. Sterilisation of Medical Devices – Validation and routine control of sterilisation by moist heat.
Palenik C J, King T N, Newton C W, Miller C H, Koerber L G . A survey of sterilisation practices in selected endodontic offices. J Endod 1986; 12: 206–209.
Simonsen R J, Schachtele C F, Joos R W . An evaluation of sterilisation by autoclave in dental offices. J Dent Res 1979; 58: 400.
Skaug N . Proper monitoring of sterilisation procedures used in oral surgery. Int J Oral Surg 1983; 12: 153–158.
Engelhardt F P, Fisvatin H . Hygiene in der Zahnartzpraxis – Wunsch und Wirklichkeit. Dtsch Zahnarzd Z 1976; 31: 277–281.
McErlane B, Rosebush W J, Waterfield J D . Assessment of the effectiveness of dental sterilisers using biological monitors. J Canad Dent Assoc 1992; 58: 481–484.
Scheutz F, Reinholdt J . Outcome of sterilisation by steam autoclaves in Danish dental offices. Scand J Dent Res 1988; 96: 167–170.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Palenik, C., Burke, F., Coulter, W. et al. Improving and monitoring autoclave performance in dental practice. Br Dent J 187, 581–584 (1999). https://doi.org/10.1038/sj.bdj.4800338
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800338
This article is cited by
-
Decontamination practices of paediatric crowns: a systematic review
European Archives of Paediatric Dentistry (2022)