Abstract
Objective To describe the morbidity related to general anaesthesia provided in general dental practices for the extraction of teeth in school children.
Design Observational study supported by structured questionnaires and interviews.
Setting Three general dental practices in a Lancashire health district and children's homes.
Subjects 80 children aged 5–15 years undergoing extractions under general anaesthesia.
Main outcome measures Observed demeanour of the children prior to, during and immediately after the surgical procedures. Reported morbidity during the following 24 hours and 1 month later.
Results 92% of the children complained of symptoms associated with the surgery under general anaesthesia. Distress was noted in 16 (20%) patients during the induction of 26 (33%) during recovery. Continued crying was reported for 24 (39%) during the journey home and for 23 (37%) once home had been reached. Other symptoms included nausea, vomiting, sickness and prolonged bleeding. Six reported psychological trauma 1 month after; three had nightmares, two had continuing bad memories and one was depressed for several days.
Conclusion Morbidity following extractions under general anaesthesia in general dental practice is common and has distressing consequences for the young patients and their carers.
Similar content being viewed by others
Main
The use of general anaesthesia for the extraction of teeth in young people is still common in the UK, with nearly 70% of the total number of administrations being given to patients under the age of 15 years, nearly 80% of these treatments were given in the primary dental care sector.1 The procedure involves the minimum of preparation, usually with no premedication, and the need to leave the premises within a short period of time. While admitting that there still seemed to be a need for this service, the Expert Working Party on General Anaesthesia, chaired by Professor Poswillo appreciated the innate dangers involved and recommended that this form of anaesthesia for tooth extraction should be minimised.1 The risk of mortality from general anaesthesia in the dental chair while extremely serious is so rare that it is an inadequate measure of outcome. The Working Party were concerned at the lack of data on morbidity, a much more common complication. The Clinical Advisory Standards Group report on dental general anaesthesia recommended that a prospective study on morbidity is required.2
This lack of data is particularly surprising when it is appreciated that more than 230,000 general anaesthetics were given in England in 1994/95 for the extraction of teeth in patients under the age of 18 years.3 In the north-west of England, where fluoridation of the water supplies has still to be introduced and caries prevalence is the highest in England,4 extraction under general anaesthesia is a very common occurrence often involving many teeth. In that Region alone more than 47,000 administrations were given in 1994/95.3 It is important to understand the type and degree of morbidity these young people may experience as a result.
Morbidity following general anaesthesia for dental extractions, in its general sense of adverse effects, can manifest itself in varying degrees of severity across a range of physiological, pathological, psychological or social effects. The more serious morbidities, such as arrhythmias and liver damage associated with the use of Halothane and the possibility of hypoxia in consequence of administration in the supine position have been reported.5 The more common sequelae of nausea, vomiting, headache and drowsiness have not received the same attention. Those studies that have been reported are limited to the first 24 hours, and have generally been based on day-case anaesthesia in hospital clinics.6,7 Although these symptoms may be regarded by some as trivial it is likely that they will have a profound effect on the young child. Other anaesthetic agents such as Sevoflurane are being used in an attempt to reduce morbidity.8 In view of the large numbers of general anaesthetics that are administered to children in general dental practice it is unfortunate that such symptoms have not been thoroughly investigated in this environment.
The aim of this study was to investigate the prevalence, nature and severity of the morbidity associated with general anaesthesia given in general dental practice for the extraction of teeth to patients 5–15 years of age living in a district of Lancashire. Emphasis was placed on the children's perspective particularly with regard to their physical and emotional wellbeing.
Method
The study took place in the only three general dental practices in a health district in Lancashire offering an extraction service under general anaesthesia. The district contains both urban and rural communities where levels of dental caries are among the highest in England and are considered to be associated with relative material disadvantage. The local ethics committee approved the protocol.
All children between the ages of 5–15 years who attended for extractions under general anaesthesia were included in the study. To measure morbidity to within 10% (SE = 5%) it was estimated that at least 69 children needed to be observed. It was known from a pilot study that the main investigation would need to span 4 weeks to achieve this sample. During this period 80 children were eligible and included. Informed consent was obtained and no child or parent refused.
The research was conducted in two phases. The first was a quantitative study over the first 24 hours recording experiences before, during and after the administration of the anaesthetic. The second was a qualitative investigation arranged 1 month after the anaesthetic and took the form of unstructured interviews at the patients' homes.
Phase 1
After the patients had been 'booked-in' and informed consent obtained, a 'delegated dental nurse' asked the accompanying adults to complete a structured, closed questionnaire. This included a series of questions about the patients' dental and social histories, about the journeys to the practices, and about the parents' own dental histories. The children were then addressed about their knowledge of the procedure to be carried out. They were also asked to show their feelings by completing a Wong/Baker Faces Rating Scale which shows a diagrammatic series of faces from 'very happy' to 'very sad' asking them to choose that which most closely represented their current feelings.9 In addition they were asked whether or not their teeth were hurting.
The patient then entered the operating room and was directly observed by one of the authors (CMB) who recorded the nature of the anaesthetic used and the treatment carried out. The length of time from induction to recovery was noted. The end of the anaesthetic was the time when the patient opened his or her eyes on request. The patient was then taken to the recovery room where any immediate side effects either observed or reported by the child were noted. In addition, the occurrence of haemorrhage, crying and vomiting were recorded.
On leaving the practices, the accompanying adults were given a questionnaire which they were asked to fill in and return by post. This requested details of the journey home and the events during the first 24 hours post-operatively. Questions were asked about the patient's condition on the journey, the presence of pain and the patient's behaviour including eating and sleeping. The adult's feelings about the procedure were also sought.
Phase 2
The overall intention of this phase of the study was to obtain from the patients, accounts of their experiences of having a general anaesthetic in general dental practice. To do this, the children were seen in their homes by one of the authors (CMB) 1 month after the anaesthetic induction by which time it was hoped that the sequelae of the treatment would have resolved. The meetings took the form of a qualitative enquiry using the 'surveying through stories' method.10 Each child was asked 'to tell the story of what happened the day you went to the dentist to have your teeth out'. The conversation was conducted in the presence of at least one parent who sometimes made a contribution. An assistant using a consistent method recorded in shorthand the contents of the discussion.11 The records of the interviews were analysed using a 'cut and paste' method described by Addison.12
Results
Of the 80 patients who took part in the study, 43 were boys and 37 were girls with an age range of 5–15 years and a modal age of 7–8 years (28%). They came from all social classes, but 58 (73%) were from households with manual or unclassified occupations, with 21 (26%) living in single parent or unemployed families. The accompanying adults claimed that 53 (66%) of the children were 'regular attenders', with 59 (74%) having had restorations, 39 (49%) experiencing local analgesia and 30 (38%) general anaesthesia. Most of the adults (56, 70%) claimed not to be anxious about receiving dental treatment.
The distances travelled to the practices varied from 1 to 15 miles, most of the patients (41, 51%) coming by car with 35 (44%) walking. Once the preliminaries had been completed, the most common waiting time was nine minutes and the maximum was 43 minutes.
Most (70, 87%) of the patients were aware of the procedures to be administered at this visit, but four did not know whether they would lose consciousness or not and three thought that they would be awake throughout the procedure. When asked to respond to the Wong/Baker Faces Rating Scale, 44 (55%) indicated that they were happy, 29 (36%) that they were apprehensive, and seven (9%) that they were sad or very sad. Most (66, 82%) had not experienced toothache on the day of the visit.
In the surgeries, three anaesthetists gave 62 (77%) inhalation and 18 intravenous inductions, all of which were administered in the upright position. Methohexitone was the intravenous agent of choice and in five cases it was the sole agent used. The remaining 75 (94%) children all received oxygen. Halothane was administered to 68 (85%) of the children and nitrous oxide to 73 (91%). At least 16 (20%) of the patients showed distress during the induction, one of them being seriously distressed and another vomiting. No intubations took place. Five operators removed 50 permanent and 160 deciduous teeth, while in addition, eight (10%) patients had some minor restorative treatment. The most usual length of time was 3 minutes with a mean of 5.9 minutes (SD = 3.5). The total anaesthetic time ranged from 2 to 20 minutes, the restorative treatment accounting for the longer periods.
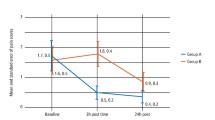
During the immediate post-treatment phase, 26 (33%) of the patients were distressed with one micturating; 22 (28%) were in pain, six (8%) had headaches, nine (11%) felt sick, five (6%) vomited, 57 (71%) were bleeding and 35 (44%) were crying (Table 1).
During the journey home, of the 62 (78%) parents who returned the questionnaire, 15 (24%) said the child was still in pain, 24 (39%) children were crying, 19 (31%) felt sick, three (5%) vomited and 23 (37%) were still bleeding (Table 1). On returning home, all but three of the children were looked after by a parent, of whom 16 (20%) said they were very anxious about the outcome of the visit. Once at home, 12 children (19%) were still in pain, 23 (37%) were still crying, 11 (18%) felt sick, eight (13%) vomited, nine (15%) were still bleeding and 7 (11%) did not eat later that day (Table 1).
That night, seven (11%) patients slept badly, and the following day 13 (21%) were still in pain and eight were still upset. Thirteen (21%) of the parents were still very anxious about the outcome of the treatment.
One month after the treatment, 69 (86%) of the children were contacted at home and gave their account of the treatment experience. The waiting period upset 18 (26%) of the children and 20 (29%) disliked the appearance of the surgery on entering it. There were too many people in the room and some were frightened by being strapped into the chair.
Intravenous induction seemed more popular than inhalation. One child said: 'I can remember the prick. It felt good. I felt funny for a few seconds then I fell asleep'. In contrast another said: 'I got the gas thing put on my face. I was shaking. He said to someone "turn it up a bit". I tried to tell them; I wanted to tell someone. I was trying to get it off and I was struggling. It was really horrible'.
Some of the comments made by the patients a month after their experience of extractions under general anaesthesia described their feelings more vividly than the raw data. For example, seven (10%) children remembered feeling sick later that day. However, when describing this, one said:'When I got home I felt sick. Then I was sick that afternoon and I felt faint all the time'. Three children said that they had nightmares following the treatment, two had continuing bad memories and one was depressed for several days. One said: '... I had a nightmare about what happened to me. The dream was — I was strapped with the belts and I couldn't get out'. Another said: 'I still have nightmares about it. I will never forget it. Every time I go near that dentist's I get a funny feeling'. The treatment itself can also be distressing. One child said: 'I was glad when I woke up. I felt relieved it was all over and I was glad there was some teeth left, because I thought they were all going to be taken out'. Another said: 'All the blood came out and all the bleeding was in the sink'.
Parents also took the opportunity to raise some issues. One parent said: 'He cried all the way home and didn't stop until 4 o'clock. He was crying most of the day'. Another said: 'He was vomiting when I got home'. A third said: 'He broke his arm two weeks ago and he thought he was going to have gas again. They had a mask with oxygen and he was shaking and terrified. He thought it was going to be the same'. Many adults may recall similar memories from the past.13
Discussion
The morbidity reported in this study emphasises that dental extractions under general anaesthesia do produce sequelae, 92% of the children complaining of one or more symptoms. This compares well with the 91% reported by Holt et al.7 but is greater than the 61% described by Ogg.14
The lack of a control group precludes the conclusion that all the morbidity reported resulted from the general anaesthetic. For example, Muir et al.15 reported that the incidence of headaches was similar for both general and local anaesthesia.14 The pain that occurred was mostly due to the surgical procedure and again this might have been similar whatever the anaesthetic used. However, the placement of a mouth prop and a throat pack can cause post-operative trauma, and the need to keep the anaesthetic as brief as possible calls for haste during the extraction procedure. The soft tissues of the mouth may also be inadvertently traumatised while the patient is unconscious. Restraining children with a strap while performing extractions under general anaesthetic is a long established method that is still used in some dental practices (one in this study). The distress it may cause outweighs any advantages from having a stabilised patient.
Although the morbidity experienced may seem of a trivial nature, it is common and distressing and has been reported as a factor causing fear of the dentist in later life.16 It is certainly an experience that children can do without.
The use of general anaesthesia in general dental practice is unknown in many other countries, for example, USA, Australia and Scandanavia, and every effort should be made to reduce the use of general anaesthesia in the primary dental care setting in the UK. A comment from one mother formed an appropriate summary: 'Having a child's teeth taken out isn't something as a mother I want to experience again. It wasn't a pleasant experience because he was distressed for some time after'. It is apparent that the parents also suffer distress along with their children15 although this was not studied systematically in this present investigation.
When tooth extraction cannot be avoided, there are more acceptable techniques than general anaesthesia that can be used in the majority of cases.17 More positive steps should be taken to reduce the demand for general anaesthesia for dental extractions, from introducing the fluoridation of public water supplies18 to encouraging the use of more acceptable techniques for exodontia in children such as local analgesia under inhalation sedation.
Conclusion
Morbidity associated with the extraction of teeth from children in general dental practice using general anaesthesia is a common and often harrowing experience for both the patients and the parents who care for them. Appropriate measures to reduce this should be urgently considered.
References
General anaesthesia, sedation and resuscitation in dentistry. Report of an Expert Working Party. London: Department of Health, 1991.
Clinical Standards Advisory Group. Report on Dental General Anaesthesia. London: HMSO, 1995.
The Dental Public Health Northern Quality Improvement Group (1997): An audit of dental general anaesthesia in the North of England 1991/2 to 1994/5. Preston: North West Dental Public Health Resource Centre.
Community Dent Health 1997: 14 (Supplement 1); 30–54.
Hastings G B, Lawther, S, Eadie D R et al. General anaesthesia: who decides and why? Br Dent J 1994; 177: 331–336.
Smith B L, Young P N . Day case anaesthesia. A follow-up of day patients undergoing dental operations under general anaesthesia with tracheal intubation. Anaesthesia 1976: 31: 181–189.
Holt R D, Chidiac R H, Rule D C . Dental treatment for children under general anaesthesia in day care facilities at London dental hospital. Br Dent J 1991; 170: 262–266.
Paris S T, Cafferkey M, Tarling M, Hancock P, Yate P M, Flynn P J . Comparison of Sevoflurane and Halothane for out-patient dental anaesthesia in children. Br J Anaesth 1997; 79: 280–84.
Wong D L, Baker C M . Pain in children, comparison of assessment scales. Pediatric Nursing 1988: 14: 9–17.
Graham H . Surveying through stores. In: C. Bell and H. Roberts (eds) Social researching politics, problems and practices. London: Routledge and Kegan Paul, 1984.
Brodgewic S P . On becoming a family physicia. In Crabtree B F and Miller L W (eds) Doing qualitative research. Research methods for primary care. London: SAGE publications, 1992.
Addison R B . Grounded interpretive research: an investigation of physician socialisation, pp 39–57. Albany State University Press, 1989.
Ogg T W . An assessment of post-operative outpatient cases. Br Med J 1972: 4: 573–576.
Muir V M J . Morbidity following dental extraction. A comparative study of local analgesia and general anaesthesia. Anaesthesia 1976; 31: 171–180.
Todd J E, Lader D . Adult dental health in the United Kingdom 1988. OPCS. London: HMSO, 1991.
Shaw A J, Meechan J G, Kilpatrick N M, Welbury R R . The use of inhalation sedation and local anaesthesia instead of general anaesthesia for extractions and minor oral surgery in children: a prospective study. Int J Paed Dent 1996; 6: 7–11.
Evans D J, Rugg-Gunn A J, Tabari E D, Butler T . The effect of fluoridation and social class on caries experience in 5-year old Newcastle children in 1994 compared with results over the previous 18 years. Community Dent Health 1995; 13: 5–10.
Blain K M, Hill F J . The use of inhalation sedation and local anaesthesia as an alternative to general anaesthesia for dental extractions in children. Br Dent J 1998; 184: 608–611.
Acknowledgements
The authors would like to thank all the practitioners and their staff, children and their parents for giving their time and taking part in this study.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Bridgman, C., Ashby, D. & Holloway, P. An investigation of the effects on children of tooth extraction under general anaesthesia in general dental practice. Br Dent J 186, 245–247 (1999). https://doi.org/10.1038/sj.bdj.4800076
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800076
This article is cited by
-
Piezosurgery versus conventional osteotomy: a randomized clinical trial on pain and anxiety in children with unerupted mandibular third molars
Clinical Oral Investigations (2023)
-
Comparison of Oral Health-Related Quality of Life scores in children treated for early childhood caries under general and local anesthesia: a quasi-experimental study
European Archives of Paediatric Dentistry (2023)
-
Repeat paediatric dental general anaesthesia at Sheffield Children's NHS Foundation Trust: a service evaluation
British Dental Journal (2020)
-
Post-operative pain and morbidity in children who have tooth extractions under general anaesthesia: a service evaluation
British Dental Journal (2019)
-
Does relative analgesia with nitrous oxide reduce the number of general anaesthetic sessions and dental loss?
British Dental Journal (2018)