Abstract
Objective To further investigate the efficacy of N-monochloro-DL-2-aminobutyrate (NMAB) and NMAB containing 2M urea (NMAB-urea) as chemomechanical caries removal reagents in deciduous teeth using standardised lesions and limited applicator pressure.
Design In vitro.
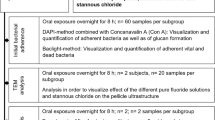
Method Carious dentine was removed from standardised lesions in deciduous teeth using NMAB, NMAB-urea or isotonic saline (control); 50 lesions were studied with each reagent. The surface of the dentine remaining in cavities where complete caries removal was achieved was examined by light and scanning electron microscopy.
Main results NMAB-urea (but not NMAB) gave significantly improved caries removal compared with saline. The dentine surfaces remaining after complete caries removal were irregular and approximately one third were bacterially contaminated.
Conclusions The improved efficacy of NMAB by the addition of urea has been confirmed. Toxicity studies are still necessary prior to clinical use of this reagent.
Similar content being viewed by others
Main
Chemomechanical removal of dental caries involves the chemical softening of dental caries by N-monochloro-DL-2-aminobutyric acid (NMAB) or by N-monochloroglycine (NMG) at pH 11.2-11.4 followed by selective removal of carious material by gentle mechanical excavation. The procedure has been developed as a possible alternative to the conventional mechanical removal of carious dentine.1,2 The reagent is produced by mixing aminobutyric acid or glycine with sodium hypochlorite and the mechanism of action is claimed to involve the chlorination and disruption by NMAB or NMG of the partially degraded collagen fibres found in carious dentine.3,4 The application of NMAB or NMG to carious dentine therefore softens the layer that contains denatured collagen; this then becomes more friable and can be selectively removed by gentle excavation. The layer of dentine containing undenatured collagen fibres is allegedly unaffected.5,6,7
Clinical studies have reported the efficacy of chemomechanical caries removal on all classes of coronal8,9,10 and root surface lesions.11 A review of the literature showed that most of these clinical trials have reported favourably on the efficacy of caries removal.12 Patient acceptance favours this procedure over conventional rotary instrumentation. The system has also been shown to be potentially useful in treating child dental patients13,14,15 and is more effective in the treatment of deciduous than of permanent teeth.12
The procedure is claimed to reduce the need for local anaesthesia because it avoids the painful removal of sound dentine. The use of rotary instruments is also reduced, and sound tooth structure is conserved because only carious tissue is removed. The number of vital pulpal exposures is also said to be reduced.16 Despite the apparent advantages, the limitations of the current procedure regarding treatment time, suitability of cavities and the need for some continued use of mechanical instruments should be recognised and its use must be selective.12 More recently however, two in vitro studies with well-controlled parameters have shown that NMAB is no more effective than saline12 or water17 in the removal of carious dentine in permanent teeth. These findings therefore cast doubt on the validity of previous clinical trials that have not taken into consideration factors such as the force applied and the criteria for assessment for caries removal. The commercial applicator system using the Caridex TM unit was also found to have poor thermostatic and flow rate control.12
In a previous study it was shown that the addition of 2 mol/L urea to NMAB resulted in some improvement in the efficacy of caries removal in vitro.12 In that study,12 a large sample size with permanent and deciduous carious lesions was used in order to compensate for the sample variation. It was found that the system may be of particular use in treating primary carious lesions in deciduous teeth. Caries with a medium to soft consistency was more readily removed. This paper describes a further in vitro study using standardised and well-defined lesions in an attempt to minimise sample variation and to reach a more definitive conclusion on the efficacy of the modified reagent.
Materials and methods
Freshly extracted human deciduous carious teeth (150) were collected as previously described.12 They were radiographed using the long cone paralleling technique with a standardised distance of 0.4m using a custom-made x-ray stand and using Kodak Ultraspeed film. Radiographs were developed in a standard automatic dental x-ray film processor.
All carious lesions were assessed and used by one operator either immediately or within one week of extraction. Teeth not used immediately were stored in phosphate buffered saline containing 0.2% (w/v) sodium azide at 4°C.12 Only primary coronal carious lesions with no radiographic pulpal involvement were used. Isolated lesions without communication with other lesions in the same tooth were selected. They also had easy access with little undermined enamel, medium consistency (when tested with a sharp dental probe), no periapical pathology, eg periapical granuloma, no stained and eburnated dentine caries on the surface of the lesion, were not grossly carious and root resorption was limited to less than one third of the original root length (in the judgement of the operator). Carious tissue was classified as being of medium consistency if it was resistant to probing, not easily removed by mechanical means and readily penetrated by a sharp dental probe.1 The assessment was based on the colour, texture and appearance on the dental radiographs. Visual measurements of the lesion width, length and depth were made using a William's periodontal probe.15
Carious material was removed from the teeth using NMAB, NMAB-urea or isotonic-saline (control) by gentle scraping with an applicator tip similar to that described previously12 but modified in that the tips were made of soft metal that would bend and might also block the flow of solution from the lumen when the force exerted on the tip exceeded on average 1N. This was tested using a hand-held digital force gauge (Model DFG-0.2 K, Shimpo Industrial Co. Ltd., 338 Tonoshirocho, Kuze, Minami-ku, Kyoto, Japan). This served as the upper limit of the force used in the removal of carious dentine. The procedure was continued until either the lesion was deemed caries free by normal visual and tactile criteria or until no more caries could be removed.
The experimental design took the form of a blind trial and one investigator treated all teeth with the coded solutions. The 150 teeth were randomly allocated to the three treatment groups, to produce three groups of 50 teeth each. A colour transparency record was made of each specimen having 'complete caries removal' (using Kodak Ektachrome 50 film) showing the surface of the cavity to the greatest possible advantage for visual reference when sectioning teeth. Each tooth was then sectioned with an osteotome through the centre of the cavity. One half was stored in 3% (w/v) glutaraldehyde buffered with 0.1 mol/L sodium cacodylate at pH 7.4 for critical point drying prior to scanning electron microscopy. The other half was placed in 10% neutral formalin for histological processing. Thirty specimens with complete caries removal were selected for further microscopic study, ten having been treated with NMAB, ten with NMAB-urea and ten with a saline control.
Light microscopy
The other half of each tooth used for histological studies was decalcified in 11.9% (w/v) ethylenediaminetetra-acetic acid (EDTA) until radiographs taken after the decalcification procedure showed no evidence of any remaining mineralisation. Decalcified tissues were dehydrated and embedded in paraffin blocks. Nine sections of 7 μm thick were then prepared at representative depths from three separate areas of each specimen to reduce the possibility that infected tubules might be missed due to the plane in which the sections had been cut. Sections were mounted on glass slides, deparaffinised, dehydrated and stained with haematoxylin and eosin18 or modified Gram-Weigert stain19 for observation under the light microscope. Each slide was examined for the presence of bacteria. Photomicrographs were then taken. No attempt was made to quantify the bacteria present.
Results
The results of the in vitro study involving 150 deciduous teeth and three different solutions for chemomechanical caries removal are shown in Table 1. NMAB-urea was more effective than NMAB alone for complete caries removal; both reagents were more effective than a saline control. However, only NMAB-urea, unlike NMAB alone, showed a statistically significant improvement in complete caries removal as compared with the saline control. The mean times required for complete caries removal ranged from 3.4 to 4.4 minutes and the volumes of solutions required from 160–220 ml. There were no statistically significant differences between any of the three solutions with either parameter.
Light microscopy showed that the dentinal floors of cavities prepared chemomechanically were irregular (fig. 1), a finding in accordance with SEM studies. Approximately one-third of cavities prepared using NMAB or NMAB-urea appeared to be bacteria free but only about one-quarter of those prepared using saline were bacteria free (Table 2).
SEM showed that generally the cavity surfaces had a very uneven appearance with some areas being highly undermined. Cavities prepared using NMAB, NMAB-urea or saline were similar. These surfaces could be composed of 'dentine scale',6 be amorphous or show a combination of both features (fig. 2). Most of the dentinal tubules appeared to be patent on SEM and histological sections through the dentinal tubules enabled the patent tubules to be traced (fig. 1). Some tubules however appeared to be occluded (fig. 2), possibly due to the debris overlaid on the tubule openings. No smear layer was found on the dentinal surface (fig. 1).
Discussion
The results of this study indicated that, contrary to previous in vitro studies,1 NMAB was not significantly more effective than isotonic saline in the chemomechanical removal of dentine caries. These findings were consistent with those of a well-controlled study17 and of our previous study.12 The addition of 2 mol/L urea to NMAB did not significantly improve its effectiveness in 'complete caries removal' when compared with NMAB alone, but was however significantly more effective than isotonic saline. This study therefore confirmed our previous finding that NMAB was only statistically significantly better than a saline control when it contained 2M urea.
The times required and volumes of solution used to achieve 'complete caries removal' were similar for both NMAB and NMAB-urea and were not statistically significantly different. In this study however, the percentages of deciduous teeth with 'complete caries removal' with both NMAB and NMAB-urea were much higher than those in previous in vitro studies on permanent teeth.12
Although the modified formulation (NMAB-urea) seems to be more effective, the toxicity and biocompatability are still unknown. Until these tests have been carried out, clinical use of the improved formulation is not an option.
The surfaces of the dentinal floor in deciduous teeth prepared using the caries removal agents were irregular and confirm the findings using SEM as shown here and in previous publications in permanent teeth7,16 and in deciduous teeth.12
The cavities prepared chemomechanically showed the presence of bacteria in some of the tubules (fig. 1). Only about one-third of cavities prepared using NMAB or NMAB-urea were bacteria free, a level similar to cavities prepared using conventional rotary techniques.21,22 Serial stained sections would however be necessary to detect bacteria which are present in only small numbers in the tissues. Failure to detect stained bacteria in histological sections is not an absolute proof of their absence.19 Dentinal surfaces might also have been contaminated in the non-sterile procedure of preparation.
Both SEM and light microscopy showed the dentinal surfaces after 'complete caries removal' using NMAB or NMAB-urea to be similar to those previously reported.12,23 There were no major morphological differences between the dentine surfaces treated with either NMAB or NMAB-urea and ultra-microscopic features were not influenced by the caries removal agents used so long as 'complete caries removal' was achieved.12 Most of the dentinal tubules observed were patent but some appeared to be occluded. These tubules might have been occluded by the gentle crushing and burnishing action of the applicator tip on the dentine surface23 or by the deposition of reactionary, sclerotic dentine as a result of the caries process. The highly irregular surfaces of the cavity floors seem to indicate the possibility of this being used to advantage in the restoration of the lesion using adhesive restorative materials, especially in the absence of a smear layer as seen in conventional, mechanically prepared cavities.24,25 The dentinal features are predominantly determined by the status of the carious lesions prior to caries removal and probably reflect whether it is demineralising, remineralising or in an arrested state. The presence of both secondary and reparative dentine as shown in histological sections may also contribute to the variation of the surface morphology observed under the SEM.
Recently another development in chemomechanical caries removal systems has appeared with the launch onto the market of Carisolv. This consists of a combination of three different amino acids and has a lower concentration of sodium hypochlorite as compared with NMAB. It comes as a gel and volumes used are very much smaller. A comparison of the effectiveness of NMAB, NMAB-urea and Carisolv has yet to be carried out.26
Conclusions
This in-vitro study in chemomechanical removal of dental caries using 'standardised' primary carious lesions in deciduous teeth and a more standardised application procedure has confirmed that only the improved formulation (NMAB-urea) was significantly more effective than the saline control. The average time required was around 4 minutes and the average volume of NMAB-urea used to achieve complete caries removal was around 220 ml. The dentinal cavity floors remaining were irregular and consisted of secondary and /or reparative dentine; bacteria were present in some cavities which were considered to be clinically 'caries free'. The cavity surfaces formed seem well suited to bonding with composite resins and glass-ionomers. With the recent resurgence of interest in chemomechanical caries removal because of the launch of Carisolv onto the UK market, it is prudent to examine the published data before selecting the most appropriate clinical applications.
We would like to thank Drs H. Elder and I. Montgomery, (Institute of Physiology, The University of Glasgow, UK) for advice and provision of scanning electron microscope, Mr. M. T. Lee (Oral Biology Unit, The University of Hong Kong, HK) for histological preparations and Mr. G. Cheung (Department of Conservative Dentistry, The University of Hong Kong) for technical assistance. The funding from the Scottish Home and Health Department, UK (K/MRS/5O/C1380) and CRC Grants, HK (335/252/0005) is gratefully acknowledged.
References
Schutzbank S G, Galaini J, Kronman J H, Goldman M, Clark R E . A comparison in vitro study of GK-101 and GK-101E in caries removal. J Dent Res 1978; 57: 861–864.
Burke F M, Lynch E . Chemomechanical caries removal. J Ir Dent Assoc 1995; 41: 10–14.
Kronman J H, Goldman M, Habib C M, Mengel L . Electron microscopic study of altered collagen structure after treatment with N-monochloro-DL-2-aminobutyrate (GK-101E). J Dent Res 1977; 56: 1539–1545.
Habib C M, Kronman J H, Goldman M . A chemical evaluation of collagen and hydroxyproline after treatment ith GK-101 (N-chloroglycine). Pharm Ther Dent 1975; 2: 209–216.
Kurosaki N, Sato Y, Iwaku M, Fusayama T . Effect of a carious dentin softener on the dentin and pulp. J Prosthet Dent 1977; 38: 169–173.
Brännström M, Johnson G, Friskopp J . Microscopic observations of the dentine under caries lesions excavated with the GK-101 technique. J Dent Child 1980; 47: 46–49.
Yip H K, Beeley J A, Stevenson A G . The interface of carious and sound dentine. Med Sci Res 1991; 19: 187–188.
McCune R J . Proceedings of a symposium on chemomechanical caries removal: a multicentre study. Compend Contin Educ Dent 1986; 7: 151–159.
Robbins A . Efficacy of GK101E solution (Caridex 100) for caries removal. Gen Dent 1987; 35: 392–393.
Cavel W T, Kelsey III W P, Barkmerier W W, Blankenau R J . Clinical evaluation of chemomechanical removal of cervical caries. Gen Dent 1988; 36: 405–408.
Tavares M, Soparker P M, DePaola P F . Evaluation of a chemomechanical method of caries removal in root surface lesions. Quintessence Int 1988; 19: 29–32.
Yip H K, Stevenson A G, Beeley J A . An improved reagent for chemomechanical removal of dental caries in permanent and deciduous teeth: an in vitro study. J Dent 1995; 23: 197–204.
Rothman D L . Caries removal system: preliminary case reports of four pediatric dental patients. Calif Dent Assoc J 1985; 13: 35–37.
Punwani I C, Anderson A W, Soh J I . Efficacy of Caridex in children and adults. J Pedod 1988; 12: 351–361.
McNiernery H D, Petruzillo M A . A gentle approach to operative dentistry: the Caridex caries removal system. Gen Dent 1986; 34: 282–284.
Goldman M, Kronman J H . A preliminary report on a chemomechanical means of removing caries. J Am Dent Assoc 1976; 93: 1149–1153.
Barwart O, Moschen I, Graber A, Pfaller K . In-vitro study to compare the efficacy of N-monochloro-D,L-2-aminobutyrate (NMAB, GK101E) and water in caries removal. J Oral Rehab 1991; 18: 523–529.
Brain E B, Eastoe J E . Studies in the decalcification of dental tissues for histological purposes. Br Dent J 1962; 112: 277–283.
Watts A, Paterson R C . Detection of bacteria in histological sections of the dental pulp. Int Endod J 1990; 23: 1–12.
Goldman M, Siu L, White R R, Kronman J A . The dentinal surface of composite restorations after chemo-mechanical caries removal. J Pedod 1988; 12: 157–166.
Shovelton D S . A study of deep carious dentine. Int Dent J 1968; 18: 392–405.
Shovelton D S . The maintenance of pulp vitality. Br Dent J 1972; 133: 95–107.
Sherrer J D, Mullis W, Pashley D H . The effect of the Caridex system on dentin permeability. Gen Dent 1989; 37: 122–124.
McInnes-Ledoux P, Zinck J, Weinberg R, McInnes J . Bond strength of dentine bonding agents to Caridex-treated dentine. Dent Mater 1987; 3: 331–336.
Wolski K, Goldman M, Kronman J H, Nathanson D . Dentinal bonding after chemomechanical caries removal — effect of surface topography. Oper Dent 1989; 14: 87–92.
BDA Background Briefing No. 18 (9 January 1998).
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Yip, H., Stevenson, A. & Beeley, J. Chemomechanical removal of dental caries in deciduous teeth: further studies in vitro. Br Dent J 186, 179–182 (1999). https://doi.org/10.1038/sj.bdj.4800057a1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800057a1
This article is cited by
-
Chemochemical caries removal: a review of the techniques and latest developments
British Dental Journal (2000)
-
Dentine caries excavation: a review of current clinical techniques
British Dental Journal (2000)