Abstract
Apoptosis is a major mechanism of treatment-induced T-cell depletion in leukemia and autoimmune diseases. While ‘classical’ apoptosis is considered to depend on caspase activation, caspase-independent death is increasingly recognized as an alternative pathway. Although the DNA-damaging drug cyclophosphamide (CY) is widely used for therapy of hematological malignancies and autoimmune disorders, the molecular mechanism of apoptosis induction remains largely unknown. Here, we report that treatment of Jurkat, cytotoxic, and primary leukemic T cells with an activated analog of CY, 4-hydroperoxy-cyclophosphamide (4-OOH-CY), induces caspase activation and typical features of apoptosis, although cell death was not prevented by caspase inhibition. Also depletion of murine thymocytes and splenocytes after CY treatment in vivo was not inhibited by Z-Val-Ala-DL-Asp-fluoromethylketone (Z-VAD.fmk). Caspase-8 and receptor-induced protein (RIP) were dispensable for 4-OOH-CY-mediated apoptosis, while overexpression of Bcl-2 was partially protective. 4-OOH-CY treatment induced reactive oxygen species production, upregulation of Bax, and nuclear relocation of the mitochondrial factors apoptosis-inducing factor (AIF) and endonuclease G (EndoG). The antioxidant N-acetyl-L-cysteine substantially inhibited conformational changes of Bax, loss of mitochondrial membrane potential, nuclear relocation of mitochondrial factors, and apoptosis induction in 4-OOH-CY-treated T cells. These results strongly indicate that oxidative damage-induced nuclear translocation of AIF and EndoG in 4-OOH-CY-treated T cells might represent an alternative death pathway in the absence of caspase activity.
Similar content being viewed by others
Main
Self-tolerance and cellular homeostasis are regulated by T-cell apoptosis.1 The extrinsic apoptotic pathway involves triggering of death receptors, which induce the activation of the initiator caspases-8/-10 in the death-inducing signaling complex (DISC) followed by direct cleavage of downstream effector caspases. After activation of the intrinsic mitochondrial pathway, mitochondrial cytochrome c release initiates apoptosome formation and subsequent activation of effector caspases.2 Both pathways are characterized by their dependence on caspases. Recently, mitochondria-mediated, caspase-independent apoptotic pathways were described. Disturbance of the mitochondrial function induces the release of apoptosis-inducing factor (AIF), endonuclease G (EndoG), and HtrA2/Omi, which triggers cell death in the absence of caspase activation.3 Permeabilization of the outer mitochondrial membrane and the release of molecules from the intermembrane space are controlled by molecules of the Bcl-2 family. Proapoptotic molecules such as Bax and Bak serve as pore forming effector molecules, while antiapoptotic molecules such as Bcl-2 and Bcl-xL prevent mitochondrial pore formation.4
The CD95/CD95L system regulates T-cell homeostasis predominantly in a caspase-dependent fashion, since patients with mutations in the CD95-signaling pathway suffer from autoimmunity and lymphoproliferation.5 However, there is increasing evidence for alternative caspase-independent death of T cells during T-cell development and T-cell activation, for example negative thymic selection or CD95-mediated death can also proceed in the absence of caspase activation.6 Two pathways of CD95-mediated death have been described in T cells.7 One pathway involves DISC formation, caspase activation, and subsequent DNA fragmentation, whereas the second pathway takes place in the absence of caspase activation and shows typical features of necrosis. This CD95-induced necrotic cell death reportedly depends on the activation of the kinase RIP (receptor-induced protein).8
The majority of cytotoxic agents activate the mitochondrial pathway, either in a caspase-dependent or -independent fashion.9 Cell death in the absence of caspase activation was, for example, reported from sulfasalazine-treated T cells,10 placlitaxel treatment of ovarian carcinoma cells,11 or safingol-stimulated oral squamous cell carcinomas.12 Death induction by these drugs is considered to involve the nuclear translocation of mitochondrial apoptogenic factors AIF or EndoG. Nuclear relocation of mitochondrial factors is often preceded by drug-mediated induction of reactive oxygen species (ROS) followed by mitochondrial relocalization of Bax and subsequent mitochondrial disintegration.13
Cyclophosphamide (CY), a DNA-damaging agent inducing interstrand DNA cross-links, is used in the treatment of lymphomas and autoimmune diseases.14 CY is a prodrug, which is converted into its active form 4-hydroxy-cyclophosphamide in the liver. Despite its broad clinical use, the molecular mechanisms of CY-induced apoptosis in T cells are only poorly understood. Dependence of the p53 tumor suppressor was reported for CY-induced B-cell lymphoma death in vivo,15 and oxidative DNA damage16 was suggested to be involved in 4-hydroperoxy-cyclophosphamide (4-OOH-CY)-induced apoptosis. In rat thymocytes and splenic T cells from NOD mice, CY-induced apoptosis is mediated by engagement of the CD95 death receptor.17, 18 Other reports suggest a CY-mediated mitochondrial death pathway, based on the observation that Bcl-2 overexpressing tumors are protected from CY-induced apoptosis19 and 4-OOH-CY-treated murine limbs exhibited cytochrome c release and caspase-3 processing.20, 21
In the present study we demonstrate that T-cell apoptosis induced by an activated analog of CY, 4-OOH-CY, proceeds in the absence of caspase activation in vitro in three different model systems, namely in Jurkat T cells, primary human cytotoxic T cells (CTL), and primary leukemic T cells. Also in vivo depletion of murine thymocytes and splenocytes by CY was not inhibited by Z-Val-Ala-DL-Asp-fluoromethylketone (Z-VAD.fmk). 4-OOH-CY-mediated T-cell death was independent of death-receptor activation but activated the mitochondrial death pathway by ROS production and disturbance of the mitochondrial membrane potential (ΔΨm) accompanied by nuclear translocation of the mitochondrial factors AIF and EndoG. These results further support the relevance of caspase-independent death in primary T cells and demonstrate an alternative pathway through which cytotoxic drugs can trigger apoptosis.
Results
4-OOH-CY-induced apoptosis in Jurkat T cells is independent from death receptor signaling and caspase activity
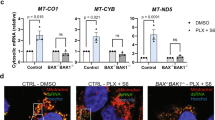
Death receptor signaling or disturbance of mitochondrial integrity has been implicated in apoptosis induced by cytotoxic drugs.9 Since caspase-8 is required for death receptor-transduced apoptosis we analyzed whether caspase-8-deficient Jurkat cells are susceptible to 4-OOH-CY-induced apoptosis. Since CY can only be metabolized in its active form in the liver, the activated analog of CY, 4-OOH-CY, has to be used in cell culture experiments. The parental Jurkat line and Jurkat caspase-8def cells were treated with 4-OOH-CY and apoptosis was measured after 24, 48, and 72 h (Figure 1a). Caspase-8 deficiency prevented CD95-mediated death induced by anti-CD95 monoclonal antibody (mAb) APO-1 in Jurkat cells, while cell death induced by 4-OOH-CY was not inhibited and comparable to death of parental cells. Absence of caspase-8 expression was confirmed by western blot analysis (Figure 1a). Since CD95-mediated necrotic T-cell death was associated with the kinase RIP,8 RIP-deficient Jurkat cells were treated with 4-OOH-CY. RIP deficiency in Jurkat cells was shown by western blot analysis (Figure 1b). Cell death, however, was indistinguishable in RIP-deficient cells and their parental counterparts (Jurkat SVT35) (Figure 1b). While receptor signaling did not contribute to 4-OOH-CY-mediated apoptosis, overexpression of Bcl-2 in Jurkat cells completely inhibited 4-OOH-CY-mediated apoptosis at 4-OOH-CY concentrations of 1 μg/ml (Figure 1c). Inhibition of cell death at higher 4-OOH-CY-concentrations (3 μg/ml) was only partial. Overexpression of Bcl-2 was confirmed by cytoplasmic Bcl-2 staining (Figure 1c).
4-OOH-CY-induced apoptosis is independent of death receptor signaling and caspase activation in Jurkat T cells. (a, b) Caspase-8 or RIP-deficient Jurkat cells and parental Jurkat cells were incubated with 4-OOH-CY (4-CY) (1 or 3 μg/ml) or APO-1 (1 μg/ml) for 24, 48, and 72 h and apoptosis was determined by measurement of hypodiploid DNA content. RIP and caspase-8 deficiency were confirmed by western blot analysis. (c) Jurkat cells overexpressing Bcl-2 and the parental cell line were treated with 1 and 3 μg/ml 4-OOH-CY (4-CY) for 24, 48, and 72 h and apoptosis induction was analyzed by the amount of hypodiploid DNA content. Intracellular staining of Bcl-2 (filled curves) confirmed overexpression of Bcl-2 in J-Bcl-2 cells. Non-filled curves represent staining with isotype-specific antibody. (d) Jurkat cells were incubated for 24 or 48 h with 4-OOH-CY (4-CY) (3 μg/ml) in the absence or presence of Z-VAD.fmk (100 μM). Caspase activation was analyzed fluorometrically by cleavage of caspase substrates DEVD-R110 (caspase-3), IETD-Afc (caspae-8), and LEHD-Afc (caspase-9). (e) Apoptosis induction in the absence (medium) or presence of Z-VAD.fmk (100 μM) was analyzed by measurement of hypodiploid DNA content. Values present the mean of triplicates±S.D. and each experiment was performed three times. At each time point and for all cell lines the spontaneous apoptosis never exceeded 18%
To determine the putative caspase dependence of 4-OOH-CY-mediated apoptosis, Jurkat T cells were exposed to 4-OOH-CY in the presence or absence of the broad-spectrum caspase inhibitor Z-VAD.fmk. After 24 and 48 h of culture, caspase activation was analyzed fluorometrically by assessing the cleavage of caspase-specific substrates (Figure 1d). Weak activation of caspase-8 and -9 was detected upon treatment with 4-OOH-CY, while caspase-3 exhibited pronounced activity. Although caspase activity was fully blocked by Z-VAD.fmk and the caspase inhibitor efficiently inhibited CD95-mediated apoptosis, 4-OOH-CY-induced cell death proceeded independently of caspase inhibition (Figure 1e), indicating that in Jurkat cells 4-OOH-CY-induced apoptosis is death receptor- and caspase-independent.
4-OOH-CY induced caspase-independent apoptosis in human CTL and primary leukemic T cells
Since CY is used in the treatment of leukemia, lymphoma, and autoimmune diseases, we investigated caspase-independent cell death induction in activated, primary, human alloantigen-specific CTL. HLA-A1-specific CTL22 were incubated with increasing concentrations of 4-OOH-CY in the presence or absence of Z-VAD.fmk for 24, 48, and 72 h. In the presence of Z-VAD.fmk, we did not observe a significant inhibition of cell death induction (Figure 2a). Depending on the time point and the 4-OOH-CY concentration used, inhibition of death varies between 0 and 20%, indicating that cell death is largely caspase-independent. For further experiments we chose a 4-OOH-CY concentration of 3 μg/ml. In 4-OOH-CY-treated CTL, Annexin-V positivity preceded the loss of membrane integrity (propidium iodide (PI+) positivity) and changes in cell size and granularity (forward/side scatter (FSC/SSC)) (Figure 2b), indicating that cell death is primarily apoptotic. This was further supported by typical morphological features of apoptosis in 4-OOH-CY-treated CTL such as rounding up of the cell, pyknosis, condensation, and fragmentation of the nucleus and the maintenance of an intact plasma membrane (Figure 2c). Z-VAD.fmk marginally inhibited Annexin-V positivity in 4-OOH-CY-treated cells, while cell death detected by PI+ and FSC/SSC was not inhibited (Figure 2b). To show that Z-VAD.fmk was efficiently taken up and completely inhibited caspase activation in CTL, we incubated non-lysed CTL with the membrane-permeable caspase substrate Z-DEVD-R110, known to be cleaved preferentially by caspase-3, but also with lower efficiency by caspase-6, -7, -8, and -10. Subsequently, caspase activation was analyzed by flow cytometry (Figure 2d). Efficient caspase activation occurred after 24 and 48 h, which was completely inhibited by Z-VAD.fmk. Since CTL express endogenously activated caspases22 the presence of Z-VAD.fmk reduced caspase activation below the medium control. Additionally, apoptosis induction in CTL by etoposide was blocked by about 45% after 72 h by Z-VAD.fmk, showing that caspase dependence of apoptosis varies between different DNA-damaging drugs (Supplementary Figure 1). While Z-VAD.fmk is a strong inhibitor of caspase-1, -3, -5, -7, -8, and -9, caspase-2 activation is only weakly inhibited.23 Therefore, we tested whether 4-OOH-CY-triggered apoptosis induces caspase-2 activation considered to be involved in death induction after DNA damage.24 The presence of the caspase-2-specific inhibitor Z-VDVAD.fmk did not prevent 4-OOH-CY-induced apoptosis in CTL, while etoposide-induced cell death in Jurkat cells, known to be mediated by caspase-2 activation,25 was prevented (Figure 2e). To explore whether 4-OOH-CY-induced cell death requires caspase activation in primary leukemic cells, we treated T-cell acute lymphocytic leukemia (T-ALL) blasts with 4-OOH-CY in the absence or presence of Z-VAD.fmk and analyzed cell death after 48 and 72 h by measuring Annexin-V and PI positivity (Figure 3a). Although Z-VAD.fmk efficiently blocked caspase activity (Figure 3b), cell death was not inhibited (Figure 3a). Taken together, these data demonstrate that 4-OOH-CY-induced cell death does not require caspase activity in primary leukemic T cells and is also predominantly caspase-independent in primary human CTL.
Caspase-independent death of human CTL after 4-OOH-CY treatment. (a) Human HLA-A1-specific CTL were incubated with increasing concentrations of 4-OOH-CY (4-CY) in the absence or presence of Z-VAD.fmk (50 μM) and apoptosis was determined after different time points by measuring Annexin-V positivity. (b) Human HLA-A1-specific CTL were incubated with 4-OOH-CY (4-CY) (3 μg/ml) in the absence or presence of Z-VAD.fmk (50 μM) and apoptosis was determined after different time points by measuring Annexin-V- or PI-positive cells or changes in cell size (FSC/SSC). (c) Human HLA-A1-specific CTL were cultured in the absence (untreated) or presence of 4-OOH-CY (4-CY) (3 μg/ml) for 48 h, followed by analysis of their morphology, either by DAPI-staining (upper row) or by light microscopy (lower row). Representative pictures of two independent experiments, taken with identical camera settings, magnification: × 60. (d) CTL were left untreated or incubated with 4-OOH-CY (4-CY) (3 μg/ml) in the absence or presence of Z-VAD.fmk (50 μM), and caspase activation was analyzed by flow cytometry using the cell-permeable caspase substrate Z-DEVD-R110. (e) CTL were treated with 4-OOH-CY (4-CY) (3 μg/ml) and Jurkat cells were incubated with etoposide (10 μM) in the absence or presence of the caspase-2-specific inhibitor Z-VDVAD.fmk (50 μM) for 24 h. Apoptosis induction was determined by staining Annexin-V-positive cells. Values present the mean of triplicates±S.D. Experiments are representative for three different experiments performed. Spontaneous apoptosis of CTL never exceeded 25% for all experiments performed
4-OOH-CY-mediated apoptosis of T-ALL primary cells does not require caspase activation. (a) T-ALL cells, which have been expanded in NOD/SCID mice, were incubated for 48 and 72 h with 4-OOH-CY (4-CY) (3 μg/ml) in the presence or absence of Z-VAD.fmk (50 μM), and apoptosis induction was determined by staining Annexin-V- and PI-positive cells. (b) Caspase activation was determined by flow cytometry measuring the cleavage of the cell-permeable substrate Z-DEVD-R110 in T-ALL cells either left untreated (medium) or treated with 3 μg/ml 4-OOH-CY (4-CY) in the presence or absence of Z-VAD.fmk (50 μM) at 48 h
Caspase-independent T- and B-cell death in CY-treated mice
CY is employed for the treatment of hematological malignancies and autoimmune disorders.14 We therefore asked whether the native, non-active form of CY, which is metabolized in the liver to 4-hydroxy-cyclophosphamide, also induces caspase-independent death of lymphocytes in vivo. BALB/c mice were injected i.p. with 200 mg/kg CY or i.v. with 10 μg/mouse Jo2 (anti-CD95 mAb). To test caspase dependence of lymphocyte death, two further groups were treated with a combination of CY and Z-VAD.fmk or Jo2 and Z-VAD.fmk. At day 5, the mice were killed and the total number of thymocytes and splenocytes was determined (Table 1). CY-treated mice exhibited a marked depletion of immature double-positive CD4+CD8+ thymocytes and mature single-positive CD4+ and CD8+ T cells, which could not be inhibited by Z-VAD.fmk. Up to 58% of peripheral CD4+ and CD8+ T cells were deleted after CY treatment, and B cells were reduced by 92%. Inhibition of caspase activity by Z-VAD.fmk did not protect against CY-mediated apoptosis of splenocytes. While mice treated with Jo2 died during the first 4 h of treatment, mice receiving Jo2 and Z-VAD.fmk survived, demonstrating that Z-VAD.fmk is functional and can efficiently inhibit caspase-dependent cell death. Cell numbers of single-positive CD4+ and CD8+ thymocytes and splenocytes were slightly increased in Jo2/Z-VAD.fmk-treated animals probably due to protection from spontaneous apoptosis by Z-VAD.fmk. Double-positive CD4+CD8+ thymocytes, however, were only partially protected by Z-VAD.fmk from CD95-mediated apoptosis. Since CD4+CD8+ double-positive thymocytes present the major subpopulation of thymic cells, the total thymocyte number was not completely recovered after Jo2/Z-VAD.fmk treatment. The inability of Z-VAD.fmk to prevent CY-mediated mature lymphocyte death in vivo further supports our in vitro findings.
Upregulation of p53 and Bax in primary CTL after 4-OOH-CY treatment
To clarify the molecular mechanism underlying CY-induced T-cell death, we first analyzed whether functional p53 and p53-induced Bax are upregulated after 4-OOH-CY treatment. Since our CTL cultures consist of CD4+ and CD8+ T-cell subsets, we analyzed both populations separately (Figure 4a). After 24 h, 4-OOH-CY-treated CD4+ and CD8+ T cells exhibited a strong induction of p53 and Bax, which did not substantially increase at later time points. Upregulation of p21 and MDM2 confirmed the transcriptional activity of p53. Apoptosis induction via CD95 receptor triggered by APO-1, however, did not induce p53, p21, MDM2, or Bax. 4-OOH-CY treatment did not alter the expression of Bcl-2. Since CD4+ and CD8+ T cells did not reveal any differences in their response to 4-OOH-CY and the amount of apoptosis was comparable for both populations (data not shown) and resembled the results shown in Figure 2a for unseparated cells, we considered the bulk culture of CTL as a unique population for further experiments. Cotreatment of CTL with 4-OOH-CY and cycloheximide decreased death induction, indicating that de novo protein synthesis was required for 4-OOH-CY-induced death (data not shown). However, Jurkat cells, known to have point mutations in the p53 gene, expressed high endogenous levels of p53 and did not further upregulate p53 after 4-OOH-CY treatment (Supplementary Figure 2), showing that it is unlikely that 4-OOH-CY-mediated apoptosis is entirely p53-dependent in T cells.
4-OOH-CY-mediated apoptosis is associated with p53 upregulation and induced caspase-independent dissipation of ΔΨm in CTL. (a) CD4+ and CD8+ T cells were isolated from HLA-A1-specific CTL bulk culture and treated with 4-OOH-CY (4-CY) (3 μg/ml) for 24, 48, and 72 h or with APO-1 (1 μg/ml) for 24 h. Isolated proteins were subjected to western blot analysis. β-Actin served as loading control and blots are representative for two other experiments performed. (b) HLA-A1-specific CTL were incubated for 48 h in the presence of 4-OOH-CY (4-CY) (3 μg/ml) or for 12 h with APO-1 (1 μg/ml) or medium alone in the absence or presence of Z-VAD.fmk (50 μM), and % ΔΨmlow cells were determined by flow cytometry using DiOC6. Experiments were performed three times with comparable results
Since the insertion of Bax in the outer mitochondrial membrane induces the loss of ΔΨm,26 we examined whether 4-OOH-CY treatment of CTL decreased ΔΨm in a caspase-independent manner. Reduction of ΔΨm was observed after 4-OOH-CY treatment and could not be inhibited by Z-VAD.fmk. Z-VAD.fmk, however, inhibited ΔΨm dissipation in CTL treated with the CD95-specific mAb APO-1 (Figure 4b).
Inhibition of oxidative damage prevents 4-OOH-CY-mediated upregulation of p53, conformational changes of Bax, dissipation of ΔΨm, and apoptosis induction
Since oxidative damage was reported to be involved in 4-OOH-CY-mediated death,16 we incubated CTL with the cell-permeable dye CM-H2DCFDA (5-(and-6-)-chloromethyl-2′,7′-dichlorodihydrofluorescein diacetate, acetyl ester), which fluoresces after cleavage by intracellular esterases and subsequent oxidation. Efficient ROS production was detected 5 h after 4-OOH-CY treatment in CTL (Figure 5a). Since ROS generates 8-oxoguanine, the most frequently occurring mutagenic base modification, we analyzed the generation of 8-oxoguanine in the presence of 4-OOH-CY in CTL using FITC-labeled avidin, which binds directly and specifically to 8-oxoguanine.27 While untreated CTL were only weakly stained by FITC-avidin, the nuclei of 4-OOH-CY-treated CTL exhibited a strong fluorescence showing that ROS production mediates oxidative DNA damage (Figure 5b). N-acetyl-L-cysteine (NAC) is known as an efficient antioxidant and therefore we determined whether 4-OOH-CY-mediated apoptosis in CTL could be inhibited in the presence of NAC. CTL were treated with 4-OOH-CY in the presence and absence of NAC and cell death was determined by Annexin-V positivity. Importantly, CTL exhibited a decrease in cell death of 60% at 24 h, 56% at 48 h, and 35% at 72 h in the presence of NAC (Figure 5c). Comparable to the results shown in Figure 2a, incubation of 4-OOH-CY-treated cells with Z-VAD.fmk shows that cell death is largely caspase-independent and inhibition of 4-OOH-CY-mediated cell death by the combined treatment of Z-VAD.fmk and NAC was not further increased compared to NAC treatment alone. In the presence of NAC, 4-OOH-CY induced ROS production (Figure 5d) and 4-OOH-CY-mediated upregulation of p53 was significantly prevented (Figure 5e) indicating that ROS predominantly acts upstream of p53. Subsequently, we observed an inhibition of Bax translocation from the cytoplasm to the outer mitochondrial membrane in the presence of NAC after 4-OOH-CY treatment. Conformational changes of Bax, detected by conformation-specific antibody, occurred in 33% of the 4-OOH-CY-treated T cells after 48 h and could be significantly inhibited in the presence of NAC (18%) (Figure 5f). Since Bax translocation to the mitochondria induces dissipation of ΔΨm, we could also observe that inhibition of Bax translocation by NAC prevented disruption of ΔΨm (Figure 5g) and Annexin-V positivity (Figure 5h) in 4-OOH-CY-treated CTL. In summary, this set of experiments demonstrates that NAC significantly prevents ROS production, p53 upregulation, Bax-translocation, dissipation of the ΔΨm, and subsequently cell death induction.
Induction of oxidative stress by 4-OOH-CY and inhibition of 4-OOH-CY-mediated CTL apoptosis by NAC. (a) HLA-A1-specific CTL were incubated with the cell-permeable dye CM-H2DCFDA (2.5 μM) and cultured in the absence (medium) or presence of 4-OOH-CY (4-CY, 3 μg/ml) and green fluorescence was measured to detect ROS production after 5 h. (b) HLA-A1-specific CTL were cultured in the absence (medium) or presence of 4-OOH-CY (4-CY) (3 μM) for 6 h. The amount of oxidation-induced DNA damage was detected by fluorescence microscopy, using 8-oxoguanine as a surrogate read-out. Representative pictures of two independent experiments, taken with identical camera settings, magnification: × 40. (c) HLA-A1-specific CTL were incubated with 4-OOH-CY (4-CY) (3 μg/ml) in the absence or presence of Z-VAD.fmk (50 μM) and NAC (30 mM) or a combination of both inhibitors. Apoptosis induction was measured after 24, 48, and 72 h by Annexin-V positivity. Values present the mean of triplicates±S.D. Spontaneous apoptosis of CTL was 8% at 24 h, 16% at 48 h, and 25% at 72 h. (d) HLA-A1-specific CTL were incubated with the cell-permeable dye CM-H2DCFDA (2.5 μM). Subsequently, CTL were incubated with NAC (30 mM) alone, 4-OOH-CY (3 μg/ml) or 4-OOH-CY (3 μg/ml) and NAC (30 mM), and production of ROS was analyzed by flow cytometry. (e) HLA-A1-specific CTL were incubated with 4-OOH-CY (3 μg/ml) in the absence (medium) or presence of NAC (30 mM) and proteins were isolated after 24, 48, and 72 h. Expression of p53 and β-actin was analyzed by western blot. (f–h) HLA-A1-specific CTL were incubated with 4-OOH-CY (4-CY) (3 μg/ml) in the presence or absence of NAC (30 mM), and percentage of Baxhi -expressing cells (f), ΔΨmlow cells (g), and Annexin-V-positive cells (h) was determined by flow cytometry. The experiments shown are representative for three independent experiments performed
4-OOH-CY induces oxidative stress-mediated nuclear localization of mitochondrial factors cytochrome c, AIF, and EndoG in human CTL
To identify the factors inducing caspase-independent 4-OOH-CY-mediated CTL death, we determined the subcellular localization of mitochondrial factors AIF, EndoG, and cytochrome c, all considered to induce caspase-independent death.3, 28 CTL were treated for 36 h with 4-OOH-CY in the presence or absence of Z-VAD.fmk or NAC, and subsequently immunofluorescence analysis was performed (Figure 6a). Since cells either incubated with medium alone or in the presence of Z-VAD.fmk or NAC exhibited no differences, untreated cells represent cells incubated in medium alone. In addition, the percentage of apoptotic cells exhibiting nuclear expression of cytochrome c, AIF, and EndoG was quantified (Figure 6b). 4-OOH-CYinduced apoptosis in about 50% of the treated cells after 36 h (Figure 6c). In 48% of the 4-OOH-CY-treated cells we detected cytochrome c in the nucleus, in 54% EndoG, and in 38% AIF (Figure 6b). Nuclear translocation of cytochrome c was totally blocked in the presence of Z-VAD.fmk and NAC, although cell death was not inhibited by Z-VAD.fmk, indicating that nuclear localization of cytochrome c is dispensable for death induction. While nuclear localization of EndoG and AIF was not significantly inhibited by Z-VAD.fmk, NAC totally prevented AIF relocalization and EndoG relocalization by 50% suggesting that oxidative-damage mediates nuclear translocation of AIF and EndoG after 4-OOH-CY treatment. To prove that AIF and EndoG are mediators of 4-OOH-CY-induced T-cell death we generated a lentiviral vector system to express short hairpin RNA (shRNA) directed against AIF or EndoG.29 Jurkat cells expressing EndoG shRNA showed a decrease in EndoG expression of 20% (Figure 7a) and cells expressing AIF shRNA exhibited a reduction in AIF expression to 50% (Figure 7b). Although downregulation of EndoG was only weak, Jurkat cells exhibited an inhibition of apoptosis induction after 4-OOH-CY treatment of 40% at 1 μg/ml and 32% at 3 μg/ml (Figure 7a). Downregulation of AIF prevented 4-OOH-CY-mediated T-cell apoptosis to 50% at 1 μg/ml and 16% at 3 μg/ml (Figure 7b), confirming that AIF and EndoG both contribute to 4-OOH-CY-induced apoptosis. This was further confirmed in a second cellular system using the preadipocyte cell line SGBS.30 4-OOH-CY-induced apoptosis in SGBS was also largely caspase-independent since z-VAD.fmk did not efficiently block apoptosis induction, while NAC totally prevented cell death (Supplementary Figure 3). Inhibition of EndoG (Figure 7c) and AIF (Figure 7d) expression in SGBS cells efficiently protected from 4-OOH-CY-mediated apoptosis. Since NAC totally prevented ROS production, but 4-OOH-CY-mediated apoptosis was not completely inhibited, there might be currently unidentified factors, including non-oxidative mechanisms, which might additionally participate in 4-OOH-CY-mediated T-cell apoptosis.
4-OOH-CY induced oxidative damage-mediated nuclear localization of AIF, EndoG, and cytochrome c. HLA-A1-specific CTL were treated with 4-OOH-CY (4-CY) (3 μg/ml) for 36 h in the absence or presence of Z-VAD.fmk (50 μM) or NAC (30 mM). AIF, EndoG, and cytochrome c (cyt c) were detected by immunofluorescence staining (a). Nuclear and non-nuclear localization of mitochondrial factors was calculated by counting at least 100 cells (b). Simultaneously, apoptosis induction was determined by FSC/SSC (c). Values in (b) and (c) represent the mean of two independently performed experiments±S.D.
AIF and EndoG are mediators of caspase-independent 4-OOH-CY-induced apoptosis. Jurkat cells (a, b) and SGBS cells (c, d) were stably infected with lentiviral vectors expressing shRNA directed against AIF (shRNA AIF), EndoG (shRNA EndoG), or a scrambled shRNA (shRNA HRS). Downregulation of AIF and EndoG was confirmed by western blot analysis and β-actin served as a loading control. Jurkat cells or serum-starved SGBS cells were treated with 4-OOH-CY (4-CY) and apoptosis induction was measured by Annexin-V positivity after 48 h. Spontaneous apoptosis of all Jurkat lines was maximum 23% and of SGBS lines 25%. Values present the mean of triplicates±S.D. Experiments were performed three times with similar results
Discussion
Apoptotic T-cell death controls cellular homeostasis or is extrinsically induced by pathological stimuli such as cytotoxic drugs.9 Here we addressed the molecular mechanisms of apoptosis induction in T cells by the DNA-damaging drug CY, widely used in the treatment of hematological malignancies and autoimmune diseases. Cytotoxic drugs can mediate apoptosis via the extrinsic death receptor pathway or the intrinsic mitochondrial pathway. Both pathways, however, are closely connected and converge at the downstream caspase cascade finally executing cell death. Since caspase-8 processing activates the extrinsic death pathway and can also initiate the intrinsic death pathway by cleavage of Bid,31 we examined 4-OOH-CY-induced T-cell death in Jurkat cells deficient in caspase-8 expression. However, Jurkat caspase-8def cells were not protected from 4-OOH-CY-induced apoptosis, suggesting a death receptor-independent apoptosis pathway. This is in contrast to reports showing that CY acts via CD95/CD95L interaction.17, 18 Instead, Bcl-2 overexpression partially protected Jurkat cells from 4-OOH-CY-mediated apoptosis, indicating that 4-OOH-CY activates the intrinsic mitochondrial death pathway in the absence of caspase-8. This is in agreement with studies showing cytochrome c release and activation of caspase-3 in 4-OOH-CY-treated murine embryos or limbs20, 21 and the protection of Bcl-2 overexpressing tumors from CY-mediated death.19 Inhibition of 4-OOH-CY-triggered apoptosis in murine limbs, however, was not achieved by a caspase-3-specific inhibitor.21 In agreement with this finding, we observed that lethal response of Jurkat cells and primary human CTL to 4-OOH-CY was only marginally inhibited by the broad caspase inhibitor Z-VAD.fmk. Since CY is used in the treatment of leukemias, we analyzed caspase dependence of 4-OOH-CY-induced death in primary human T-ALL cells, which were previously expanded in NOD/SCID mice.32 Also in T-ALL cells, Z-VAD.fmk could not block 4-OOH-CY-induced T-cell death. Caspase-independent 4-OOH-CY-induced death in vitro was confirmed by in vivo experiments. CY-mediated deletion of murine thymocytes and splenocytes proceeded in the presence of Z-VAD.fmk, while Z-VAD.fmk efficiently blocked the caspase-dependent lethal effect of anti-CD95 injection. Z-VAD.fmk is a competitive and irreversible inhibitor of caspases 1–10 although with variable inactivation rates for the different caspases.23 Functionality and penetrating capacity of Z-VAD.fmk was confirmed in our experiments by the observation that caspase activity in Jurkat cells, in CTL, and in primary leukemic T cells was efficiently blocked by Z-VAD.fmk. However, we cannot formally exclude that so far unknown caspases are activated during 4-OOH-CY-mediated apoptosis, which might not be inhibited by Z-VAD.fmk.
Caspase-independent cell death is considered to be mediated by the release and nuclear translocation of mitochondrial proteins AIF, an NADH oxidoreductase; EndoG, a mitochondrial DNA repair enzyme; HtrA2/Omi, a serine protease; and cytochrome c, a redox-active component of the respiratory chain.3, 28 Mitochondrial membrane permeabilization and the release of molecules from the intermembrane mitochondrial space is under the control of Bcl-2-related family members.4 As shown here, Bcl-2 partially blocked 4-OOH-CY-induced apoptosis in Jurkat cells. Due to the sensitivity of CTL to any transfection method, the effect of BCL-2 overexpression on 4-OOH-treated CTL could not be analyzed. However, we could show that 4-OOH-CY induced p53 and Bax upregulation in CTL suggesting that 4-OOH-CY-mediated CTL apoptosis might be p53-dependent. Dependence on p53 was also reported for CY-induced cell death of B-cell lymphomas in vivo.15 While both primary B- and T cells carrying wild-type p53 showed dependence on p53 in CY-induced death, Jurkat cells, known to have point mutations in the p53 gene, endogenously expressed high levels of p53 and did not further upregulate p53 after 4-OOH-CY treatment (Supplementary Figure 2). However, cells exhibiting p53 mutations might have been adapted to p53-independent death mechanisms. Since CY-induced apoptosis can be induced in p53 wild type and mutant cells, it is unlikely that 4-OOH-CY-mediated apoptosis is entirely p53-dependent. Recent data, however, showed that alkylating DNA damaging drugs such as mechlorethamine hydrochloride (nitrogen mustard) or N-methyl-N′-nitro-N-nitrosoguanidine induce the activation of the DNA repair and protein-modifying enzyme poly(ADP-ribose) polymerase (PARP) in Bax/Bak-deficient mouse embryonic fibroblasts in a p53-, Bax/Bak- and caspase-independent manner.33 However, in primary T cells, PARP inhibitors 3,4-dihydro-5-[4-(1-piperidinyl)butoxyl]-1(2H)-isoquinolinone and 3-aminobenzamide could not prevent 4-OOH-CY-induced cell death (data not shown), but substantial decrease in 4-OOH-CY-induced death was achieved by inhibiting oxidative damage.
ROS are reported to directly activate the mitochondrial permeability transition resulting in ΔΨm loss and the release of proapoptotic molecules such as cytochrome c,34 EndoG, and AIF.13, 35 Experiments using antioxidants further indicate that ROS acts upstream of Bax relocation and mitochondrial depolarization.13 We observed that NAC substantially inhibited ROS production, upregulation of p53, conformational changes of Bax, disruption of the ΔΨm, and cell death induction. Nuclear localization of cytochrome c, AIF, and EndoG was detected in all 4-OOH-CY-treated apoptotic cells. Coincubation with Z-VAD.fmk totally inhibited cytochrome c relocation but had no significant influence on the relocalization of AIF and EndoG. Since Z-VAD.fmk did not prevent 4-OOH-CY-induced apoptosis, nuclear localization of cytochrome c is dispensable for 4-OOH-CY-induced death. However, AIF and EndoG both contribute to 4-OOH-CY-mediated death, since Jurkat and SGBS cells exhibiting decreased expression of AIF or EndoG showed a significant reduction in apoptosis induction. Although nuclear translocation of AIF was totally blocked and reduced to 50% for EndoG in the presence of NAC, apoptosis induction was only prevented in 50% of the 4-OOH-CY-treated cells indicating that others, as yet unidentified factors, including non-oxidative mechanisms, might additionally participate in 4-OOH-CY-mediated T-cell apoptosis. The serine protease HtrA2/Omi also stored in the intermembrane mitochondrial space is known to induce caspase-independent death with necrotic features.36 However, this necrotic-like morphology was not detected in 4-OOH-CY-treated CTL (Figure 2c), suggesting that HtrA2/Omi does not contribute to 4-OOH-CY-mediated death. Furthermore, serine protease inhibitors such as 4-(2-aminoethyl)benzenesulfonyl fluoride and cathepsin G inhibitor I or cysteine protease inhibitors, for example, inhibitors of cathepsin B and L (L-trans-Epoxysuccinyl-Leu-3-methylbutylamide, Z-Phe-DL-Ala-fluoromethylketone), or calpain inhibitor I failed to block apoptosis induction (data not shown), indicating that cysteine and serine proteases are not involved in 4-OOH-CY-mediated T-cell death.
In conclusion, our data show that T cells undergo caspase-independent death by 4-OOH-CY in vitro and no inhibition of CY-mediated apoptosis was observed in vivo by Z-VAD.fmk. Apoptosis is independent from death receptor-triggered cell death but mediated by the mitochondrial apoptotic pathway involving ROS production, p53 upregulation, Bax translocation, disturbance of the ΔΨm, and nuclear relocation of mitochondrial factors AIF and EndoG. These results further support the importance of caspase-independent death in T cells and might help to elucidate the molecular mechanisms of CY-induced T-cell apoptosis during the treatment of leukemias and autoimmune diseases.
Materials and Methods
Cell lines and primary T-cell cultures
T cells were grown in RPMI 1640 medium (Gibco-BRL, UK) supplemented with 10% FCS (CAMBREX, Belgium), 2 mM L-glutamine, and 1 mM sodium pyruvate at 37°C in a humidified atmosphere containing 7.5% CO2. SGBS preadipocytes were cultured in DMEM/Ham's F-12 (1 : 1) containing 33 μM biotin, 17 μM pantothenate, 100 U/ml penicillin G sodium, 100 μg/ml streptomycin sulfate (=basal medium), and 10% FBS. To induced apoptosis in SGBS by 4-OOH-CY, cells were washed twice with PBS and subsequently cultured in serum-free basal medium containing 4 μg/ml 4-OOH-CY. HLA-A1-specific CTL were established as described previously.22 In brief, PBMC from HLA-A1− donors were stimulated weekly with the mitomycin C-treated HLA-A1+ lymphoblastoid cell line (LCL) 721 or the HLA-A1-transfected LCL C1R.A1.37 CTL were used for apoptosis induction after they achieved specific cytotoxicity toward HLA-A1 expressing target cells (tested by standard chromium release assay). CD4+ and CD8+ T cells were isolated from CTL culture after the 4th round of stimulation. CTL were incubated with HP2/6 (anti-CD4) to obtain CD8+ cells or OKT8 (anti-CD8) to isolate CD4+ T cells. Depletion of T cells was carried out with BioMag goat anti-mouse IgG Beads (Paesel+Lorei, Hanau, Germany). Purity of both populations was determined by flow cytometry with CD4-FITC and CD8-FITC mAb on a FACScan cytometer (BD Biosciences, Heidelberg, Germany) and ranged between 95 and 97%. The following Jurkat lines were used: Jurkat (obtained from American Type Culture Collection), Jurkat caspase-8−/−38 Jurkat SVT35, Jurkat RIP−/−39, and Jurkat-Bcl-2.40
Reagents
4-OOH-CY was kindly provided by Baxter Oncology GmbH, Frankfurt am Main, Germany. The manufactures certify that the drug provided is pure and not contaminated by oxidizing species. Etoposide USP 23 was obtained from Alexis (Laeufelingen, Switzerland), NAC from Sigma-Aldrich (Steinheim, Germany), and 4′,6-diamidino-2-phenylindole (DAPI) from Roche Diagnostics (Mannheim, Germany).
Analysis of apoptosis induction
Cell death was determined by measuring FSC/SSC, by quantification of DNA fragmentation or by Annexin-V-FITC staining (Annexin-V-FITC Kit, Bender MedSystems, Vienna, Austria) on a FACScan cytometer (BD Biosciences). Briefly, for quantification of DNA fragmentation cell pellets were washed twice with ice-cold PBS and subsequently resuspended in hypotonic fluorochrome solution (PI 50 mg/ml in 0.1% sodium citrate plus 0.1% Triton X-100; Sigma, Taufkirchen, Germany). The tubes were placed at 4°C in dark, overnight before the flow-cytrometric analysis. Specific apoptosis was calculated according to the formula 100 × (experimental cell death (%)−spontaneous cell death (%))/(100−spontaneous cell death (%)). Caspase activation was inhibited by the addition of Z-VAD.fmk (Bachem, Heidelberg, Germany) or Z-VDVAD.FMK (Sigma-Aldrich).
Fluorometrical analysis of caspase activation
Jurkat T cells were incubated with 4-OOH-CY in the presence or absence of Z-VAD.fmk. After 24 and 48 h caspase activity was analyzed by caspase-8/FLICE fluorometric protease assay kit (BioVision, Palo Alto, CA, USA). Briefly, 1 × 106 cells were resuspended in cell lysis buffer on ice. After 10 min, 2 × reaction buffer containing 10 mM DTT and 50 μM caspase substrates were added and incubated for 1 h at 37°C. Adding PBS instead of caspase substrates served as negative control. The following caspase substrates were used: DEVD-R110 (caspase-3-specific; Roche Diagnostics), IETD-Afc (caspase-8-specific; BioVision), and LEHD-Afc (caspase-9-specific; Bachem). Free R110 or Afc was measured fluorometrically at λ=535 or 505 nm on microplate fluorescence reader (1420 Victor™ Multilabel Counter, Wallac, Germany). Experiments were set up in triplicates. X-fold increase in activity=mean emission caspase substrates/mean emission PBS.
Flow cytometric analysis of ROS production, Δψm, activation of caspases, and intracellular staining of Bax and Bcl-2
To determine ROS production, cells were incubated with 2.5 μM CM-H2DCFDA (Molecular Probes Europe BV, The Netherlands) for 30 min at 37°C. After three washes with PBS, cells were treated with 4-OOH-CY in the presence or absence of NAC and analyzed by flow cytometry after 5 h. To evaluate changes in the mitochondrial transmembrane potential (Δψm), 2 × 106 cells were stained for 15 min at 37°C with 35 nM DiOC6-FITC (MoBiTec, Göttingen, Germany), washed, resuspended in phosphate-buffered saline, and immediately analyzed on a FACScan cytometer. To analyze caspase activation, CTL and leukemic T cells were incubated with a 100 μM solution of the cell membrane-permeable caspase substrate Z-DEVD-R110 (Molecular Probes), which can be cleaved by caspase-3,-6,-7,-8, and -10 for 30 min on 37°C and caspase activation was analyzed on a FACScan cytometer. To detect intracellular Bcl-2 and conformational changes of Bax, cells were fixed in 4% formaldehyde for 10 min at room temperature. Cells were washed and incubated with 1 μg anti-Bax Ab (Cl.3) or anti-Bcl-2 Ab (Cl. Bcl-2/100) (BD Biosciences) in PBS/0.3% saponin (Sigma) for 30 min at 4°C, followed by washing with PBS-1% saponin and subsequent incubation with goat anti-mouse IgG (H+L) F(ab′)2-FITC (Dianova, Hamburg, Germany) in PBS-0.3% saponin for 30 min at 4°C. Cells were washed in PBS-0.1% saponin and resupended in PBS for analysis on a FACScan cytometer.
Western blot analysis
For western blot analysis, cells were lysed for 15 min at 4°C in lysis buffer (Tris/HCl 30 mM, pH 7.5, NaCl 150 mM, Triton X-100 1%, glycerol 10%, PMSF 1 mM, DTT 1 mM). Twenty microgram of lysate was separated on a 10–20% gradient SDS-PAGE and electroblotted onto Hybond ECL nitrocellulose membrane (Amersham Life Science, Braunschweig, Germany). Membranes were blocked in PBS, 5% milk powder, and 0.1% Tween 20. Membranes were stained overnight with the 1st Ab, followed by 1-h incubation with the HRP-conjugated 2nd antibody and signals were detected by enhanced chemo-luminescence (Amersham Bioscience, Freiburg, Germany). The following antibodies were used: Bax (YTH-2D2) (R&D, Wiesbaden, Germany), β-actin (AC-15) (Sigma), Bcl-2 (Bcl-2/100), p21 (SXM30), p53 (DO-7), RIP (G322-2) (BD Biosciences), MDM2 (IF2; Calbiochem, Bad Soden, Germany), caspase-8 (12F5) (Alexis, Grünberg, Germany), AIF (AB16501, Chemicon), EndoG (3035, ProSci), and goat anti-mouse IgG-HRP and goat ant-rabbit IgG-HRP (Santa Cruz Biotechnology, Europe).
Immunofluorescence microscopy
To detect nuclear relocation of mitochondrial apoptogenic factors, 1 × 106 cells were centrifuged on POLY-PREP™ SLIDES (Sigma) and fixed in paraformaldehyde/PBS (4% w/v) for at least 15 min. Following two washes in PBS, cells were permeabilized in 0.5% Triton X-100/PBS solution for 5 min. After several more washes, cells were blocked in 10% FCS/PBS for 1 h and incubated with primary antibody overnight. One hour incubation with secondary FITC-labeled antibody was preceded and followed by 4 × 4 min washes with 10% FCS/PBS. Cells were mounted with Vectashield mounting medium for immunofluorescence (Vector Laboratories) and analyzed using a confocal electron scanning microscope (Leica DM IRB, Solms, Germany). The following antibodies were used: AIF (AB16501, Chemicon), EndoG (3035, ProSci), cytochrome c (G742A, Promega), anti-rabbit IgG-FITC (sc-2012, Santa Cruz Biotechnology), and anti-mouse IgG-F(ab′)2 Flour (AQ127F, Chemicon).
Detection of apoptotic morphology
Cells were collected and fixed as above, followed by 15 min incubation with 1 μg/ml DAPI in methanol at 37°C. Cells were mounted and analyzed using an Olympus AX70 fluorescence microscope (Olympus Deutschland GmbH, Hamburg, Germany).
Fluorescent binding assay for 8-oxoguanosine
Cells were collected, fixed, permeabilized, and blocked as described above. After 1 h incubation with 1 : 100 FITC-avidin (Sigma), cells were washed 4 × 4 min with 10% FCS/PBS and mounted as described above. Cells were analyzed using an Olympus AX70 fluorescence microscope.
Lentivector construction
AIF and EndoG-specific shRNA constructs and scrambled shRNA were cloned into the pENTR™/H1/TO entry vector using the BLOCK-iT Inducible H1 RNAi Entry Vector Kit (Invitrogen, Karlsruhe, Germany) and subsequently transferred into the pLenti4/BLOCK-iT™-DEST expression vector by targeted recombination using BLOCK-iT Inducible H1 Lentiviral RNAi system (Invitrogen) according to manufacture's protocol. The following shRNA sequences were designed as described previously:29 AIF sense, 5′GGATTGTGCTATGGAACATCT 3′; EndoG sense, 5′-GATGGGAAATCCTACGTAAAG-3′; scrambled sense, 5′-GATCATGTAGATACGCTCA-3′; loop, TTCAAGAGA. The pLenti expression constructs were cotransfected with packing plasmids by Lipofectamine™ 2000 (Invitrogen) in the 293FT producer cell line using ViraPower™ Lentiviral Expression Systems (Invitrogen) according to the manufacturer's protocols. Three days after transfection the viral supernatant was harvested, filtered through a 0.45 μM PVDF filter, and stored at −80°C.
Transduction of Jurkat cells with viral supernatant
Jurkat cells were seeded in complete medium in 96-well plates. One hundred microliter of viral supernatant and hexadimethrine bromide (8 μg/ml) was added and plates were centrifuged for 1 h at 32°C and subsequently incubated at 37°C. After 16 h medium was changed and cells were cultured in complete medium containing Zeocin (500 μg/ml) (Invitrogen). Zeocin-resistant cells were tested for downregulation of the appropriate target gene by western blot analysis. Percentage downregulation was calculated with the ImageJ image processing program calculating the ratio of specific protein bands related to the β-actin bands.
CY-induced T-cell depletion in mice
Groups of five female BALB/c mice (Charles River, Sulzfeld, Germany) at the age of 6–8 weeks were injected with CY monohydrate (Sigma) (200 mg/kg, i.p.) or Jo2 (anti-CD95; BD Biosciences) (10 μg/mouse, i.v.). To prevent CD95- or CY-induced cell death by caspase activation, two additional groups of five mice were injected with Z-VAD.fmk (Bachem) along the following protocol: −0.5 h, Z-VAD.fmk (200 μg/mouse, i.p.); 0 h, CY (200 mg/kg, i.p.) or Jo2 (10 μg/mouse, i.v.); +0.5 h, Z-VAD.fmk (200 μg/mouse, i.p.). Z-VAD.fmk injections (200 μg/mouse, i.p.) were given daily for 3 further days. All mice were killed on day 5. Thymocytes and splenocytes were stained with CD4-FITC, CD8α-PCP, and CD19-PE (BD Biosciences) and analyzed on a FACScan cytometer. Animal experiments were approved by the Regierungspräsidium Thübingen, Germany, approval no. 702.
Expansion of T-ALL blasts in NOD/SCID mice
Institutional ethics committee approved collection and the use of human primary leukemia cells. Leukemia samples were obtained from patients of the University Children's Hospital, Ulm, Germany, at bone marrow aspiration for diagnostic purposes, after informed consent was obtained from the child and/or their parents. Mononuclear cells were purified by density centrifugation (Biocoll separating solution; Biochrom AG, Berlin, Germany). Diagnosis of T-cell leukemia was verified by immunophenotypic analysis.
All animal studies were conducted according to guidelines of the Federation of European Laboratory Animal Science Association and were approved by the local government (Regierungspräsidium Tübingen, Germany, approval no. 2003/775). Female NOD/SCID (NOD/LtSz-scid/scid) mice (Charles River) aged 5–8 weeks were housed in a pathogen-free environment. 1–2 × 107 human leukemia cells were injected in the tail vein and mice were regularly monitored for developing disease. At first indication of morbidity (lethargy, ruffled fur, conjunctivitis) or at latest 25 weeks after inoculation, mice were killed and splenocytes were isolated. Mononuclear cells were purified by density centrifugation and engrafted human leukemia cells were either used for cell culture experiments or for retransplantation. Purity of human leukemia cells in the preparations from mouse splenocytes was always more than 90%. Purity was confirmed by flow cytometric analysis after staining cells with PE-conjugated anti-Ly-5 (BD Biosciences) and APC-conjugated antihuman-CD7 (BD, Biosciences).
Abbreviations
- ΔΨm:
-
mitochondrial membrane potential
- 4-OOH-CY:
-
4-hydroperoxy-cyclophosphamide
- AIF:
-
apoptosis-inducing factor
- CM-H2DCFDA:
-
5-(and-6-)-chloromethyl-2′,7′-dichlorodihydrofluorescein diacetate, acetyl ester
- CTL:
-
cytotoxic T cells
- CY:
-
cyclophophamide
- DAPI:
-
4′,6-diamidino-2-phenylindole
- DISC:
-
death-inducing signaling complex
- EndoG:
-
endonuclease G
- FSC/SSC:
-
forward/side scatter
- LCL:
-
lymphoblastoid cell line
- mAb:
-
monoclonal antibody
- NAC:
-
N-acetyl-L-cysteine
- PARP:
-
poly(ADP-ribose) polymerase
- PI:
-
propidium iodide
- RIP:
-
receptor-induced protein
- ROS:
-
reactive oxygen species
- shRNA:
-
short hairpin RNA
- T-ALL:
-
T-cell acute lymphocytic leukemia
- Z-VAD.fmk:
-
Z-Val-Ala-DL-Asp-fluoromethylketone
References
Siegel RM, Chan FK, Chun HJ, Lenardo MJ . The multifaceted role of Fas signaling in immune cell homeostasis and autoimmunity. Nat Immunol 2000; 1: 469–474.
Barnhart BC, Alappat EC, Peter ME . The CD95 type I/type II model. Semin Immunol 2003; 15: 185–193.
Ravagnan L, Roumier T, Kroemer G . Mitochondria, the killer organelles and their weapons. J Cell Physiol 2002; 192: 131–137.
Martinou JC, Green DR . Breaking the mitochondrial barrier. Nat Rev Mol Cell Biol 2001; 2: 63–67.
Bidere N, Su HC, Lenardo MJ . Genetic disorders of programmed cell death in the immune system. Annu Rev Immunol 2006; 24: 321–352.
Matsumura H, Shimizu Y, Ohsawa Y, Kawahara A, Uchiyama Y, Nagata S . Necrotic death pathway in Fas receptor signaling. J Cell Biol 2000; 151: 1247–1256.
Vonarbourg C, Stolzenberg MC, Holzelova E, Fischer A, Deist FL, Rieux-Laucat F . Differential sensitivity of Jurkat and primary T cells to caspase-independent cell death triggered upon Fas stimulation. Eur J Immunol 2002; 32: 2376–2384.
Holler N, Zaru R, Micheau O, Thome M, Attinger A, Valitutti S et al. Fas triggers an alternative, caspase-8-independent cell death pathway using the kinase RIP as effector molecule. Nat Immunol 2000; 1: 489–495.
Debatin KM . Apoptosis pathways in cancer and cancer therapy. Cancer Immunol Immunother 2004; 53: 153–159.
Liptay S, Fulda S, Schanbacher M, Bourteele S, Ferri KF, Kroemer G et al. Molecular mechanisms of sulfasalazine-induced T-cell apoptosis. Br J Pharmacol 2002; 137: 608–620.
Ahn HJ, Kim YS, Kim JU, Han SM, Shin JW, Yang HO . Mechanism of taxol-induced apoptosis in human SKOV3 ovarian carcinoma cells. J Cell Biochem 2004; 91: 1043–1052.
Hamada M, Sumi T, Iwai S, Nakazawa M, Yura Y . Induction of endonuclease G-mediated apopotosis in human oral squamous cell carcinoma cells by protein kinase C inhibitor safingol. Apoptosis 2006; 11: 47–56.
Park MT, Kim MJ, Kang YH, Choi SY, Lee JH, Choi JA et al. Phytosphingosine in combination with ionizing radiation enhances apoptotic cell death in radiation-resistant cancer cells through ROS-dependent and -independent AIF release. Blood 2005; 105: 1724–1733.
Colvin OM . An overview of cyclophosphamide development and clinical applications. Curr Pharm Des 1999; 5: 555–560.
Schmitt CA, Fridman JS, Yang M, Lee S, Baranov E, Hoffman RM et al. A senescence program controlled by p53 and p16INK4a contributes to the outcome of cancer therapy. Cell 2002; 109: 335–346.
Murata M, Suzuki T, Midorikawa K, Oikawa S, Kawanishi S . Oxidative DNA damage induced by a hydroperoxide derivative of cyclophosphamide. Free Radic Biol Med 2004; 37: 793–802.
Wang GJ, Cai L . Relatively low-dose cyclophosphamide is likely to induce apoptotic cell death in rat thymus through Fas/Fas ligand pathway. Mutat Res 1999; 427: 125–133.
Mahiou J, Walter U, Lepault F, Godeau F, Bach JF, Chatenoud L . In vivo blockade of the Fas–Fas ligand pathway inhibits cyclophosphamide-induced diabetes in NOD mice. J Autoimmun 2001; 16: 431–440.
Story MD, Mirkovic N, Hunter N, Meyn RE . Bcl-2 expression correlates with apoptosis induction but not tumor growth delay in transplantable murine lymphomas treated with different chemotherapy drugs. Cancer Chemother Pharmacol 1999; 44: 367–371.
Mirkes PE, Little SA . Cytochrome c release from mitochondria of early postimplantation murine embryos exposed to 4-hydroperoxycyclophosphamide, heat shock, and staurosporine. Toxicol Appl Pharmacol 2000; 162: 197–206.
Huang C, Hales BF . Role of caspases in murine limb bud cell death induced by 4-hydroperoxycyclophosphamide, an activated analog of cyclophosphamide. Teratology 2002; 66: 288–299.
Strauss G, Knape I, Melzner I, Debatin KM . Constitutive caspase activation and impaired death-inducing signaling complex formation in CD95-resistant, long-term activated, antigen-specific T cells. J Immunol 2003; 171: 1172–1182.
Garcia-Calvo M, Peterson EP, Leiting B, Ruel R, Nicholson DW, Thornberry NA . Inhibition of human caspases by peptide-based and macromolecular inhibitors. J Biol Chem 1998; 273: 32608–32613.
Tinel A, Tschopp J . The PIDDosome, a protein complex implicated in activation of caspase-2 in response to genotoxic stress. Science 2004; 304: 843–846.
Robertson JD, Enoksson M, Suomela M, Zhivotovsky B, Orrenius S . Caspase-2 acts upstream of mitochondria to promote cytochrome c release during etoposide-induced apoptosis. J Biol Chem 2002; 277: 29803–29809.
Loeffler M, Kroemer G . The mitochondrion in cell death control: certainties and incognita. Exp Cell Res 2000; 256: 19–26.
Struthers L, Patel R, Clark J, Thomas S . Direct detection of 8-oxodeoxyguanosine and 8-oxoguanine by avidin and its analogues. Anal Biochem 1998; 255: 20–31.
Nur EKA, Gross SR, Pan Z, Balklava Z, Ma J, Liu LF . Nuclear translocation of cytochrome c during apoptosis. J Biol Chem 2004; 279: 24911–24914.
Brummelkamp TR, Bernards R, Agami R . A system for stable expression of short interfering RNAs in mammalian cells. Science 2002; 296: 550–553.
Wabitsch M, Brenner RE, Melzner I, Braun M, Moller P, Heinze E et al. Characterization of a human preadipocyte cell strain with high capacity for adipose differentiation. Int J Obes Relat Metab Disord 2001; 25: 8–15.
Li H, Zhu H, Xu CJ, Yuan J . Cleavage of BID by caspase 8 mediates the mitochondrial damage in the Fas pathway of apoptosis. Cell 1998; 94: 491–501.
Borgmann A, Baldy C, von Stackelberg A, Beyermann B, Fichtner I, Nurnberg P et al. Childhood all blasts retain phenotypic and genotypic characteristics upon long-term serial passage in NOD/SCID mice. Pediatr Hematol Oncol 2000; 17: 635–650.
Zong WX, Ditsworth D, Bauer DE, Wang ZQ, Thompson CB . Alkylating DNA damage stimulates a regulated form of necrotic cell death. Genes Dev 2004; 18: 1272–1282.
Atlante A, Calissano P, Bobba A, Azzariti A, Marra E, Passarella S . Cytochrome c is released from mitochondria in a reactive oxygen species (ROS)-dependent fashion and can operate as a ROS scavenger and as a respiratory substrate in cerebellar neurons undergoing excitotoxic death. J Biol Chem 2000; 275: 37159–37166.
Ishihara Y, Shimamoto N . Involvement of endonuclease G in nucleosomal DNA fragmentation under sustained endogenous oxidative stress. J Biol Chem 2006; 281: 6726–6733.
Suzuki Y, Imai Y, Nakayama H, Takahashi K, Takio K, Takahashi R . A serine protease, HtrA2, is released from the mitochondria and interacts with XIAP, inducing cell death. Mol Cell 2001; 8: 613–621.
Strauss G, Osen W, Debatin KM . Induction of apoptosis and modulation of activation and effector function in T cells by immunosuppressive drugs. Clin Exp Immunol 2002; 128: 255–266.
Juo P, Kuo CJ, Yuan J, Blenis J . Essential requirement for caspase-8/FLICE in the initiation of the Fas-induced apoptotic cascade. Curr Biol 1998; 8: 1001–1008.
Ting AT, Pimentel-Muinos FX, Seed B . RIP mediates tumor necrosis factor receptor 1 activation of NF-kappaB but not Fas/APO-1-initiated apoptosis. EMBO J 1996; 15: 6189–6196.
Scaffidi C, Fulda S, Srinivasan A, Friesen C, Li F, Tomaselli KJ et al. Two CD95 (APO-1/Fas) signaling pathways. EMBO J 1998; 17: 1675–1687.
Acknowledgements
We thank B Seed for provision of the RIP-deficient Jurkat line and Baxter Oncology GmbH, Frankfurt am Main, Germany, for supplying 4-hydroperoxy-cyclophosphamide, and Ingrid Knape for excellent technical assistance. This work was supported by grants from EU and DFG (K-MD and SF) and EU, LNC, ANRS, FF, EU, and the French Ministry of Science (GK). NV receives a fellowship from ARC.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by SH Kaufmann
Supplementary Information accompanies the paper on Cell Death and Differentiation website (http://www.nature.com/cdd)
Supplementary information
Rights and permissions
About this article
Cite this article
Strauss, G., Westhoff, MA., Fischer-Posovszky, P. et al. 4-hydroperoxy-cyclophosphamide mediates caspase-independent T-cell apoptosis involving oxidative stress-induced nuclear relocation of mitochondrial apoptogenic factors AIF and EndoG. Cell Death Differ 15, 332–343 (2008). https://doi.org/10.1038/sj.cdd.4402272
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4402272
Keywords
This article is cited by
-
An ex vivo organ culture screening model revealed that low temperature conditions prevent side effects of anticancer drugs
Scientific Reports (2022)
-
Effects of Green cardamom (Elettaria cardamomum Maton) and its combination with cyclophosphamide on Ehrlich solid tumors
BMC Complementary Medicine and Therapies (2021)
-
p53 induction and cell viability modulation by genotoxic individual chemicals and mixtures
Environmental Science and Pollution Research (2018)
-
White light augments chemotherapeutic potential of cyclophosphamide: an in vitro study
BioMetals (2013)
-
Role of Bcl-2 family proteins and caspases in the regulation of apoptosis
Molecular and Cellular Biochemistry (2011)