Abstract
Neural precursor cells (NPCs) are markedly sensitive to apoptotic insults. p53-dependent transcriptional activation of proapoptotic genes has been hypothesized to regulate NPC death in response to DNA damage. Recent studies of non-NPCs have also indicated that p53 may directly interact with Bcl-2 molecules and thereby regulate death independently of transcription. The contribution of transcription-independent p53 activation in NPC death has not been characterized. In this study, we found that apoptosis caused by chemotherapeutic agents in NPCs required p53 expression and new macromolecular synthesis. In contrast, NPC death induced by staurosporine, a broad kinase inhibitor, is regulated by p53 in the absence of macromolecular synthesis. The apoptosis effector molecules Bax and Bak, Apaf-1, and caspase-9 were shown to be downstream of p53 in both pathways. These findings indicate that p53 is in a unique position to regulate at least two distinct signaling portals that activate the intrinsic apoptotic death pathway in NPCs.
Similar content being viewed by others
Introduction
Neural precursor cells (NPCs) are operationally defined as multipotent neural stem cells and mitotically active lineage-restricted neural progenitor cells.1 NPCs reside in the telencephalic ventricular zone and ganglionic eminences of the embryonic forebrain and the external granule cell layer of the neonatal cerebellum and play a critical role in normal brain development.2
Injury to the developing brain has serious consequences for brain morphogenesis and function.3 NPCs are exquisitely sensitive to DNA damage and undergo apoptosis following genotoxic insult. DNA damage-induced death is regulated by multidomain members of the Bcl-2 family, caspases, and components of the intrinsic mitochondrial apoptotic pathway.4, 5 In vivo, genotoxic injury causes the activation of caspase-9 and -3, and produces extensive apoptotic death of NPCs in embryonic day 13 (E13) mice.6, 7, 8, 9 These pathological changes are also seen in freshly isolated NPCs treated ex vivo with genotoxic agents.10 Bax and Bak are known to regulate entry into apoptosis in NPCs,11 but the molecules positioned upstream of Bax and Bak have not been as well characterized, and it is unclear how the intrinsic pathway is activated in NPCs.
In many cell types, genotoxic stress leads to both cell cycle arrest and apoptosis that is regulated by the tumor suppressor protein p53.12, 13 p53 is highly expressed in NPCs,14 and p53-deficient NPCs show dramatically reduced caspase-3 activation and cell death following exposure to cytosine arabinoside (AraC) or γ-irradiation.7 The precise mechanism of p53 action in NPCs exposed to genotoxic injury is incompletely defined, but may require p53-dependent transcription of proapoptotic BH3-domain-only molecules, such as Noxa and PUMA.15, 16 In addition to having transcription-dependent functions, p53 may have a transcription-independent role in regulating apoptosis.17 Several reports have described a novel role for p53 protein in activating the intrinsic apoptotic pathway.18, 19, 20 It is unclear whether a p53-dependent, transcription-independent apoptotic pathway exists in NPCs.
To better define the role of p53 and other apoptosis-associated molecules in regulating NPC apoptosis, we characterized the death responses, caspase-3 activation, and genetic requirements for NPC apoptosis following exposure to several DNA-damaging agents and staurosporine (STS), a broad kinase inhibitor and potent apoptosis inducer.21 Using NPCs prepared from mice with gene disruptions of p53, bax and bak, apaf-1, or caspase-9, we investigated whether the molecular requirements for STS-induced death were similar to the requirements for genotoxic injury-induced death. Our results indicate that specific death stimuli activate selective upstream signaling molecules that converge at the level of p53, which leads to Bax/Bak-dependent caspase activation and NPC death through either transcription-dependent or -independent mechanisms. Taken together, we conclude that p53 activates the intrinsic apoptotic pathway in NPCs through at least two different mechanisms.
Results
NPCs exhibit caspase activation and die after DNA damage or exposure to STS
Our previous studies on freshly isolated NPCs determined that these cells are sensitive to several forms of genotoxic injury, including exposure to AraC, etoposide, ethylnitrosourea, or γ-irradiation.7, 8, 10 Here, we used mitogenically expanded telencephalic NPCs in order to make mechanistic studies of NPC death more feasible. Primary telencephalic cells were isolated from E13 mice and incubated in a chemically defined, serum-free medium containing fibroblast growth factor-2 (FGF2) (see Materials and Methods). FGF2-expanded NPCs retain immunoreactivity for nestin, an intermediate filament expressed in neural progenitors (97.7±1.6% positive cells, n=3 wells). In addition, FGF2-expanded NPC cultures contained only very rare NeuN-immunoreactive (0.25±0.1%, n=3 wells) or GFAP-immunoreactive (0.70±0.5%, n=4 wells) cells, markers for mature neurons or astrocytes, respectively.
An assessment of baseline cell proliferation in our experimental system is important because DNA damage can induce both cell cycle arrest and cell death,12, 13 and thus decreased viability in response to cytotoxic injury may result from cell cycle arrest rather than cell death. To determine the extent of cell proliferation that occurs during the experimental period, we assessed the cell viability of untreated NPCs at 0, 6, and 24 h. Our viability assay detected a 2.57±4.4% increase in cell number over 6 h and an 11.1±2.1% increase over 24 h (n=8 wells from three independent experiments; additional data not shown). These results demonstrate that the magnitude of cell proliferation is relatively small during our drug treatment periods, accounting for less than a 15% increase in cell number over a 24 h period.
Previous reports showed that exposure to the nucleoside analog AraC induces caspase-dependent cell death in freshly isolated NPCs.7, 8, 10, 22 We confirmed that FGF2-expanded NPCs are also sensitive to AraC in a concentration and time-dependent manner (Figure 1a and data not shown). To determine whether other genotoxic agents that produce different forms of DNA damage induce similar responses, we exposed FGF2-expanded NPCs to the chemotherapeutic agents bleomycin, etoposide, or camptothecin. Bleomycin sulfate, a streptomyces product, causes single- and double-stranded DNA breaks.23 Etoposide forms complexes with DNA topoisomerase and also induces single- and double-stranded DNA breaks.24 Camptothecin binds to DNA–topoisomerase complexes and produces DNA breaks.25 We determined that these agents also potently induced cell death in NPCs (Figure 1b and c, and data not shown). These results demonstrate that FGF2-expanded NPCs have a conserved sensitivity to a number of genotoxic agents with different mechanisms of action.
Exposure to genotoxic agents or STS induces cell death in FGF2-expanded NPCs. Exposure to 24 h AraC (a), 36 h bleomycin (b), or 24 h camptothecin (c) produces a significant decrease in cell viability in a concentration-dependent manner. Similar results are seen following 24 h etoposide exposure (data not shown). Exposure to STS for 6 h also reduces cell viability in a concentration-dependent manner (d). Cell viability is normalized to untreated control (UT). Data points represent mean±S.E.M. with n=8. (*P<0.001 by one-way ANOVA/Bonferroni post-test versus UT)
We have previously reported that freshly isolated telencephalic NPCs were responsive to the death-inducing effects of STS; however, the specific molecules regulating this response were not investigated.10 NPC-derived cell lines that lack Apaf-1 are protected from STS-induced death,26 suggesting that the intrinsic pathway may be activated by this agent. To confirm and extend these findings, we exposed FGF2-expanded NPCs to increasing concentrations of STS and detected a significant decrease in cell viability following 6 h (Figure 1d). Although this result demonstrates that STS can induce death of NPCs, it does not indicate whether FGF2-expanded NPCs die via an apoptotic pathway following this stimulus. Immunocytochemical staining for the cleaved p17 fragment of caspase-3 is a useful marker for apoptosis, both in vivo and in vitro, following a number of death-inducing insults.27 To determine whether STS induced apoptosis in FGF2-expanded NPCs, we treated FGF2-expanded NPCs with STS for 6 h, fixed them with 4% paraformaldehyde, and assessed the appearance of cleaved ‘activated’ caspase-3 immunoreactivity and apoptotic nuclear features. For untreated NPCs, media were replaced at the onset of treatment and cells were fixed 6 h later. As shown in Figure 2a, untreated NPCs show few apoptotic nuclei and only rare cells with activated caspase-3-like immunoreactivity (1.4±1.2%, n=3 wells). After treatment with 3 μM AraC, numerous apoptotic nuclei were observed and there was a significant increase in the number of cells displaying activated caspase-3 immunoreactivity (at 3 h, 5.0±2.0%; at 6 h, 9.2±1.8%; n=3 wells each time point) (Figure 2b and c). Similar results were seen after exposure to bleomycin, etoposide, or camptothecin (data not shown). Treatment with STS caused marked increases in NPCs with apoptotic features and activated caspase-3-like immunoreactivity (at 3 h, 7.9±1.2%; at 6 h, 14.5±3.4%; n=3 wells) (Figure 2d and e). Quantitation of activated caspase-3 immunoreactivity is shown in Figure 2f. To verify these immunocytochemical observations, we measured the cleaved p17 fragment of caspase-3 by Western blot. NPCs were treated with AraC, bleomycin, or STS for 12 h and protein lysates were prepared. Using the activated caspase-3 antibody (see Materials and Methods), we detected increased levels of the 17 kDa band by Western blot after all treatments (Figure 3a). In total, these results indicate that STS induces caspase-3 activation and apoptotic death in NPCs,26 as it does in other cell types.
Both genotoxic injury and STS exposure induce caspase-3 activation in NPCs. (a) In untreated NPCs, only rare activated caspase-3 immunoreactive cells can be detected by immunocytochemical labeling of the cleaved p17 fragment of caspase-3. (b) After 3 h exposure to 3 μM AraC, increased cleaved caspase-3 immunoreactivity (IR) can be detected in NPCs (red; positive cells indicated by arrows). (c) This effect increases after 6 h of exposure to 3 μM AraC. (d) Similarly, 3 h exposure to 0.5 μM STS also induces increased activated caspase-3 IR. (e) A 6 h exposure to 0.5 μM STS induces widespread cleaved caspase-3 IR. All preparations are counterstained with bisbenzimide to label nuclei (blue). Scale bar=100 μm. (f) Quantitation of the number of activated caspase-3 immunoreactive cells from cultures corresponding to panels (a–e). (*P<0.0005 by one-tailed t-test versus UT)
Biochemical detection of caspase-3 cleavage following either DNA damage or exposure to STS. (a) Exposure to either AraC, bleomycin (BLM), or STS for 12 h induces cleavage of caspase-3 as detected by Western blot. β-Tubulin indicated as loading control. (b) AraC and (c) STS induce significant enzymatic cleavage of DEVD-AMC, a synthetic caspase-3 substrate, in a concentration-dependent manner. Similar results are seen after exposure to bleomycin, camptothecin, or etoposide (data not shown). Caspase-3 activity is normalized to untreated control (UT). Data points represent mean±S.E.M. with n=8. (*P<0.001 by one-way ANOVA/Bonferroni post-test versus UT)
To complement our immunocytochemical and Western blot studies, we measured the in vitro enzymatic cleavage of DEVD-7-amino-4-methylcoumarin (AMC), a fluorogenic caspase-3 substrate. We found that increasing concentrations of AraC caused a significant increase in DEVD-AMC cleavage after 24 h of exposure (Figure 3b). Significant DEVD-AMC cleavage could be detected as early as 6 h after exposure (data not shown). Similarly, exposure to bleomycin, camptothecin, or etoposide increased DEVD-AMC cleavage in a time- and concentration-dependent manner (data not shown). We also determined that STS exposure caused a significant concentration-dependent increase in DEVD-AMC cleavage within 6 h of exposure (Figure 3c). The induction of DEVD-AMC cleavage following STS exposure occurred within 3 h (data not shown). These results indicate that STS produces an apoptotic cell death that shares downstream features of DNA damage-induced death, namely significant caspase-3 activation. Furthermore, the more rapid and robust induction of caspase-3 activation in NPCs exposed to STS compared to DNA-damaging agents prompted us to compare the intracellular events activated by these different death stimuli.
Caspase activation via the intrinsic mitochondrial pathway is required for both STS- and DNA damage-induced death in NPCs
To begin to identify the upstream mediators of caspase-3 activation following STS exposure or DNA damage, we first investigated whether caspase activation was required for death in NPCs exposed to these stimuli. We selected the broad caspase inhibitor BOC-aspartyl(Ome)-fluoromethyl ketone (BAF) to test the caspase requirement of STS- and genotoxin-induced NPC death.10 We found that DNA damage-induced NPC death is significantly inhibited by coincubation with 150 μM BAF (Figure 4a). Similarly, 150 μM BAF attenuated STS-induced cell death (Figure 4b), indicating that caspase activation is important for both DNA damage- and STS-induced NPC death.
Pharmacological or genetic caspase inhibition attenuates cell death following either DNA damage or STS exposure. (a) Coincubation with BAF, a broad caspase inhibitor, attenuates AraC-induced cell death in NPCs. (b) Similarly, BAF coincubation attenuates STS-induced cell death in NPCs. (*P<0.001 by two-way ANOVA/Bonferroni post-test versus matched treated group). (c) FGF2-expanded NPCs from mice that are deficient in both Bax and Bak show significantly less cell death in response to either AraC or STS. Bax deficiency alone also significantly attenuates AraC- and STS-induced cell death. Control group includes both bak+/+/bax+/+ and bak+/−/bax+/+ NPCs. (*P<0.001 by two-way ANOVA/Bonferroni post-test compared to control treated group). (d) FGF2-expanded NPCs that lack both Bax and Bak show decreased cell death and caspase-3 activation (additional data not shown) following exposure to genotoxic injury. (*P<0.001 by two-way ANOVA/Bonferroni post-test compared to wild-type treated group). (e) Exposure to STS results in decreased caspase-3 activation and cell death of Bax and Bak double-deficient NPCs. (*P<0.001 by two-way ANOVA/Bonferroni post-test compared to wild-type treated group). At 0.3 and 1.0 μM STS, a significant (#P<0.01, Bonferroni post-test compared to both the wild-type treated group and the knockout-treated group) effect of Bax heterozygosity was seen. All data points represent mean±S.E.M. with n=8. Cell viability is normalized to untreated control (UT). All experiments were repeated two or more times; representative experiments are shown
To further define the molecular pathways regulating STS- and DNA damage-induced death, we analyzed NPCs derived from mice deficient in critical mediators of the intrinsic apoptotic pathway, such as Bax and Bak, Apaf-1, and caspase-9. The proapoptotic molecules Bax and Bak play overlapping functions in the regulation of apoptosis, and it appears that the significance of either molecule is highly dependent on cell type.11, 28, 29, 30 We reasoned that either Bax or Bak might be critical for the activation of the intrinsic apoptotic pathway in NPCs. To test this hypothesis, we crossed mice that were heterozygous for both bax and bak and prepared FGF2-expanded NPCs from E13 embryos. We then compared the death responsiveness of Bax or Bak single-deficient NPCs and Bax and Bak double-deficient NPCs to their littermate control NPCs. We found that Bak deficiency alone did not significantly alter cell death following exposure to AraC or STS (Figure 4c). However, Bax deficiency alone provided significant protection against both AraC- and STS-induced NPC death (Figure 4c). Quantitatively, deficiency of both molecules provided the highest level of protection following either stimulus. We confirmed these results by investigating the effect of Bax expression, in the context of Bak deficiency, on AraC- and STS-induced death. Dual deficiency led to a significant attenuation of death following exposure to multiple concentrations of AraC (Figure 4d). We also found that death following exposure to bleomycin, etoposide, or camptothecin was also attenuated by dual Bax and Bak deficiency (data not shown). Similarly, dual deficiency markedly reduced death following STS exposure (Figure 4e). Interestingly, a gene–dosage effect of Bax was seen for STS-induced NPC death. Dual Bax and Bak deficiency virtually eliminated caspase-3 activation, as measured by DEVD-AMC cleavage, following either stimulus (data not shown). Taken together, our results demonstrate that STS-induced NPC death is regulated by the combined action of Bax and Bak, but that Bax appears to play a more significant role, similar to previous findings for DNA damage.8, 11 Dual Bax- and Bak-deficient NPCs exposed to either AraC or STS have a small decrease in cell viability as compared to untreated NPCs, which may result from cell cycle arrest and/or nonapoptotic death.
Given Bax and Bak involvement in both DNA damage- and STS-induced death, we proposed that deficiency of either caspase-9 or Apaf-1 would also lead to diminished NPC death following treatment with these two stimuli. As expected, AraC-induced death was significantly decreased by deficiency of Apaf-1 (Figure 5a). This protective effect was also seen after exposure to either camptothecin or STS (Figure 5a). We also exposed caspase-9-deficient NPCs to AraC, bleomycin, camptothecin or STS, and found that deficiency of caspase-9 significantly attenuated death (Figure 5b). Caspase-3 activation in caspase-9 or Apaf-1-deficient NPCs was virtually eliminated following exposure to either genotoxic agents or to STS (Figure 5c and data not shown). Thus, disruption of apoptosome formation prevents caspase-3 activation and death in NPCs exposed to DNA damage or to STS. These results suggest that both STS and genotoxic agents engage a common apoptotic pathway downstream of Bax and Bak activation. To investigate the upstream events leading to NPC apoptosis following DNA damage and STS exposure, we focused on p53 as a molecule known to regulate NPC apoptosis.
Apaf-1 and caspase-9 regulate cell death in NPCs following multiple death stimuli. (a) Apaf-1-deficient NPCs exhibit decreased cell death following 24 h AraC exposure as compared to wild-type NPCs. Similarly, exposure to 24 h camptothecin (CMP; n=6), or 6 h STS also induce Apaf-1-dependent cell death. (b) Caspase-9 deficiency decreases cell death following exposure to 24 h AraC, BLM, or CMP, or to 6 h STS in comparison with caspase-9 heterozygous NPCs, which are equivalent to caspase-9 wild-type cells.7 (c) Apaf-1 deficiency markedly attenuates caspase-3 activation after exposure to AraC (24 h), BLM (24 h), CMP (24 h), or STS (6 h). (*P<0.001 by two-way ANOVA/Bonferonni post-test compared to treated wild-type group). All data points represent mean±S.E.M. Cell viability and caspase activation are normalized to untreated control (UT)
p53 plays an essential but distinct role in STS- versus genotoxin-mediated cell death of NPCs
Given the high levels of p53 in NPCs and its central role in AraC-induced NPC death,7, 8 we reasoned that p53 may play a role in STS-induced NPC caspase-3 activation and death. To begin to define the role of p53 in STS-induced NPC death, we exposed p53-deficient FGF2-expanded NPCs to genotoxic agents or STS and determined caspase-3 activation and cell death. p53 deficiency markedly reduced caspase-3 activation and cell death following AraC, bleomycin, or camptothecin exposure (Figure 6a and c). This result is consistent with the hypothesis that p53 is critically required for the induction of apoptosis following genotoxic injury. Interestingly, p53 deficiency also inhibited a significant component of STS-induced caspase-3 activation and cell death over a broad range of STS concentrations (Figure 6b and d). At the highest concentrations of STS tested, p53-independent caspase-3 activation (Figure 6d) and death (Figure 6b) was also observed, indicating that STS may simultaneously activate several death pathways in NPCs. These results indicate that p53, like Bax and Bak and other components of the intrinsic apoptotic pathway, plays a significant role in STS-induced NPC death.
Both STS-induced death and genotoxin-induced death are regulated by p53. (a) Deficiency of p53 markedly inhibits cell death in NPCs following exposure to AraC. At 1 μM AraC, a significant effect of p53 heterozygosity was seen. (#P<0.001, Bonferroni post-test compared to both the wild-type treated group and the knockout treated group). (b) STS-induced death is attenuated by p53 deficiency, similar to that seen with genotoxin-induced death. (*P<0.001 by two-way ANOVA/Bonferroni post-test compared to wild-type treated group). (c and d) p53 deficiency reduces caspase-3 activation following DNA damage or STS exposure. (*P<0.001 by two-way ANOVA/Bonferroni post-test compared to control treated group). Cell viability is normalized to untreated control (UT). Data points represent mean±S.E.M. with n=6 for UT, n=7 for treated groups
Many p53-regulated processes are dependent on transactivation of p53-target genes, synthesis of new mRNA, and new protein translation. If macromolecular synthesis is necessary for DNA damage- or STS-induced apoptosis in NPCs, we hypothesized that general inhibitors of new gene transcription and protein translation would attenuate caspase-3 activation and cell death following apoptotic insult. Actinomycin D, an inhibitor of new gene transcription, binds to double-stranded DNA and disrupts DNA-primed RNA synthesis.31 Cycloheximide (CHX), an inhibitor of new protein translation, disrupts the 80S ribosome interactions with cytosolic mRNA.32 It has been shown that the induction of proapoptotic genes in neuronal cells can be attenuated using 0.1–1.0 μg/ml of actinomycin D or CHX.33 Over a 24 h period, these agents alone cause NPC death in a concentration-dependent manner (data not shown), as is expected since a baseline level of transcription and translation is required for NPC survival. Therefore, we limited drug exposure to 6 h, which by itself did not produce significant caspase cleavage or cell death in FGF2-expanded NPCs (data not shown). In the presence of CHX or actinomycin D, caspase-3 activation was significantly attenuated following exposure to AraC, bleomycin, camptothecin, or etoposide (Figure 7a; additional data not shown). This result indicates that new gene transcription and protein translation are required for the induction of caspase-3 activity within the first 6 h following genotoxic injury and likely, the subsequent NPC death that occurs over the next 24 h. In contrast, CHX or actinomycin D did not alter caspase-3 activation or cell death in NPCs exposed to STS for 6 h (Figure 7b and c). These results are the first in our analysis to demonstrate that DNA damage and STS activate different cell death programs in NPCs.
Inhibitors of new macromolecular synthesis attenuate DNA damage-induced caspase activation in NPCs but do not alter caspase activation or cell death following exposure to STS. (a) CHX, an inhibitor of new protein translation, significantly attenuated caspase-3 activation following 6 h AraC exposure. BAF, a broad-spectrum caspase inhibitor, also prevented caspase activation following genotoxic injury. (*P<0.001 by one-way ANOVA/Bonferroni post-test compared to AraC-alone treated group). Similar results were seen using other genotoxic agents (data not shown). (b) CHX does not alter caspase-3 activation induced by STS. No concentration of CHX significantly inhibited caspase-3 activation following STS treatment, whereas BAF significantly decreased caspase-3 activation (additional data not shown). (c) CHX does not prevent STS-induced cell death. (*P<0.001 by one-way ANOVA/Bonferroni post-test compared to AraC- or STS-alone treated group). Caspase-3 activity is normalized to untreated control (UT). Data points represent mean±S.E.M. with n=8 (AraC experiment) or 6 (STS experiment). Similar results were obtained with actinomycin D, a gene transcription inhibitor (data not shown)
Based on these observations, we hypothesized that STS may induce a p53-dependent apoptotic program in NPCs that was independent of transcription. To test this hypothesis, we measured the upregulation of two p53-regulated genes, the cyclin-dependent kinase inhibitor p21Waf1/Cip1 (p21)13 and the BH3-domain only molecule noxa,16 following exposure to chemotherapeutic agents or to STS. p21 was found to be upregulated following exposure to AraC, bleomycin, camptothecin, and etoposide (Figure 8a). We also detected an upregulation of noxa expression after AraC exposure (Figure 8b), suggesting that p53-regulated transcriptional programs are activated following DNA damage in NPCs. In contrast, no upregulation of these p53-target genes was detected in NPCs exposed to STS (Figure 8a and b). We extended these analyses by measuring noxa expression by real-time RT-PCR. Exposure to DNA-damaging agents induced significant expression of noxa in NPCs (Figure 8c). In contrast, STS exposure did not induce significantly increased noxa expression (Figure 8c). We confirmed that noxa expression in response to DNA damage was dependent on p53 by measuring noxa expression in p53-wild-type, p53-heterozygous, and p53-deficient NPCs exposed to AraC. DNA damage-induced noxa expression was greatly attenuated in p53-deficient NPCs (Figure 8d). Taken together, these experiments demonstrate that p53-dependent transcriptional activity occurs in NPCs exposed to DNA damage. In contrast, p53-dependent transcriptional activity is not induced by STS exposure. Our findings are consistent with the hypothesis that DNA damage stimulates the transactivation of p53-target genes that cause cell cycle arrest and apoptotic cell death, whereas STS acts on p53 in a more direct manner to induce death.
p53-target genes are upregulated by DNA damage but not by exposure to STS. (a) p53-target gene p21 has a low baseline expression in untreated NPCs (UT) by RT-PCR. Significant upregulation of p21 was seen following 6 h exposure to 1 μM AraC, 3 μM BLM, 1 μM CMP, or 1 μM etoposide (ETO). In contrast, 0.5 μM STS exposure for 6 h did not induce p21. Expression of actin or cyclophillin was not changed by treatment. (b) p53-target gene noxa was increased by 6 h 1 μM AraC treatment, but was absent in untreated NPCs and 0.5 μM STS-treated NPCs. (c) Real-time expression of noxa was significantly increased in response to 24 h exposure to 1 μM AraC, 3 μM BLM, 1 μM CMP, or 1 μM ETO. In contrast, 0.5 μM STS exposure for 6 h did not lead to significant noxa expression. The numbers in parentheses below each column indicate the increase in noxa expression relative to UT samples. (d) Expression of noxa dramatically increased in response to 3 μM AraC exposure for 6 h in both wild-type and p53-heterozygous NPCs. In contrast, p53-deficient NPCs did not show increased expression of noxa following this stimulus
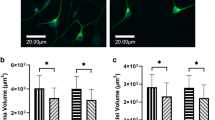
The upregulation of p53-target genes in response to death stimuli is preceded by stabilization of p53 in the nucleus.12 Phosphorylation of p53 by ATM or DNA-PK causes the accumulation of p53 in the nucleus and subsequent activation of p53-target genes (reviewed in Fei and El Deiry13). Therefore, we hypothesized that DNA damage, but not STS, should induce nuclear localization of p53. We detected nuclear p53 immunoreactivity in less than 1% of untreated NPCs at 6 h (0.97±0.9%, n=4 wells) (Figure 9a and f). NPCs treated for 3 h with AraC showed significant p53 immunoreactivity that colocalized with bisbenzimide nuclear staining (25.4±2.0%, n=4 wells) (Figure 9b). The nuclear p53 immunoreactivity persisted for 6 h following AraC exposure (26.2±5.2%, n=4 wells) (Figure 9c). In comparison, STS increased p53 nuclear immunoreactivity in only a small subset of cells (at 3 h, 5.6±5.2%; at 6 h, 4.2±2.3%, n=4 wells) (Figure 9d and e). Summary quantitative data are shown in Figure 9f. These results indicate that the two death stimuli differentially affect p53 in NPCs.
p53 immunoreactivity localizes to the nucleus after exposure to genotoxic injury but not STS. (a) Untreated NPCs show only very low nuclear p53 immunoreactivity (IR) (red). (b) A significant increase in nuclear p53 IR was seen by 3 h exposure to 3 μM AraC. (c) Nuclear p53 IR persisted 6 h after exposure to 3 μM AraC. (d) In contrast, 3 h of 0.5 μM STS exposure is unassociated with significant nuclear p53 IR. (e) Minimal nuclear p53 IR is seen after 6 h 0.5 μM STS exposure. (f) Quantitation of cells with nuclear p53 IR after no treatment (UT), 3 or 6 h of 0.5 μM STS exposure, or 3 or 6 h of 3 μM AraC exposure. (*P<0.0001 by unpaired t-test compared to UT). All preparations are counterstained with bisbenzimide (blue) to indicate nuclear morphology. Scale bar=100 μm
p53 deficiency also protects cerebellar NPCs from DNA damage- and STS-induced death
Our results indicate that p53 has multiple functions in the regulation of apoptosis in telencephalic NPCs. To determine if these death pathways exist in NPCs from other brain regions, we extended our analysis to NPCs derived from the external granule cell layer of the cerebellum. Cerebellar NPCs from wild-type, p53-heterozygous, and p53-deficient mice were isolated, expanded with FGF2, and exposed to either DNA-damaging agents or STS. Similar to telencephalic NPCs, p53-deficient cerebellar NPCs were significantly protected against death following AraC or STS exposure (Figure 10). These results indicate that p53 is an important regulator of cell death across different NPC subpopulations in the developing mammalian nervous system.
p53 regulates cerebellar NPC apoptosis. p53-deficient cerebellar NPCs undergo significantly reduced death following exposure to either AraC or to STS. (*P<0.001 by two-way ANOVA/Bonferroni post-test compared to treated wild-type or heterozygous group). All data points represent mean±S.E.M. with n=8. Cell viability is normalized to untreated control (UT)
Discussion
In this report, we examine and further characterize the role of p53 in regulating entry into the intrinsic mitochondrial death pathway. We focused on neural stem cells as they express relatively high levels of endogenous p53 and little is known about the upstream mediators of intrinsic apoptotic signaling in this important cell type. We show that p53 not only mediates transcription-dependent genotoxic death in NPCs but also has important functions in transcription-independent death produced by STS (Figure 11). Both DNA damage- and STS-induced caspase activation and cell death were markedly reduced by p53 deficiency, providing direct evidence that p53 participates in the apoptotic programs activated by either stimuli. Nuclear p53 localization was greatly increased by DNA damage but not by STS exposure, and in contrast to DNA damage, STS-induced death was not associated with transactivation of p53-target genes. Furthermore, STS-induced caspase-3 activation was not sensitive to inhibitors of new macromolecular synthesis, in contrast to the responses following DNA damage. Finally, we show that disruption of the intrinsic mitochondrial pathway, via either pharmacological or genetic means, significantly abrogates caspase-3 activation and apoptosis in NPCs exposed to either STS or genotoxic injury, an effect that occurs in multiple NPC populations. In total, our results indicate that p53 can activate the intrinsic apoptotic pathway in NPCs by at least two different mechanisms (Figure 11).
Proposed model of p53-dependent apoptotic signaling in NPCs. Both DNA damage and STS exposure induce p53-dependent death in NPCs. However, at the level of p53, the signaling pathway diverges depending on the initiating stimulus. After DNA damage, p53 transactivates p53-inducible genes (PIGs), which subsequently activate Bax and Bak. In contrast, STS exposure activates Bax and Bak through a p53-dependent, transcription-independent pathway. This pathway may involve direct interactions between p53- and mitochondrial-associated proteins. Both stimuli ultimately activate the intrinsic apoptotic pathway and NPC death
NPCs undergo apoptosis during normal development and in response to cytotoxic injury.34 The intrinsic mitochondrial pathway, activated by the proapoptotic molecules Bax and Bak, is critically required for these death programs (reviewed in Akhtar and Roth5). Specifically, in telencephalic NPCs exposed to genotoxic injury, the multidomain pro-apoptotic Bcl-2 family members Bax and Bak mediate the release of mitochondrial cytochrome c into the cytosol. There, cytochrome c forms a complex with procaspase-9 and Apaf-1 called the ‘apoptosome’, which catalyzes the activation of caspase-9 and caspase-3 (reviewed in Akhtar and Roth5). Genotoxic injury-induced caspase-3 activation and apoptosis are markedly reduced in Apaf-1- or caspase-9-deficient NPCs, indicating that caspase-9 activation precedes that of caspase-3 in a linear signaling pathway.7 Bax and Bak double-deficient cells are similarly protected from DNA damage-induced caspase-3 activation and cell death.7, 8 Although caspase-3 is required for the generation of apoptotic features in NPCs, deficiency of caspase-3 does not protect NPCs from genotoxin-induced death,7 indicating that the commitment point to death in NPCs is at the level of caspase-9 activation. In addition, several nongenotoxic apoptotic stimuli, including STS, induce an Apaf-1-dependent death in NPCs,26 indicating the central role for the intrinsic pathway in NPC death regulation.
Little is known about the upstream regulators of this pathway in NPCs. We have previously reported that the tumor suppressor protein p53 and the proapoptotic molecules Bax and Bak are required for DNA damage-induced death in NPCs,7, 8 and we hypothesize that p53-dependent signaling events mediate Bax and Bak activation in NPCs. In proliferating cells such as NPCs, p53-mediated cell cycle arrest and/or apoptosis after irreparable DNA damage inhibits oncogenic transformation.12, 13 NPCs have been proposed to serve as initiating cells for neoplasia.35 Furthermore, mutations in p53 have been associated with several brain neoplasms.12 Apoptotic stimuli lead to the activation of p53 by protein stabilization and post-translational modification.12 Stabilized p53 protein may interact with both pro- and antiapoptotic molecules. In addition, p53 and homologous proteins p63 and p73 regulate the expression of several target genes involved in cell death, both by gene induction and gene suppression.12 We present evidence in this report that p53-regulate NPC death via both transcription-dependent and -independent mechanisms.
P53 may regulate cell death through its physical interaction with Bcl-2 family members. Two alternative models have been proposed for this activity. In irradiated thymocytes, p53 can form inhibitory complexes with Bcl-xL or Bcl-2, ultimately leading to permeabilization of the outer mitochondrial membrane, release of mitochondrial cytochrome c, and apoptosis.18 However, NPCs have minimal Bcl-xL expression,34 suggesting that other molecules must be involved in mediating the effects of p53 in this cell type. Alternatively, p53-mediated proapoptotic activity may be through direct activation of Bax19 or Bak20 at the mitochondria. In this manner, p53 may directly activate the intrinsic apoptotic pathway. As a direct link between apoptotic stimuli and Bax and Bak activation, p53 may serve as a ‘BH3 analog’.17 Here, we present evidence that p53, independent of its regulation of transcriptional events, functions in NPCs in an analogous manner to that described in these reports. To date, no specific p53 post-translational modification has been identified that activates its interaction with Bcl-2 family members or selectively targets p53 to the mitochondria.36
Of the proapoptotic members of the Bcl-2 family, Bax is considered to be the most significant mediator of mitochondria-dependent apoptosis in neurons.29, 30 The contribution of Bak to neuronal apoptosis depends on the cell type and apoptotic stimulus.28 Bax deficiency alone partially protects primary telencephalic NPCs against DNA damage-induced death; however, dual Bax and Bak deficiency provides an even greater protective effect against this apoptotic stimulus.7, 8 In this study, we found that Bax deficiency alone, but not Bak deficiency alone, significantly protected NPCs from either DNA damage- or STS-induced death. However, maximal protection from these death stimuli was observed in NPCs lacking both Bax and Bak, indicating a role for both of these multidomain proapoptotic Bcl-2 molecules in NPCs.
It is clear from a number of studies that the molecular regulation of apoptosis in the nervous system is remarkably cell-type specific. The critical molecules and signaling events for specific apoptotic stimuli may differ between related cell populations. Our results demonstrate that NPCs present in several brain regions are exquisitely sensitive to both STS and DNA damage. Extending our previous studies, we show that a variety of DNA-damaging agents, with differing mechanisms of action, induce a similar apoptotic program in NPCs. The chemotherapeutic agents used in this study cause a variety of molecular insults in DNA, including single- and double-stranded DNA breaks, inhibition of DNA/topoisomerase complex formation, and inhibition of DNA synthesis.22, 23, 24, 25 Given the sensitivity of NPCs from the developing brain to DNA damage, it is likely that NPCs in the adult brain may also be negatively affected by DNA damage. Small pools of NPCs persist in the adolescent and adult hippocampal subgranular and subventricular zones, where they are responsible for ongoing neurogenesis and may contribute to cognitive and behavioral function.2 Although the precise function of adult NPCs is still under investigation, several reports have linked cell death in adult NPCs to disorders of learning and memory, brain tumors, neurodegenerative conditions, and psychiatric disorders.37, 38 The onset of cognitive abnormalities during cancer treatment could arise from dysregulation or death of adult NPCs.39 Adult NPCs do appear to be sensitive to STS,40 indicating that transcription-independent pro-death activity of p53 may be present in multiple populations of NPCs. Interestingly, in certain neuronal populations, STS does not appear to induce a p53- or Bax-dependent apoptosis.30 Like NPCs, SH-SY5Y neuroblastoma cells undergo a transcription-independent death in response to STS that is prevented by inactivation of caspase-9.16 However, STS-induced apoptosis of SH-SY5Y cells is unaffected by p53 inactivation,16 further highlighting the remarkable cell-type specificity of apoptosis regulation.
Our results are the first, to our knowledge, to identify a p53-dependent, transcription-independent pathway of apoptosis in a neural stem cell population. Given the central role NPC apoptosis plays in both normal brain development and in neuropathological conditions, characterization of the signaling events upstream of the intrinsic apoptotic pathway is essential.
Materials and Methods
Chemicals
AraC, camptothecin, bleomycin, etoposide, STS, CHX, and actinomycin D were all purchased from Sigma (St. Louis, MO, USA). BAF was purchased from MP Biomedicals (Aurora, OH, USA).
Mice
Generation of bax−/−, bak−/−, Apaf-1−/−, and caspase-9−/− mice has been described previously (see Akhtar and Roth5). p53+/− mice were purchased from Taconic (Germantown, NY). Endogenous and disrupted genes were detected by PCR analysis of DNA extracts from limb or tail samples as described previously.7 The morning on which a vaginal plug was seen was designated as E0.5. Mice were cared for in accordance with the guidelines of the NIH Guide for the Care and Use of Laboratory Animals. All animal protocols were approved by the Institutional Animal Care and Use Committee of the University of Alabama at Birmingham.
FGF2-expanded NPC cultures
FGF2 has previously been demonstrated to maintain NPCs in an undifferentiated state while serving as a mitotic stimulus for their proliferation.7 As described previously,7 telencephalic and cerebellar NPC cultures were prepared from embryos harvested between gestational days 12 and 13 and from the cerebellum of postnatal day 6 (P6) mice, respectively. Briefly, telencephalic vesicles or cerebellum were isolated and cells were dissociated for 20 min at 37°C in HBSS (Gibco, Grand Island, NY, USA) containing 0.05% trypsin with 0.02% EDTA, 0.001% DNAse I, and 0.2% BSA (all from Sigma). Trypsinization was stopped by adding an equivalent volume of 10% fetal calf serum (FCS) in either HBSS or DMEM (Gibco, Grand Island, NY, USA). Tissue digests were dissociated using several rounds of trituration using a fire-polished Pasteur pipette. Cells were washed once with HBSS containing 0.2% BSA and then resuspended in DMEM containing 20 ng/ml FGF2 (Research Diagnostics Inc., Flanders, NJ), 8 μg/ml heparin, 5 μg/ml insulin, 100 μg/ml apotransferrin, 30 nM sodium selenite, 20 nM progesterone, 100 μM putrescine, 6 g/l glucose, 2 mM glutamine, 94.38 μM 2-mercaptoethanol, 100 U/ml penicillin, and 100 μg/ml streptomycin (all from Sigma), pH 7.4. Cells were incubated at 37°C in humidified 5% CO2/95% air atmosphere. Fresh media were added to cultures every 4 days. Neurospheres were then removed and placed in HBSS containing 0.05% trypsin with 0.02% EDTA, and 0.2% BSA at 37°C for 2 min. Trypsinization was stopped by adding twice the equivalent volume of DMEM containing 10% FCS. Cells were washed with HBSS containing 0.2% BSA and then plated to poly-L-lysine- (Sigma)/laminin- (BD Biosciences, Bedford, MA, USA) coated tissue culture plates (Corning Incorporated, Corning, NY, USA). NPCs formed adherent monolayer cultures and were allowed to continue to grow for 2–4 days. Cells suspensions were prepared by trypsinization as above and plated to poly-L-lysine-/laminin-coated 48-well tissue culture plates (Corning). A small aliquot of cells was stained with Trypan Blue and counted and 30 000 cells were plated per well. Cultures were then incubated for another 2–4 days before being used in experiments. To assess change in viability during the experimental period, parallel cultures of cells were plated to separate tissue culture plates and assayed for cell viability by calcein conversion assay (see below) at the onset of treatment. These viability measurements were compared with the untreated experimental group, and relative change in viability was calculated by (final mean viability−initial mean viability)/initial mean viability.
Cell viability and in vitro caspase cleavage assays
As described previously,8 cells used for viability assay were washed once with Locke's buffer (154 mM NaCl, 5.6 mM KCl, 3.6 mM NaHCO3, 2.3 mM CaCl2, 1.2 mM MgCl2, 5.6 mM glucose, 5 mM HEPES, pH 7.4). Cells were incubated at 37°C for 30 min in Locke's buffer containing 5 μM calcein AM (Molecular Probes, Eugene, OR, USA). Calcein-AM conversion was read using a fluorescence plate reader (excitation 488 nm, emission 530 nm). Cells to be used for immunohistochemistry were fixed in either Bouin's fixative or 4% paraformaldehyde. Caspase activation can be detected with in vitro cleavage assays using AMC-labeled caspase substrates.8 Cells used for in vitro caspase cleavage assay were lysed in 100 μl buffer A (10 mM HEPES, pH 7.4, 42 mM KCl, 5 mM MgCl2, 1 mM DTT, 0.5% CHAPS, 10% sucrose, 1 mM PMSF, and 1 μg/ml leupeptin). Then, 150 μl buffer B (25 mM HEPES, pH 7.4, 1 mM EDTA, 0.1% CHAPS, 10% sucrose, and 3 mM DTT) containing 10 μM DEVD-AMC (Biomol, Plymouth Meeting, PA, USA) was added to cells and the plate was incubated at 37°C for 30 min. Generation of the fluorescent AMC caspase-3 cleavage product was measured using a fluorescence plate reader (excitation 360 nm, emission 460 nm). Both calcein-AM conversion and DEVD-AMC cleavage was expressed relative to untreated controls.
Immunocytochemistry
Fixed NPC cultures were washed in phosphate-buffered saline (PBS) and permeabilized with PBS-blocking buffer (PBS-BB; PBS with 0.1%. BSA, 0.3% Triton X-100, and 0.2% nonfat powdered dry milk) for 30 min at room temperature. Primary antibody was diluted in PBS-BB (without Triton X-100) at the indicated dilutions and applied to permeabilized cells overnight at 4°C. Primary antibodies used were anti-Nestin (Rat-401 mouse monoclonal antibody; Developmental Studies Hybridoma Bank, University of Iowa, Iowa City, IA, USA), anti-GFAP (Z0334 rabbit polyclonal antiserum; Dako Corporation, Carpinteria, CA, USA), anti-NeuN (MAB377; Chemicon, Temecula, CA, USA), anti-p53 (Ncl-p53-Cm5P rabbit polyclonal antiserum; Novocastra Laboratories, Newcastle upon Tyne, UK) and anti-activated caspase-3 (no. 9661 rabbit polyclonal antiserum; Cell Signaling, Beverly MA, USA). Following washes with PBS, plates were incubated with a donkey anti-rabbit or donkey anti-mouse horseradish peroxidase-conjugated secondary antibody (Jackson Immunoresearch, West Grove, PA, USA), diluted in PBS-BB (without Triton X-100) for 1 h at room temperature. Following washes with PBS, immunostaining was detected using a tyramide signal amplification system (Perkin-Elmer Life Science Products, Boston, MA, USA) according to the manufacturer's instructions. Cultures were counterstained with bisbenzimide (2 μg/ml; Hoechst 33 258; Sigma) and examined with a Zeiss-Axiovert microscope equipped with epifluorescence. For quantitation of immunocytochemistry, the fraction of positive cells was counted in four randomly selected microscopic fields. At least three independent wells from different NPC preparations were immunostained and quantitated for each experimental group.
RT-PCR
After treatment, NPC suspensions were prepared by trypsinization as described above. Suspensions were centrifuged and total RNA from the pellets was isolated using Trizol reagent (Invitrogen, Carlsbad, CA, USA) according to manufacturer's instructions. Total RNA (1 μg) was incubated with 200 ng random hexamers, 0.5 mM dNTPs, and RNase-free water at 65°C for 10 min (all from Invitrogen). Then, 5 × first strand buffer, 5 mM DTT, 40 U RNAseOUT, and 200 U SuperScript III was added and the reaction mixture was incubated at room temperature for 5 min, at 50°C for 60 min, at 70°C for 15 min, and at 4°C for 10 min (all reagents from Invitrogen). The absence of genomic DNA contamination was confirmed by actin or cyclophilin PCR of nonenzyme cDNA controls (data not shown). Nonquantitative RT-PCR was performed using Taq DNA polymerase (Invitrogen) according to manufacturer's instructions and the following primers: GTGCCGTTGTCTCTTCG (p21, forward), ACACCAGAGTGCAAGACAGC (p21, reverse); CGCCAGTGAACCCAACGC (noxa, forward), CAAGCGAGCGTTTCTCTCATC (noxa, reverse); GACCTGACAGACTACCTCAT (actin, forward), AGACAGCACTGTGTTGGCAT (actin, reverse); and CAAGACTGAGTGGCTGGATGG (cyclophilin, forward), TAAAATGCCCGCAAGTCAAAGAAA (cyclophilin, reverse). PCR products were run on a 1.5% agarose gel, stained with 0.5 μg/ml ethidium bromide, and photographed. cDNA for quantitative real-time RT-PCR was prepared as described above. Quantitative RT-PCR was performed using TaqMan Gene Expression Assays and the Applied Biosystems 7500 Real Time PCR System (Applied Biosystems, Foster City, CA, USA) according to the manufacturer's instructions. The expression of noxa was normalized to 18S and data were expressed relative to untreated NPCs. Expression studies were performed in the presence of BAF, a broad-spectrum caspase inhibitor, to prolong NPC survival following exposure to apoptotic stimuli.
Western blot
After treatment, NPC suspensions were prepared by trypsinization as described above. Suspensions were centrifuged and pellets were washed twice in ice-cold PBS. Pellets were then re-suspended in lysis buffer containing 25 mM HEPES, 5 mM EDTA, 5 mM MgCl2, 1% SDS, 1% Triton X-100, 1 mM PMSF, 1% protease inhibitor cocktail, and 1% phosphatase inhibitor cocktail (all from Sigma). Cell lysates were sonicated to shear DNA and centrifuged (10 min at 10 000 r.p.m., 4°C). The resultant supernatant was transferred to a fresh microcentrifuge tube. Protein content was assayed using BSA Protein Assay (Pierce) according to the manufacturer's instructions. After boiling for 5 min, equal amounts of protein were resolved in a 12% polyacrylamide gel and transferred to PVDF membrane (0.2 μm pore size; Biorad). After transfer, blots were blocked in 5% milk (blotting grade blocker nonfat dry milk; Biorad) in Tris-buffered saline containing 0.1% Tween 20 (TBS-T) for 1 h at room temperature. Blots were cut at approximately 37 kDa. The upper blot was used for the detection of β-tubulin (no. 9104 rabbit polyclonal antiserum; Santa Cruz Biotechnology, Santa Cruz, CA, USA) and the lower blot was used for the detection of active caspase-3 (no. 9661 rabbit polyclonal antiserum; Cell Signaling, Beverly, MA, USA). Primary antibody was diluted in 5% milk and blots were incubated in primary antibody overnight at 4°C. Blots were then washed with TBS-T and incubated with goat anti-rabbit horseradish peroxidase-conjugated IgG secondary antibody (Biorad) at room temperature for 1 h. Signal was detected using SuperSignal West Femto Maximum Sensitivity Substrate (Pierce) or ECL Western Blotting Detection Reagent (Amersham).
Statistics
All data points represent mean±S.E.M. N=8 for all experiments, unless stated otherwise. All experiments were repeated three or more times; representative experiments are shown. Statistical significance was established by one- or two-way ANOVA followed by Bonferroni's test for all pairwise comparisons.
Abbreviations
- AraC:
-
cytosine arabinoside
- BAF:
-
BOC-aspartyl(Ome)-fluoromethyl ketone
- CHX:
-
cycloheximide
- NPC:
-
neural precursor cell
- STS:
-
staurosporine
References
Rao MS (1999) Multipotent and restricted precursors in the central nervous system. Anat. Rec. (New Anat). 257: 137–148.
Temple S (2001) The development of neural stem cells. Nature 414: 112–117.
Roth KA and D'Sa C (2001) Apoptosis and brain development. Ment. Retard. Dev. Disabil. Res. Rev. 7: 261–266.
Akhtar RS, Ness JM and Roth KA (2004) Bcl-2 family regulation of neuronal development and neurodegeneration. Biochim. Biophys. Acta 1644: 189–203.
Akhtar RS and Roth KA (2006) Regulation of neural stem cell death. In Neural. Development and Stem Cells, Rao MS (ed) (Totowa NJ: Humana Press) pp. 97–122.
Lee Y, Chong MJ and McKinnon PJ (2001) Ataxia telangiectasia mutated-dependent apoptosis after genotoxic stress in the developing nervous system is determined by cellular differentiation status. J. Neurosci. 21: 6687–6693.
D'Sa-Eipper C, Leonard JR, Putcha G, Zheng TS, Flavell RA, Rakic P, Kuida K and Roth KA (2001) DNA damage-induced neural precursor cell apoptosis requires p53 and caspase 9 but neither Bax nor caspase 3. Development 128: 137–146.
D'Sa C, Klocke BJ, Cecconi F, Lindsten T, Thompson CB, Korsmeyer SJ, Flavell RA and Roth KA (2003) Caspase regulation of genotoxin-induced neural precursor cell death. J. Neurosci. Res. 74: 435–445.
Semont A, Nowak EB, Silva LC, Mathieu C, Mouthon MA, May E, Allemand I, Millet P and Boussin FD (2004) Involvement of p53 and Fas/CD95 in murine neural progenitor cell response to ionizing irradiation. Oncogene 23: 8497–8508.
D'Sa-Eipper C and Roth KA (2000) Caspase regulation of neuronal progenitor cell apoptosis. Dev. Neurosci. 22: 116–124.
Lindsten T, Golden JA, Zong WX, Minarcik J, Harris MH and Thompson CB (2003) The proapoptotic activities of Bax and Bak limit the size of the neural stem cell pool. J. Neurosci. 23: 11112–11119.
Vousden KH and Lu X (2002) Live or let die: the cell's response to p53. Nat. Rev. Cancer 2: 594–604.
Fei P and El Deiry WS (2003) P53 and radiation responses. Oncogene 22: 5774–5783.
van Lookeren CM and Gill R (1998) Tumor-suppressor p53 is expressed in proliferating and newly formed neurons of the embryonic and postnatal rat brain: comparison with expression of the cell cycle regulators p21Waf1/Cip1, p27Kip1, p57Kip2, p16Ink4a, cyclin G1, and the proto-oncogene Bax. J. Comp. Neurol. 397: 181–198.
Jeffers JR, Parganas E, Lee Y, Yang C, Wang J, Brennan J, MacLean KH, Han J, Chittenden T, Ihle JN, McKinnon PJ, Cleveland JL and Zambetti GP (2003) Puma is an essential mediator of p53-dependent and -independent apoptotic pathways. Cancer Cell 4: 321–328.
Yakovlev AG, Di Giovanni S, Wang G, Liu W, Stoica B and Faden AI (2004) BOK and NOXA are essential mediators of p53-dependent apoptosis. J. Biol. Chem. 279: 28367–28374.
Chipuk JE and Green DR (2004) Cytoplasmic p53: bax and forward. Cell Cycle 3: 429–431.
Mihara M, Erster S, Zaika A, Petrenko O, Chittenden T, Pancoska P and Moll UM (2003) p53 has a direct apoptogenic role at the mitochondria. Mol. Cell 11: 577–590.
Chipuk JE, Kuwana T, Bouchier-Hayes L, Droin NM, Newmeyer DD, Schuler M and Green DR (2004) Direct activation of Bax by p53 mediates mitochondrial membrane permeabilization and apoptosis. Science 303: 1010–1014.
Leu JI, Dumont P, Hafey M, Murphy ME and George DL (2004) Mitochondrial p53 activates Bak and causes disruption of a Bak-Mcl1 complex. Nat. Cell Biol. 6: 443–450.
Hao Z, Duncan GS, Chang CC, Elia A, Fang M, Wakeham A, Okada H, Calzascia T, Jang Y, You-Ten A, Yeh WC, Ohashi P, Wang X and Mak TW (2005) Specific ablation of the apoptotic functions of cytochrome C reveals a differential requirement for cytochrome C and Apaf-1 in apoptosis. Cell 121: 579–591.
Grant S (1998) AraC: cellular and molecular pharmacology. Adv. Cancer Res. 72: 197–233.
Burger RM (1998) Cleavage of nucleic acids by beomycin. Chem. Rev. 98: 1153–1169.
Hande KR (1998) Etoposide: four decades of development of a topoisomerase II inhibitor. Eur. J. Cancer 34: 1514–1521.
Liu LF, Desai SD, Li TK, Mao Y, Sun M and Sim SP (2000) Mechanism of action of camptothecin. Ann. NY Acad. Sci. 922: 1–10.
Cozzolino M, Ferraro E, Ferri A, Rigamonti D, Quondamatteo F, Ding H, Xu ZS, Ferrari F, Angelini DF, Rotilio G, Cattaneo E, Carri MT and Cecconi F (2004) Apoptosome inactivation rescues proneural and neural cells from neurodegeneration. Cell Death Differ. 11: 1179–1191.
Srinivasan A, Roth KA, Sayers RO, Shindler KS, Wong AM, Fritz LC and Tomaselli KJ (1998) In situ immunodetection of activated caspase-3 in apoptotic neurons in the developing nervous system. Cell Death Differ. 5: 1004–1016.
Sun YF, Yu LY, Saarma M, Timmusk T and Arumae U (2001) Neuron-specific Bcl-2 homology 3 domain-only splice variant of Bak is anti-apoptotic in neurons, but pro-apoptotic in non-neuronal cells. J. Biol. Chem. 276: 16240–16247.
Xiang H, Kinoshita Y, Knudson CM, Korsmeyer SJ, Schwartzkroin PA and Morrison RS (1998) Bax involvement in p53-mediated neuronal cell death. J. Neurosci. 18: 1363–1373.
Johnson MD, Xiang H, London S, Kinoshita Y, Knudson M, Mayberg M, Korsmeyer SJ and Morrison RS (1998) Evidence for involvement of Bax and p53, but not caspases, in radiation-induced cell death of cultured postnatal hippocampal neurons. J. Neurosci. Res. 54: 721–733.
Sobell HM (1985) Actinomycin and DNA transcription. Proc. Natl. Acad. Sci. USA 82: 5328–5331.
Setkov NA, Kazakov VN, Rosenwald IB, Makarova GF and Epifanova OI (1992) Protein synthesis inhibitors, like growth factors, may render resting 3T3 cells competent for DNA synthesis: a radioautographic and cell fusion study. Cell Prolif. 25: 181–191.
Putcha GV, Moulder KL, Golden JP, Bouillet P, Adams JA, Strasser A and Johnson EM (2001) Induction of BIM, a proapoptotic BH3-only BCL-2 family member, is critical for neuronal apoptosis. Neuron 29: 615–628.
Roth KA, Kuan C, Haydar TF, D'Sa-Eipper C, Shindler KS, Zheng TS, Kuida K, Flavell RA and Rakic P (2000) Epistatic and independent functions of caspase-3 and Bcl-X(L) in developmental programmed cell death. Proc. Natl. Acad. Sci. USA 97: 466–471.
Chen D, Livne-Bar I, Vanderluit JL, Slack RS, Agochiya M and Bremner R (2004) Cell-specific effects of RB or RB/p107 loss on retinal development implicate an intrinsically death-resistant cell-of-origin in retinoblastoma. Cancer Cell 5: 539–551.
Erster S and Moll UM (2005) Stress-induced p53 runs a transcription-independent death program. Biochem. Biophys. Res. Commun. 331: 843–850.
Monje ML, Mizumatsu S, Fike JR and Palmer TD (2002) Irradiation induces neural precursor-cell dysfunction. Nat. Med. 8: 955–962.
Amano T, Inamura T, Wu CM, Kura S, Nakamizo A, Inoha S, Miyazono M and Ikezaki K (2002) Effects of single low dose irradiation on subventricular zone cells in juvenile rat brain. Neurol. Res. 24: 809–816.
Rola R, Raber J, Rizk A, Otsuka S, Vandenberg SR, Morhardt DR and Fike JR (2004) Radiation-induced impairment of hippocampal neurogenesis is associated with cognitive deficits in young mice. Exp. Neurol. 188: 316–330.
Sleeper E, Tamm C, Frisen J, Zhivotovsky B, Orrenius S and Ceccatelli S (2002) Cell death in adult neural stem cells. Cell Death Differ. 9: 1377–1378.
Acknowledgements
We would like to thank Dr. Steven L Carroll for helpful discussions regarding real time RT-PCR techniques, Dr. John J Shacka for critical review of this manuscript, and Ms. Cecelia B Latham for technical assistance. This work was supported by grants from the National Institutes of Health (NS35107 and NS41962). RSA is supported by the UAB Medical Scientist Training Program (GM008361). The nestin antibody developed by Susan Hockfield was obtained from the Developmental Studies Hybridoma Bank developed under the auspices of the NICHD and maintained by The University of Iowa, Department of Biological Sciences, Iowa City, IA 52242, USA.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by V De Laurenzi
Rights and permissions
About this article
Cite this article
Akhtar, R., Geng, Y., Klocke, B. et al. Neural precursor cells possess multiple p53-dependent apoptotic pathways. Cell Death Differ 13, 1727–1739 (2006). https://doi.org/10.1038/sj.cdd.4401879
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401879
Keywords
This article is cited by
-
BH3-only proteins BIM and PUMA in the regulation of survival and neuronal differentiation of newly generated cells in the adult mouse hippocampus
Cell Death & Disease (2010)
-
Bax is upregulated by p53 signal pathway in the SPE B-induced apoptosis
Molecular and Cellular Biochemistry (2010)
-
Acute neonatal glucocorticoid exposure produces selective and rapid cerebellar neural progenitor cell apoptotic death
Cell Death & Differentiation (2008)
-
Bcl-2 family and the central nervous system: from rheostat to real complex
Cell Death & Differentiation (2006)